Initially, general practice looks uncomplicated – until you try to do it and try to do it well.
– Chris Hogan
For too long, general practice has been demeaned and oversimplified by non-general practitioner (GP) colleagues, as well as members of the community and politicians.1 This, in part, is explainable by the difficulties in adequately depicting and/or describing the complexity of the discipline of general practice.
The foundation of general practice has been well outlined,2–4 as has its benefits to patients, communities and the health system at large.5–10 Many, including The Royal Australian College of General Practitioners (RACGP), have attempted to succinctly summarise the values and activities of general practice for its members and our patients into a memorable phrase, but no one has yet succeeded.
It is imperative that general practice and generalism is understood to be completely different to hospital-based care and it is this issue of ontology and epistemology that needs to be addressed for policy makers and clinicians alike.
The authors have used the vortex metaphor of health and the health system to depict the complex work of general practice and GPs. Box 1 highlights the underlying systemic challenges, problems and common policy issues.11 Figure 1 shows how the profession can contribute to improving the health of individuals and communities by influencing and directly acting at every level of the health system.
| Box 1. Assumptions that contribute to system failure |
- Governments seeing health as a cost to be controlled rather than an investment in the productivity of the nation.12–14
- Politicians and bureaucrats believing that fixing any (whatever the current biggest) failing part of the healthcare system will ‘cure the system’ despite the well-established fact that fixing parts will not improve any system as a whole, and is therefore a waste of time and effort.15–17
- General practice is the place that can deal with anything that no one else is interested in or capable of within the constraints of its resources.
- General practice is too difficult, too demanding and too unrewarding is a view promulgated tacitly and at times explicitly in undergraduate and early postgraduate settings.
- General practice is strained to breaking point with increasing demands while its ageing workforce is rapidly declining.18
- Politicians promote our healthcare system as the best in the world and able to cope even under peak demand. Yet hospitals frequently have bed blocks resulting in prolonged ambulance ramping. General practices have increasing waiting times for appointments.
|
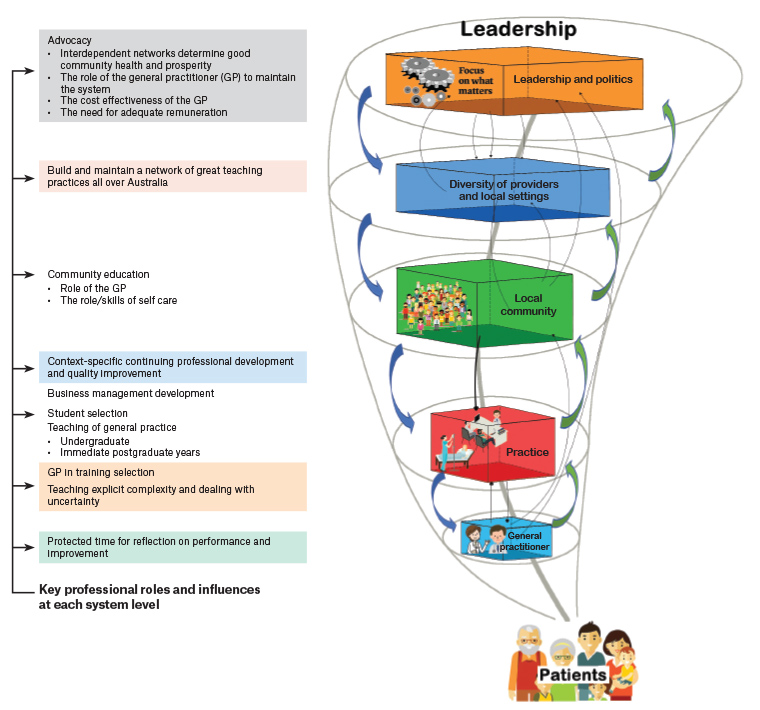
Figure 1. Key professional roles and influences at each system level. For the profession to effectively exert its influences on the health system design and function, it must appreciate its direct (coloured boxes) and indirect (advocacy, grey box) roles at different system levels. Click here to enlarge.
