In Australia there are four state-based poisons information centres (PICs), one each in Queensland, New South Wales, Victoria and Western Australia, that together provide a 24-hour Australia-wide service.
The PICs are staffed by specialists in poisons information (SPIs). Most SPIs are pharmacists who have undergone further training in toxicology and the provision of poisons information. SPIs are supported by clinical toxicologists, who advise on the more serious cases of poisoning.
In 2022, the Qld PIC answered approximately 30,500 calls regarding exposure to poisons. Of these calls, 1.5% (453) were received from general practice, and a further 2.6% (809) of callers were referred by the PIC to their GP for medical assessment (Qld PIC, unpubl. data, 2022).
The PIC receives calls covering a wide spectrum of incidents, ranging from a child with non-intentional ingestion of sink detergent to a critically ill patient following snake envenomation or to a patient with intentional ingestion of poison for purposes of self-harm. In 2022, 53.5% (16,336) of exposure cases were non-intentional accidental exposures, 17.9% (5482) were inadvertent therapeutic errors and 12.7% (3869) were intentional exposures for the purposes of self-harm (Qld PIC, unpubl. data, 2022).
This article describes some of the common calls the Qld PIC receives from general practice and provides information about how best to manage these cases. In 2022, calls received from general practice most commonly included exposures to paracetamol and household cleaning products (Table 1). Ingestion was the most common route of exposure, accounting for 54% (328) of calls, followed by ocular exposure, accounting for 14% (87) of calls (Figure 1).
| Table 1. Substances most frequently cited in 453 exposure calls from general practices to the Queensland Poisons Information Centre in 2022 (Qld PIC, unpubl. data, 2022) |
| Substance type |
No. exposuresA |
Proportion of exposure substancesB (%) |
Most common substance in this classA,C |
| Household cleaning product |
57 |
9.4 |
Cleaner: all-purpose/hard surface (9) |
| Paracetamol-containing analgesics |
47 |
7.7 |
Paracetamol immediate-release preparations (41) |
| Bites/stings |
32 |
5.3 |
Spiders (9) |
| Cardiovascular agents |
31 |
5.1 |
Ramipril (4), bisoprolol (4), atorvastatin (4) |
| Cosmetics and personal care products |
33 |
5.4 |
Hand sanitiser (7) |
| Chemicals |
23 |
3.7 |
Acids (11) |
| Hydrocarbons |
21 |
3.4 |
Petrol (9) |
| Antidepressants |
19 |
3.1 |
Mirtazapine (4), escitalopram (4) |
| Pesticides |
18 |
3.0 |
Pyrethrins/pyrethroids (8) |
| Building/handyman products |
18 |
3.0 |
Paint (11) |
AAn individual exposure call may involve more than one substance and/or more than one route of exposure. Exposure substances are counted for each route of exposure.
BThe total number of exposure substances was 607.
CThe number in parentheses reflects the number of calls received about these substances. |
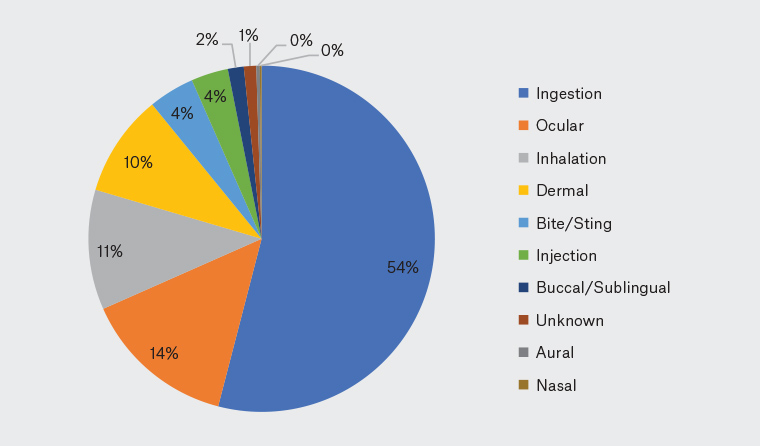
Figure 1. Route of exposure in 453 exposure calls from general practice to the Queensland Poisons Information Centre in 2022 (Qld PIC, unpubl. data, 2022)
In any poisoning situation, a risk assessment-based approach is recommended.1 Following any immediate resuscitation measures, a thorough risk assessment is undertaken. This risk assessment considers details of the product involved, an assessment of the dose or degree of exposure, the time frame and the current clinical status of the patient. Patient details, including medical and medication history, age and weight, are also considered, as are results from any investigations.
The management advice in this article is of a general nature and should be taken in the context of a thorough risk assessment. Further information on risk assessments for poisoning can be found in the Toxicology and Toxinology section published by Therapeutic Guidelines.2
Common poisoning scenarios
Paracetamol poisoning
Paracetamol poisoning is one of the most common calls to the PICs.3 The major risk from paracetamol poisoning is acute liver toxicity. Paracetamol poisoning scenarios encountered by GPs include inadvertent repeated supratherapeutic ingestions, non-intentional paediatric exposures and acute intentional self-poisonings.
