It is also important to understand that pain is the sum of inputs to the brain associated with nociception, endocrinological and immunological function, and past experiences of pain and trauma within the sociocultural context in which the patient resides. The brain decides whether the output of pain will become a conscious experience depending on all these influences. This implies that any management of pain requires an assessment of all these areas.
The location of the neck pain can be used to make an assessment as to the likely segmental nociceptive origin. Pain in the upper half of the neck is usually from the upper cervical segments (C2–3 most commonly) and pain in the lower half of the neck is usually from the lower cervical segments (C5–6 most commonly). The approximate segmental location might be able to be determined if there is a localised pattern of pain radiation. Using cervical pain maps (Figures 1, 2) will help identify approximate segmental origin but not necessarily the structure, because discs, facets ligaments and muscles all have similar pain patterns.6,7
Cervical spine pain might be a signal of serious life-threatening disease (Table 2). Each consultation needs to visit the likelihood of a red flag condition being present, along with the appropriate investigations necessary to clarify possible diagnosis.
| Table 2. Red flags |
| Red flag |
Possible pathology |
Trauma (eg fall, MVA, diving accident)
Minimal trauma in osteoporotic patients, corticosteroid use |
Fracture/dislocation, ligament disruption leading to instability |
Constitutional symptoms (eg fever, weight loss, anorexia, meningism)
History of cancer, immunosuppression, intravenous drug use, recent surgery or instrumentation |
Metastatic tumour, spinal cord tumour, osteomyelitis, epidural abscess, discitis, meningitis |
| Rheumatoid arthritis, Down syndrome |
Atlanto-axial instability |
| Ripping, tearing sensation in the neck |
Vascular dissection (eg carotid, vertebral) |
| Concurrent chest pain, shortness of breath, diaphoresis |
Ischaemic heart disease |
| Worsening/persisting inflammatory pain, raised ESR/CRP |
Rheumatoid arthritis, seronegative spondyloarthritis, polymyalgia rheumatica |
| Torticollis |
Cervical dystonia |
| CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; MVA, motor vehicle accident. |
Taking a pain history involves exploring the different aspects of pain, in particular:
- nature: Neuropathic (including radicular pain) will require a different approach from nociceptive pain
- onset: Was there any trauma involved? If onset was sudden and spontaneous, then a closer search for red flag conditions is appropriate
- severity: If pain is severe and unremitting, then a serious condition should be suspected
- precipitating/aggravating factors: Identifying these features is important for future management. Extreme apprehension for neck movements raises suspicion of atlanto-axial instability, other instability or fracture. Pain after manipulation warrants consideration of a vascular cause
- relieving factors: Ask about previous treatments, medication and the response. If there are no relieving factors and the pain is constant and interfering with sleep, red flag conditions need review.
Assessment of yellow flags is paramount in any pain assessment. Yellow flags are a major driver of chronicity and, if not addressed, will minimise the chance of full recovery. Remediable determinants of chronicity include anxiety and depression, job stress and poor job satisfaction.8
Other factors associated with an increased risk of chronicity include initial high levels of pain/disability, female sex and older age. A two-question assessment for depression has been validated for primary care assessment of depression and can be incorporated into early assessment of patients with neck pain.9
Examination
A confident examination is an important part of assessment, especially to confirm whether the cervical spine is the likely nociceptive source. Reproducing the patient’s specific pain on examination of the cervical spine helps confirm the spine as the source, but does not necessarily help with a pathoanatomical diagnosis per se.
Inspection of the neck involves looking for torticollis, wasting of muscles, lumps, scars, skin lesions and colour changes. Movement of the neck, both active and passive, can be assessed. Upper cervical flexion can be assessed by a nodding movement. Upper cervical rotation (largely C1/2) is assessed by holding the above flexed position and turning right and left. Overall flexion/extension, rotation and lateral flexion, and whether it relieves or exacerbates the cervical pain, should be assessed.
Palpation might be performed prone, supine or sitting (Figure 3). The landmarks are:
- C2, the first palpable spinous process palpable below the occiput
- C7, the most prominent spinous process.