Complex adaptive dynamics of health and healthcare
Before some systemic solutions can be proposed to address the challenges facing general practice, it is necessary to briefly:
- re-evaluate our understanding of health and illness
- re-evaluate the distribution of health and illness in the community
- emphasise the challenges of managing ill-defined illnesses and chronic complex multimorbidity
- highlight the health and economic benefits of generalist care.
Health, rather than being an objective state, is a subjective state determined by the balance between one’s physical, emotional, social and sense-making domains that define the systemic somato-psycho-socio-semiotic (SPSS) model of health.19,20 In addition, health at a population level is patterned, with each pattern emerging at the interface between the external environment and the biological blueprint (Figure 2).21
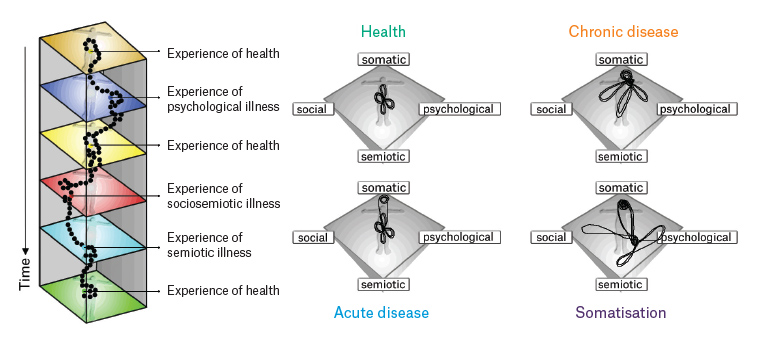
Figure 2. The complex dynamic patterns of health and disease. Appreciating the dynamics of health and disease guides the generalist approach to managing a patient’s illness in contrast to the guideline and protocol driven ‘single disease’ approach to management.
Non-linear distribution of care needs and disease distributions
White et al first demonstrated that the experience of health and the need for healthcare follow a Pareto distribution.22 That is:
- 80% of the community is healthy or healthy enough not to require care from a health professional
- Of the 20% requiring care from a health professional, 80% (ie 16% of the total community) will only require primary healthcare
- Of the 20% (ie 4% of the total community) requiring further care, 80% (ie 3.2% of the total community) will require secondary care and 20% (ie 0.8% of the total community) will require tertiary care (Figure 3A).
Equally, general practice also follows a Pareto distribution:
- 80% of all patient consultations end without a definite diagnosis
- 80% of all patients will have one of the 20% of all possible diagnoses (the common conditions)
- The remaining 20% will have one of the remaining 80% of all possible diagnoses (the uncommon conditions not to be missed, and more commonly managed by their respective non-GP speciality clinician) (Figure 3B).23,24
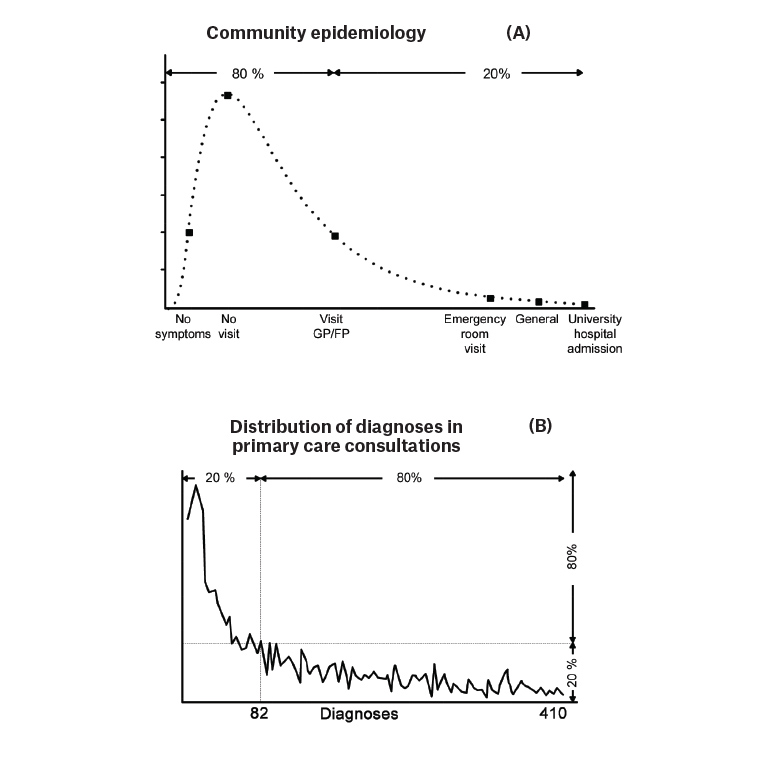
Figure 3. The 80/20 split of the distribution of care needs and disease. (A) 80% of the community is healthy or healthy enough not to require health professional care. Of the 20% seeking care, 80% require GP care, of the remaining 20%, 80% require secondary care, the other 20% tertiary hospital care.22 (B) 80% of all GP consultations deal with the 20% of the most common diseases, whereas specialists deal with 80% of uncommon diseases.