Repeated supratherapeutic ingestions
Repeated supratherapeutic ingestions occur when a patient inadvertently takes more than the recommended maximum daily dose, often for a number of days. In children, this may occur when an incorrect dose is administered repeatedly or when multiple products of different strengths or brands are inadvertently given repeatedly.
In patients who have ingested a dose of paracetamol that puts them at risk of liver injury (Box 1), a blood test is required to check the paracetamol concentration and to assess liver function, specifically looking at alanine aminotransferase (ALT). If the paracetamol concentration is greater than 20 mg/L or ALT is greater than 50 U/L, then treatment with N-acetylcysteine (NAC) is required.4
| Box 1. Repeated supratherapeutic paracetamol dosing that may be associated with acute liver injuryA |
≥10 g or ≥200 mg/kg (whichever is less) over a single 24-hour period
Or
≥12 g or ≥300 mg/kg (whichever is less) over a single 48-hour period
Or
A daily therapeutic dose or greater per day for more than 48 hours in patients who also have abdominal pain or nausea or vomiting |
| AAdapted from Chiew et al, with permission by the Medical Journal of Australasia.4 |
Some individuals are at greater risk of toxicity than others due to advanced age, comorbidities, alcohol use, nutritional status (eg prolonged fasting), concurrent medications or genetic predisposition.5 Therefore, the threshold for a potentially toxic dose of paracetamol has been made deliberately and conservatively low to account for these risks.4
Patients who have inadvertently taken more than a daily therapeutic dose of paracetamol but are below this toxic threshold and are asymptomatic can be reassured that the ingestion is not expected to cause toxicity and educated regarding the safe dosing of paracetamol.
Unintentional paediatric paracetamol ingestion
Unintentional paediatric paracetamol exposure occurs commonly in young children (age <6 years) and may occur when paracetamol-containing tablets or liquids are accessed and ingested. In these instances, it may be difficult to ascertain the exact dose taken, so a worst-case scenario should always be assumed, based on the number of tablets or amount of liquid missing. Other common scenarios include when one caregiver administers a paracetamol dose at a similar time to another, or in situations where multiple products of different strengths or brands are accidentally administered.
An acute ingestion of ≥200 mg/kg paracetamol may be associated with acute liver injury and the child should be referred to hospital for blood tests and assessment.4 The paracetamol treatment nomogram (Rumack–Matthew nomogram) is used to determine the need for treatment with NAC when there is a known time of ingestion of an immediate-release paracetamol product, using the paracetamol concentration in the blood.6
Carers of asymptomatic children who have ingested <200 mg/kg paracetamol, including any therapeutic doses, in a 24-hour period can be reassured that the ingestion is not expected to cause toxicity and be advised to avoid further dosing of paracetamol for a period of time depending on the dose ingested, up to 24 hours.
Acute intentional self-poisoning
Acute intentional self-poisoning with paracetamol may include ingestion at a single time point or multiple or staggered ingestions for the purpose of self-harm. Acute single ingestions of ≥10 g paracetamol may be associated with liver injury.4 However, referral to hospital for the measurement of the serum paracetamol concentration is advised for all intentional self-poisoning presentations to assess the need for NAC, regardless of the stated dose.4
There is an increased risk of severe liver toxicity and death in patients who present late (>8 hours) after a paracetamol overdose, in those who take very large overdoses (>30 g) and when a modified-release paracetamol preparation is ingested.7
For any paracetamol poisoning scenario, if treatment has not been required, patients should be advised that if they develop abdominal pain, nausea or vomiting, then further assessment is required. Risk assessment and the management of poisoning differs between modified-release paracetamol and immediate-release paracetamol and is beyond the scope of this paper. The PIC can be contacted for advice in these cases and additional management advice regarding paracetamol poisoning can be found in the Updated guidelines for the management of paracetamol poisoning in Australia and New Zealand.4
Exposure to household cleaning products
Household cleaning products include substances such as surface or multipurpose cleaning sprays, bleach, dishwasher tablets, dishwashing detergents, disinfectants, laundry detergents, liquid toilet bowl cleaners and toilet rim blocks. Most commonly, these products are accessed by toddlers and accidentally ingested in small quantities. Symptoms are usually mild and may include mucosal irritation, vomiting or diarrhoea. In many of these cases, if the child has remained asymptomatic since the time of ingestion and is able to tolerate oral fluid and foods, it may be suitable for them to be observed at home with the carer to be educated on ‘red flag’ symptoms that would warrant referral to hospital. The PIC can be consulted to aid in this risk assessment. Symptomatic children (Box 2) should be referred to hospital for further observation and management.
| Box 2. Symptoms of corrosive injury9 |
Painful and burning sensations in the mouth and throat
Retrosternal chest and upper abdominal pain
Nausea
Vomiting, often with haematemesis
Hypersalivation
Difficulty swallowing secondary to oedema
Ulcerations or whitish-appearing plaques in the mouth, oropharynx or on the palate
Laryngospasm
Dysphonia/aphonia
Dyspnoea |
However, intentional consumption of large quantities or exposure to concentrated household products can lead to more serious complications, even death.8 Products that convey a higher risk of corrosive injuries include oven and drain cleaners, concentrated disinfectants and laundry hygiene rinses. Oven and drain cleaners often contain sodium hydroxide or potassium hydroxide and are highly alkaline (pH > 12). Concentrated disinfectants and laundry hygiene rinses contain high-strength cationic detergents such as benzalkonium chloride, which is a quaternary ammonium compound.