The facet joints might be palpated paracervically approximately one thumb breadth from the midline. Palpate generally feeling for:
- tenderness
- taught tender bands/spots in muscles (eg upper trapezius, sternocleidomastoid, scalene and paraspinal). The presence of tender bands/spots might indicate a role for massage or needle techniques
- skin drag, temperature and sensitivity (changes can occur with spinal sensitisation and autonomic dysfunction)
- segmental dysfunction, which involves more advanced palpation skills to identify irritable/stiff vertebral segments (eg C5/6 segmental dysfunction) and is used to identify appropriate manual therapy techniques.

Figure 3. Prone palpation of the cervical spine. Reproduced with permission from the Australian Association of Musculoskeletal Medicine.
Special tests can be used to provoke symptoms if necessary. The quadrant test10 involves slight extension, rotation and lateral flexion to the painful side. If this reproduces neck pain, then the cervical spine is the likely source of nociception. If it causes shooting pain into the arm, then radicular pain (a form of neuropathic pain from an irritated nerve root) is more likely.
Neurological examination should be undertaken if there are concerns of radiculopathy, myelopathy or central nervous system disorder. A description of neurological examination is beyond the remit of this article.
Investigations
The decision to investigate a patient with acute cervical spine pain is determined by the presence of red flags. If there has been trauma, then Canadian C-spine rules should be followed.11 A simplified version of the Canadian C-spine rules is shown in Figure 4.12
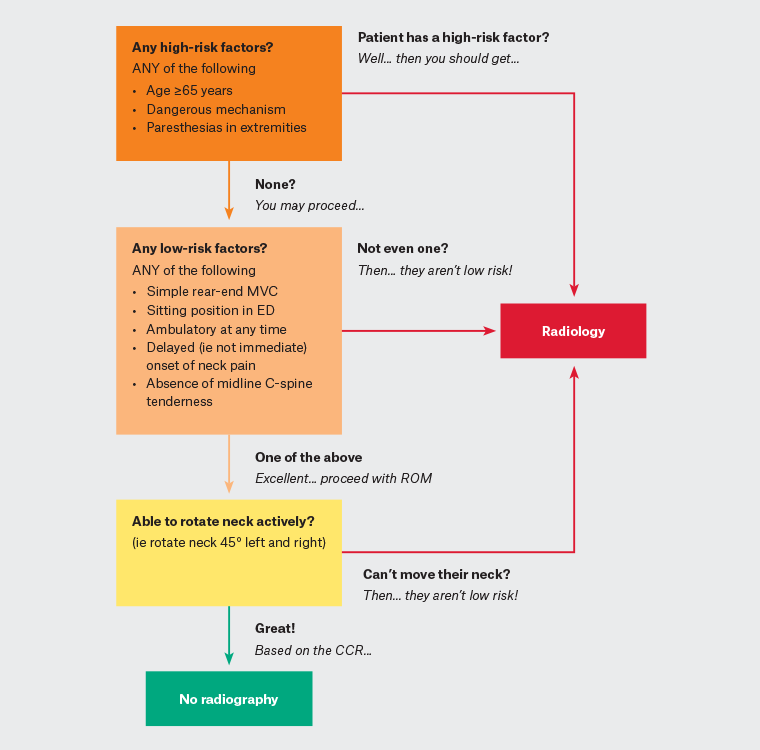
Figure 4. Modified Canadian C-spine rules.
CCR, Canadian C-spine rules; ED, emergency department; MVC, motor vehicle collision; Pt, patient; ROM, range of movement.
Blood tests might be used if there are concerns regarding polymyalgia rheumatica or a flare of inflammatory arthritis, osteomyelitis or other infections. A full blood count, differential count, erythrocyte sedimentation rate and C-reactive protein might be useful diagnostically. Isolated cervical spine is a rare presentation of inflammatory arthritis.