Based on: White – The Ecology of Primary Care Consultations22 and Die gezielte Diagnostik in der Praxis. Stuttgart: Schattauer; 1957.
FP, family physician; GP, general practitioner.
Challenges of successfully managing ill-defined illness and complex multimorbidity
In contrast to well-defined guideline- and protocol-driven disease-specific care, most GP work deals with either poorly definable illness experiences25,26 or chronic complex multimorbidity.27
Neither of these problem complexes are amenable to standardised guideline- or protocol-based approaches which have been developed for the management of single conditions. There are just a handful of guidelines for patients who experience two comorbidities,28–30 and only the guideline for deprescribing is applicable to people with five or more comorbidities.31
The success of general practice care depends as much on the generalist approach32 as on the ability to establish a therapeutic relationship with one’s patients.33–35 Being person-centred is key to the development of relational continuity which, in turn, allows the emergence of a deep contextual understanding about a patient’s personal circumstances and preferences.36,37
Health and economic benefits of generalist care
Person-centred care is demanding and time consuming,27,38,39 and more complex than specialist care.40 It is equally effective as disease specialist care for common chronic conditions,41,42 and, most importantly, more cost effective.42,43 The quality and benefits of generalist care therefore requires specific patient-centred outcome measures such as the ability to cope44 and quality of life.45 In addition, good general practice care achieves healthier people independent of the level of morbidity, geography and socioeconomic disadvantage.46,47
Gaining the required knowledge and skills for general practice
Unsurprisingly, general practice is the most challenging discipline in medicine as it operates in the realm of complexity and uncertainty.48–51 This requires aptitude and emotional coping skills to become a resilient clinician,48,50 a point that needs to be considered seriously when selecting and training medical students. In addition, medical students require more and earlier exposure to general practice to understand what it means to be ill, and to appreciate the needs of people with and without disease aligning with the Pareto distribution of care needs (Figure 4). Only then will they develop the essential aptitude and emotional coping skills to be an effective physician. This change in medical education would honour Osler’s dictum: It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.52
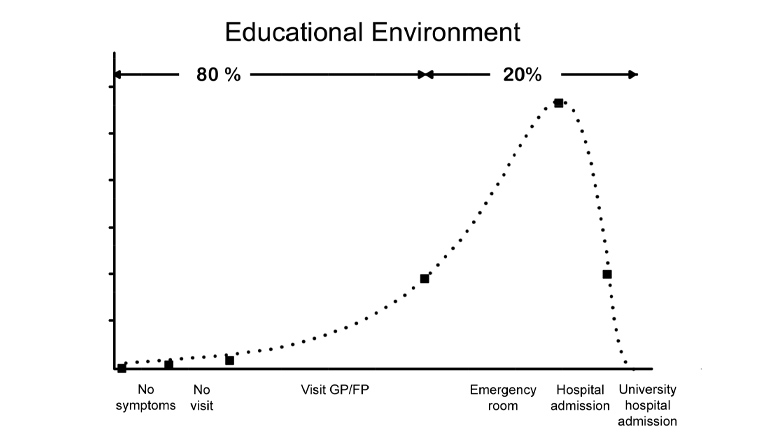
Figure 4. Medical education should reflect the ecology of health and illness. Medical education predominantly occurs in the tertiary hospital system. This approach fails students in experiencing the great variability of health, illness and disease, and developing the necessary aptitudes and coping skills of becoming a resilient clinician. It reinforces the ‘inverse needs law’ of patient need, reinforcing the fallacy that only specialists and hospitals provide ‘useful care’.
