In its 2019 position statement, The Royal Australian College of General Practitioners (RACGP) recognises climate change as a key public health issue and articulates the important role that general practitioners (GPs) play in mitigation and adaptation strategies.1
To limit global warming to 1.5°C, the Climate Council has called for Australia to reach net zero emissions by 2035, with a 75% reduction by 2030.2 This requires an enormous transformational change through every sector of the community, including health.
General practice can demonstrate leadership by being an agent of change, understanding that sustainability is part of primary care’s ethos as it aligns with quality care, continuity of care and preventative care. From the waiting room and consulting space through to the broader community, GPs have an important role in environmental health advocacy that supports our physical and mental health.
Achieving sustainability requires not just a consideration of energy use or waste, but also a fundamental re-evaluation of the purpose and practice of medicine, including a greater focus on prevention.
A planetary health perspective requires us to recognise our connectedness to and dependence on the health of nature. It demands a change to models of healthcare that are sustainable, prioritise prevention and are inclusive of the social and environmental dimensions to health.
Non-clinical emissions
The healthcare sector in Australia is estimated to contribute 7% of Australia’s total carbon emissions. General practice accounts for 4% of the health sector’s total, excluding emissions from pharmaceuticals (Figure 1).3 However, these figures are derived from economic models and assumed carbon costs within healthcare expenditure. There are few data of onsite emissions from either Australian hospitals or general practice.
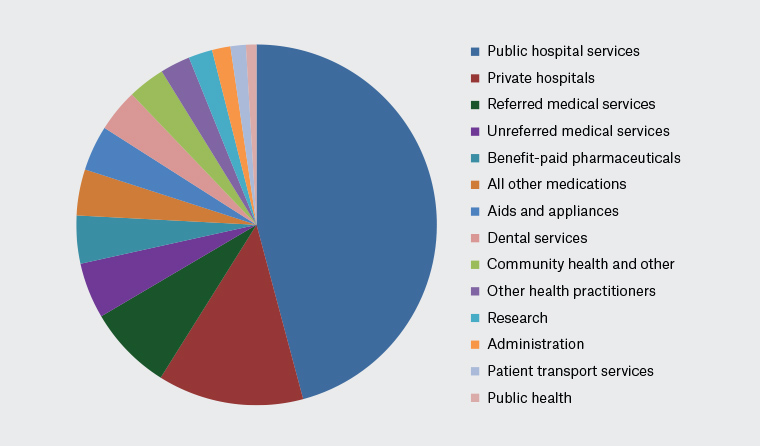
Figure 1. Total and relative CO2 equivalent emissions for 13 healthcare expenditure categories in the Australian healthcare system.
Reproduced from Malik et al,3 with the permission of Forbes McGain.
Although the non-clinical carbon footprint of practices is relatively small, as role models we should embed advocacy within all aspects of practice operations.
Sustainability is not just a series of tick boxes, but rather involves strong leadership, education and cultural change within the workplace, bringing colleagues and staff on the journey. Appointing a ‘climate champion’ or ‘green team’ and having regular reviews of interim targets supports the process of change.
In a world moving to net zero, carbon becomes an obligatory metric and carbon literacy an imperative. To integrate sustainability into practice operations, it is necessary to perform an audit of the practice’s carbon emissions to set a benchmark and a basis for future monitoring. There are numerous online carbon calculators that can provide guidance.
UK data have shown that energy use and staff travel are the main modifiable areas in general practice (Figure 2).4 Emissions from both staff and patient travel in Australia may vary considerably depending on practice location.
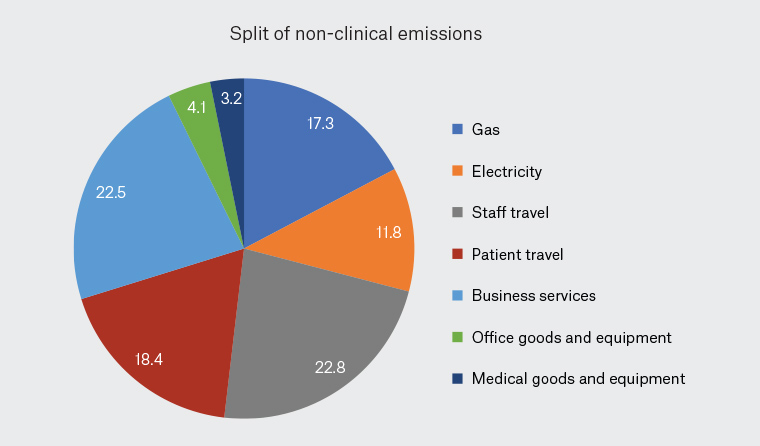
Figure 2. Carbon footprint of general practices across the Humber and North Yorkshire Integrated Care System region.