The severity of corrosive injury depends on the chemical concentration and the strength (eg pH for acids and alkalis or oxidative potential) of the product. More viscous substances may increase the severity of chemical injury because they may adhere to the wall of the gastrointestinal tract, increasing contact duration.9
Ocular exposure
In 2022, ocular exposure to poisons accounted for approximately 14% (87) of calls from general practice to the Qld PIC (Figure 1). Some of the commonly involved substances are pool products, plant saps (particularly plants in the Euphorbiaceae family) and hand sanitisers.
Exposure to pool products
Exposure to pool products commonly occurs in the home environment, when chemicals are added to domestic swimming pools. Pool chlorine is available in liquid, granular and tablet form and generally contains concentrated sodium or calcium hypochlorite. These products are highly alkaline and can cause significant corrosive injuries. Pool acids usually contain concentrated hydrochloric acid and can also cause serious eye injuries.
Exposure to Euphorbiaceae plants
All species of the Euphorbiaceae family of plants produce a milky-white, latex-like sap that is a strong ocular irritant.10 Euphorbiaceae are one of the more common species involved in plant poisonings reported to the Qld PIC and ocular exposure to the sap of Euphorbiaceae is the main reason medical referral is advised following plant exposure.11
One of the more common plants in the Euphorbiaceae family is the naked lady or firestick plant (Euphorbia tirucalli; Figure 2).12 Eye exposure to this plant can occur when pruning or removing the plant. Immediate symptoms of burning or stinging pain with blurred vision and local swelling have been described.10 Cases treated soon after injury typically have a good outcome, whereas delayed treatment may lead to complications such as corneal scarring and decreased visual acuity.10

Figure 2. Euphorbia tirucalli.
Reproduced with permission from Forest and Kim Starr.12
Exposure to hand sanitisers
The widespread use of hand sanitisers since the beginning of the COVID-19 pandemic has been associated with an increase in non-intentional exposure, especially in children.13 Calls to the Victorian PIC regarding ocular exposure to topical antiseptics more than doubled from 2019 to 2020.14 The composition of hand sanitisers can vary, but they generally contain at least 60% ethanol. Hand sanitisers are irritating to the eye but are not expected to cause permanent damage; however, corneal lesions have been reported overseas.13
Management of ocular exposure
First aid for ocular exposure primarily involves immediate irrigation of the eyes to remove the offending agent and to minimise potential injury. Prognosis is closely related to the effectiveness of immediate treatment measures.15 Immediate irrigation of the eye(s) for 30 minutes is recommended, before a full examination of the affected eye(s) can be performed. Analgesia and local anaesthetic eye drops may be required to aid irrigation and examination if there is associated pain.
If any particles remain in the eye, they should be removed from the ocular surface by everting the upper and lower eyelids and sweeping the ocular surface with a soaked cotton tip. If the exposure involves an alkaline or acidic substance, it is recommended that the pH of the eye is checked following irrigation. Further irrigation is recommended if the pH falls outside the normal range (6.5–7.4). Full examination of the eye, with assessment of visual acuity, fluorescein staining and a slit-lamp microscope, is recommended following exposure to corrosive agents and, if any injury is detected, referral for specialist ophthalmological assessment should be considered.16
Conclusion
When managing a poisoning exposure, a thorough risk assessment, including details of the product, the dose, the time since exposure and patient factors (eg current clinical status) and medical history is vital. In 2022, GPs commonly called the Qld PIC regarding cases of paracetamol poisoning and ingestion of household cleaning products, with ocular exposure being common. Many such cases can be managed in general practice. The PIC can help GPs with risk assessment and provide management advice regarding exposures to medicines, drugs of abuse, household and garden products, agricultural and industrial chemicals, plants and fungi, as well as bites and stings.
Key points
- The PIC can be contacted 24 hours a day by members of the public and health professionals by telephone on 13 11 26.
- The PIC can help GPs with risk assessment and provide management advice regarding exposures to medicines, drugs of abuse, household and garden products, agricultural and industrial chemicals, plants and fungi, as well as bites and stings.
- When calling the PIC, having accurate details of the product involved, the dose or degree of exposure, the time frame, the current clinical status of the patient and any relevant medical history will allow for an accurate risk assessment.
- GPs commonly call the PIC regarding cases of paracetamol poisoning and ingestion of household cleaning products, many of which can be managed in general practice.
- Ocular exposure to poisons requires irrigation, examination and occasionally referral for specialist ophthalmological assessment. Early adequate irrigation is important in preventing permanent harm.