FP, family physician; GP, general practitioner.
Knowledge and skills development
In general terms, GP knowledge and skills across all domains expand over a GP’s career, from final-year medical student to GP in training, to competent unsupervised general practice, through to advanced general practice. This contrasts with non-GP specialists who expand their knowledge and skills in a particular domain while at the same time no longer maintain their knowledge and skills in most other domains. While some GPs might want to develop specific interests in a particular domain – often in response to their practice population needs – they apply those skills within the generalism framework of general practice (Figure 5).
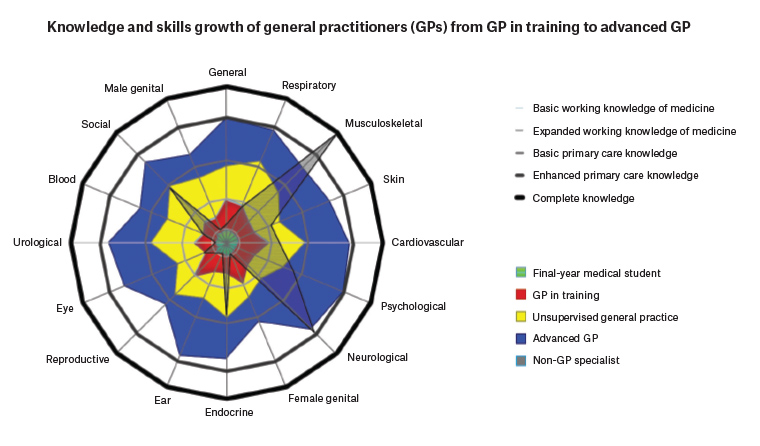
Figure 5. Contrasting knowledge and skills development between general practitioners and non-GP specialists. General practice skills grow from student to senior GP across all domains. Non-GP specialists have a narrow but greater in-depth knowledge and skills set focused on their particular discipline.
From competence to capable
There is an urgent need to rework the concept of competence away from the legalistic understanding of ‘specialist expertise’. Competence arises from the interactions of three domains: skills mix, clinical significance and performance.53 No one, including ‘specialists’, will be 100% competent in each of the three domains, and a weakness in one domain under one circumstance can be compensated for by a strength in the other two.53 Being able to successfully apply one’s mix of competencies in the context of varying patient needs and demands results in being capable to practice safely and effectively (ie doing the best one can do in the current context).54
Capability entails being able to apply one’s learnings to new situations.55,56 Capabilities emerge from continuing learning and unlearning, modification and integration of new knowledge as time progresses through one’s career. This process is described as developing mindlines, which are an important collection of complex knowledge sources that are tested and refined within the social, emotional, physical and cultural milieu of both physician and patient.57,58
From capable to mastery
Mastery is defined subjectively as attaining comprehensive knowledge and skills in a particular discipline with a feeling of confidence in one’s abilities. It is defined objectively as the ability to deliver an authentic and worthy performance. Those who have achieved mastery are fluent, even creative, in using their knowledge, skills and understanding in key performance challenges and contexts. It usually takes several years after obtaining fellowship qualifications to reach the validated high-level standards of mastery level performance. Confidence in how a person practises includes knowing how to test and refine knowledge in the face of new challenges and unexpected patient presentations.56
It is therefore important to view ongoing professional development in the light of one’s practice characteristics (ie geography, social environment and patient profile), which, in turn, determines one’s required knowledge, skills and capabilities.59 The most effective and efficient way for GPs to achieve mastery is a local community-based, peer-supported network (aka community of practice) that provides a safe peer learning environment in which to explore the interdependencies between patients’ health, illness and disease care needs within an inevitably constrained health system.60
Advocating for health system improvements
The issues discussed above are largely under the direct control and influence of general practice organisations, whereas their role in terms of health policy is largely limited to advocacy. Policy makers need to understand the systemic nature of health, illness, disease, care delivery and care outcomes; they also need to appreciate the Pareto distribution of health, illness and disease and its implication for resourcing in terms of the required healthcare infrastructure as well as its workforce size and composition.