Reproduced from Sawyer and Thrower,4 with the permission of Matthew Sawyer.
Avoiding energy use and improving efficiency saves both carbon and money. The key areas to focus on are heating/cooling, appliances and lighting. Installing rooftop solar, if possible, is cost-effective, with the payback period in Australia as short as 3 years.5 Purchasing renewable energy5 is an easy and quick action that immediately reduces emissions and sends a clear signal to the energy market.
Energy expenditure from staff and patient travel can be reduced by promoting active or public transport with health co-benefits from exercise and reduced air pollution. The appropriate use of telehealth for patients and allowing practitioners and staff to work from home provides another avenue for action.
Sustainability should be part of a practice’s business plan. Potential costs and benefits to each action need to be considered. With limits to how much one can reduce a practice’s footprint, purchasing carbon offsets is an option to help move to net zero emissions. Many companies offer offsets with a range of validation and verification standards. Offsets are not equivalent to genuine emission reductions, but they do put a price on carbon, placing it clearly on the balance sheet. As a practice progressively decarbonises, this should also be reflected in a reduced need for offsets.
Resources to support reductions in non-clinical emissions are provided in Box 1.
| Box 1. Resources to support reductions in non-clinical emissions |
- The RACGP has a new factsheet with practical tips and advice on environmental sustainability in general practice22
- The RCGP have an e-learning resource, RCGP NetZero: Decarbonising general practice, your guide to a Net-zero action plan for non-clinical emissions23
|
Clinical emissions
Beyond practice operations, estimates of the carbon footprint in general practice in the UK suggest that approximately 50% are associated with pharmaceutical prescribing,6 whereas recent Australian data suggest that pathology testing and diagnostic imaging contribute to 9% of healthcare’s carbon footprint.7 The bulk of general practice emissions lie within prescribing and clinical practice.
Reducing waste
Health resources need to be valued. Every investigation ordered and every medication prescribed has a financial cost and a carbon footprint. With up to 40% of healthcare either of low value or detrimental,8 there is considerable waste in clinical practice. In the context of sustainability, avoiding costs, resource consumption and waste represents best practice.
As an example, recent analysis of the carbon footprint of five common hospital pathology tests (full blood examination; urea and electrolyte levels; coagulation profile; C-reactive protein concentration; and arterial blood gases) revealed that the carbon dioxide equivalent (CO2e) emissions ranged between 0.5 and 116 g CO2e, the same as driving a car between 3 m and 0.8 km.9 Millions of these tests are performed each year. Routinely ordering pathology tests unsupported by evidence is wasteful.
Similarly, reducing unnecessary radiological investigations10 and unnecessary non-GP specialist referrals or specialist interventions, such as surgery, can reduce waste and carbon footprint.
Non-evidence-based pharmaceutical use is a contributor to the carbon footprint of healthcare. Reviewing and ‘deprescribing’ medications may thus reduce impact. Although we have yet to determine the carbon footprint of most medications to enable us to select low-carbon options, metered dose inhalers are a known ‘carbon hotspot’. The propellants in these inhalers are potent greenhouse gases. Each puff of a reliever causes about as much warming as driving a conventional car for a mile. Many patients can be effectively switched to dry powder inhalers without adverse clinical outcomes.11,12 Resources to support reductions in clinical waste are provided in Box 2.
| Box 2. Resources to support reductions in clinical waste |
- The RACGP Handbook of Non-Drug Intervention (HANDI) is a good reminder of options to pharmaceutical prescribing24
- Primary Health Tasmania has an excellent resource on deprescribing25
- Resources such as Choosing Wisely Australia are helpful in offering a framework to reflect on quality clinical practice: https://www.choosingwisely.org.au/
- The Royal Australasian College of Physicians’ Evolve initiative provides recommendations regarding low-value care26
|
Low-carbon interventions
Choosing health interventions with low environmental impacts, such as lifestyle and psychosocial interventions before pharmacotherapy, where appropriate, supports both holistic and sustainable healthcare practice.