Most importantly, policy makers must realise that health, illness and disease care outcomes are primarily determined by interrelated network interactions across all scales of societal organisation. These interactions and interdependencies may entail greater investment into social and community development,61,62 rather than ‘throwing more money’ (such as in the context of residential aged care, www.health.gov.au/resources/publications/budget-2021-22-budget-at-a-glance?language=en) aiming to sort out some politically pressing ‘community issues’.15
Last, there remains the urgent but unresolved issue of providing services equitably, which entails the urgent need of addressing workforce shortages and maldistribution.
A vision to make general practice colleges seamlessly integrated organisations
This article, and the authors’ previous contribution,11 outlined the characteristics of a complex adaptive organisation and documented key interdependencies within the general practice system, which entails diverse agents with different perspectives and responsibilities. For the system to achieve its purpose and meet the needs of patients, each agent within the system must carefully evaluate its role and impact on the system as a whole.
The authors, active members of the RACGP, suggest that it should adopt a systems and complexity thinking approach and redefine its purpose/focus, specific goals, core values and core operating rules.
Purpose/focus
The purpose or focus of the RACGP is to help its members to meet the needs of their patients. This could be articulated as ‘We enable members to deliver the care that meets their patients’ needs’. Being able to deliver requires every member at every level within the organisation to align their work accordingly.
Specific goals
Specific goals generally relate to the most pressing issues that need to be addressed within the short to medium timeframe. Most organisations focus on no more than a handful of goals. The authors suggest that medical colleges responsible for general practice should address the following specific goals arising from its purpose to enable members to deliver the care that meets their patients’ needs:
- Implement a teaching unit that enables GPs to apply complexity understandings of health and disease to the generalist approach of patient care.
- Revise all educational activities based on heutagogical principles55,56 to build competencies and capabilities for context-sensitive generalist care.
- Implement the assessment-based learning framework of skills development across the career trajectory.59
- Establish an advocacy agency consisting of health professionals, community leaders and patient representatives charged to highlight the systemic deficiencies in primary care to the public and policy makers.
- Re-establish local and regional GP networks that provide interprofessional support and assist in the equitable distribution of scarce resources.
- Involve and engage interested medical students with all of the above goals, including observership on the college boards.
Core values
Core values refer to those that remain unchanged in a changing environment. These would be:
- colleague-centred problem solving
- patient/person-centred healing relationship
- context-driven adaptive learning
- being agents of progress.
Core operating rules
Core (or simple) operating rules define how we interact internally and with our external stakeholders. Simple rules consistent with the purpose and goals of a general practice college might be:
- Adapt to expected and unexpected eventualities.
- Do the least harm possible.
- To care with skill (Cum Scientia Caritas).
- Or more contemporarily: To cure sometimes, to relieve often and to comfort always (Osler).52
- Promote the value/benefits of general practice care to patients and policy makers.
- Reiterate that quality care requires quality resourcing.
A way forward
The authors have aimed to ‘untangle’ the core complexities of general practice using a system and complexity-thinking framework.11 How GPs approach their work to enhance the wellbeing of patients relies on appreciating the interconnectedness and interdependencies involved when people seek healthcare; this means treating individuals who experience illness in the presence as much as the absence of identifiable diseases, understanding the impact of the nature of their community on their health, as well as developing a relationship with the wider health service network.
The effectiveness of the RACGP as well as other general practice organisations depends on embracing the core principles of a seamless horizontally and vertically integrated complex adaptive (also referred to as ‘learning’) organisation.63 Members of any GP organisation want to have an effective organisation that will help them to enhance their work in their local setting. From a complexity standpoint, the purpose, goals, values and simple rules for general practice suggested above are based on the sciences underpinning the profession.
The authors believe the approaches and perspectives discussed would allow GP organisations to emerge into truly integrated learning organisations. Embracing leadership approaches to manage the complex adaptive nature of general practice could help to empower GPs to define the interconnected and interdependent nature of their work, and to assert their irreplaceable role and expert skills to manage the complexities of health, illness and disease.