Poor diet is a major driver of the non-communicable disease epidemic. Food production accounts for approximately 30% of anthropogenic greenhouse emissions,13 70% of fresh water use and is the main cause of biodiversity loss. Switching to plant-based diets can halve greenhouse emissions, increase the mean Healthy Eating Index (a dietary index aligned with the recommendations of the Dietary Guidelines for Americans) by 8.7% and reduce diet costs by 10.5%.14
The Australasian Society of Lifestyle Medicine invites practitioners to consider innovation in clinical practice, such as shared medical appointments,15 to address some of the diseases associated with lifestyle and health inequity (eg smoking cessation, sleep and stress management, dietary and exercise interventions).
Social prescribing potentially offers another low-carbon intervention.16 One example is Parkrun, which are community-based, timed, 5-km events run by volunteers across Australia. The RACGP has recently partnered with Parkrun Australia, so general practices can be registered as Parkrun practices. A scoping review17 of Parkrun literature highlights that those participating in the events show improvements in fitness, total physical activity and mood (stress, anxiety, and depression).18 Resources to support low-carbon interventions are provided in Box 3.
| Box 3. Resources to support low-carbon interventions |
|
|
Clinical knowledge
The imperative to act on climate change and transition to sustainability must be founded on clinical knowledge and science. There are numerous pathways by which climate change affects human health, including direct effects (eg heatwaves, droughts, and extreme weather) and indirect effects (eg on air quality and water and food supply and quality). In addition, air pollution from fossil fuel combustion is a major cause of mortality and morbidity globally.
An initiative to begin GP registrar webinars has started in Victoria (Cassar et al, personal communication, 2021). The RACGP offers webinars and e-learning modules on environmental health with allocated continuing professional development points. Various primary health networks are working to integrate climate change into GP education updates.
Advocacy
With 80% of Australians visiting their GP at least once a year, primary care has an important role in advocacy. Doctors, as one of the most trusted professions, can be influential by being role models for change.
The practice ethos of sustainability can extend to the waiting room and throughout the practice, where it is reflected in all activities, from waiting room posters to the availability of bike racks to support active transport.
Choosing banks and investment schemes that include environmental impact criteria in their investment profiles is another avenue for advocacy. Resources to support advocacy are provided in Box 4.
| Box 4. Resources to support advocacy |
- The RACGP has several poster resources highlighting the health impacts of climate change and advocating for environmental sustainability22
- The Climate and Health Alliance has an excellent document about communicating the health impacts of climate change27
- Advocacy group Market Forces offer a bank comparison chart so you can find out which banks have a history of funding the fossil fuel industry and a similar chart for superannuation funds
|
Primary care within a sustainable healthcare system
General practice should be the cornerstone of a sustainable healthcare sector. Tertiary care is expensive and carbon intensive. The cost-effectiveness of primary care is well documented.19
The 2019 Western Australian Sustainable Health Review highlighted that without intervention, health spending was projected to approach 38% of the State budget by 2026–27.19 The current system is unsustainable across a range of metrics. With non-communicable chronic diseases (ie those shaped predominantly by lifestyles and broader social determinants) now responsible for the greatest burden of disease in Australia and elsewhere and accounting for up to 70% of all deaths globally,20 it is time to consider different models of care that are low carbon, low cost and more holistic.
The UK offers an example of community-based models of care within their integrated care systems. These partnerships bring together providers and commissioners of NHS services across a geographical area with local authorities and other local partners to collectively plan health and care services to meet the needs of their population.21 Although there are differences between the UK and Australian health systems, the idea of health services conceptualised within geographical communities linked to local councils and public health teams with a focus on prevention, health and wellbeing could be explored further in Australia, with primary health networks potentially playing a role. Primary care needs to be integrated into these new models, acknowledging the importance of the GP–patient relationship.
GPs operate within a biopsychosocial framework. Planetary health extends that to include the natural world, holistic care in its broadest terms. Urgent, society-wide changes must be made to avoid a climate crisis and to advance changes towards a fairer and healthier world. GPs should be at the forefront of the call for climate action and help build a planetary health system that acknowledges our interconnectedness and the principle of sustainability.
Key points
- As a practice owner, embed sustainability into your practice business model.
- Reduce emissions by encouraging active and public transport, as well as renewable energy.
- Food choices and healthy eating have benefits for both patients and the planet.
- Reduce low-value care, which includes unnecessary pharmaceuticals and investigations.
- Magnify your impact by sharing with patients; make your commitments visible.