Diagnosis
For patients with acute cervical spine pain, a pathoanatomical diagnosis is usually not required in the absence of red flags. Yet, patients still require an understanding of what is causing their pain. For patients without any red flags and no trauma, acute cervical spine somatic dysfunction is a very good descriptive label. Somatic dysfunction is defined as impaired or altered function of related components of the somatic (body framework) system: Skeletal, arthrodial and myofascial structures, as well as related vascular, lymphatic, and neural elements.13
Cervicogenic headache is defined as pain that is perceived in the head that actually arises from the cervical region and is a form of cervical referred pain.14 Examination features of cervicogenic headache are:
- C1/2: Reduced flexion–rotation test
- C2/3 and C3/4: Simultaneous reduced cervical extension, segmental restriction plus pain and reduced craniocervical flexion test values.
If considering radiofrequency ablation, diagnosis can be confirmed by controlled third occipital nerve blocks.
People with recent trauma to their head and neck invite consideration of whiplash-associated disorder (WAD). The Quebec Task Force on Whiplash Associated Disorders classifies WAD based on the severity of a person’s symptoms and signs, as follows:15
- Grade 0: No complaints about neck pain; no physical signs
- Grade I: Neck complaint of pain, stiffness or tenderness only; no physical signs
- Grade II: Neck complaint and musculoskeletal signs including decreased range of motion and point tenderness
- Grade III: Neck complaint, musculoskeletal signs and neurological signs including decreased or absent deep tendon reflexes, muscle weakness and sensory deficits
- Grade IV: Neck complaint and fracture or dislocation.
For patients with WAD, the C2/3 and C5/6 zygapophyseal joints are by far the most common detectable nociceptive sources.16
Diagnoses such as cervical sprain strain are used commonly but lack any medical meaning, with somatic dysfunction a more useful description. Another term in common usage is ‘idiopathic neck pain’, meaning atraumatic neck pain not caused by an identifiable condition.
Myofascial pain syndrome is considered a common cause of neck pain, but is somewhat controversial because of reliability and validity issues with the diagnosis.17 The hallmark features of myofascial pain syndrome are:
- palpation of a taut band
- identification of an exquisitely tender nodule (myofascial trigger point) in the taut band
- reproduction of the patient’s symptomatic pain with sustained pressure.17
Prognosis
In acute traumatic conditions, clinicians can expect individuals to follow one of three likely trajectories: Mild problems with rapid recovery (approximately 45% of individuals depending on outcome); moderate problems with some but incomplete recovery (approximately 40% of individuals); and severe problems with no recovery (approximately 15% of individuals).16 Regardless of the outcome, recovery appears to occur most rapidly in the first six to 12 weeks after injury, with considerable slowing after that and little recovery after 12 months.16 Less evidence is available for acute non-traumatic (idiopathic) neck pain, but clinicians can still expect recovery to slow considerably after six to 12 weeks from onset.16
Management
The evidence base for the management of chronic neck pain is vast compared with that for acute neck pain. There are, however, principles to follow in the management of acute neck pain that have broad consensus and are at low risk of harm:
- Education and assurance: Potentially this is the most important step. Combined with a confident clinical appraisal, this can go a long way to alleviating concerns the patient might have and allow them to safely wean back into their normal activities as soon as possible. Advise patients to minimise their use of a cervical collar. Provide assurance that recovery in the first one to two months is likely.18
- Manual therapy and exercise prescription: For patients with movement restriction on examination, manual therapy to the cervical and upper thoracic spine should be considered.19 In the subacute phase (six to 12 weeks), manual therapy might be less effective. Exercises targeting cervical and scapulothoracic endurance become more important in this phase.
- Analgesics: These might be used, although their effectiveness is variable and limited. The standard advice for the use of analgesics for musculoskeletal pain should be followed.18 Pragmatically, this involves using the lowest-risk medicine at the lowest effective doses for the shortest period of time needed to assist recovery.
- Psychological interventions: These can be considered for distressed patients, usually in the subacute phase.20
- Return to work and usual activities: These should be encouraged as soon as is feasible and safe.21
Consideration might also be given to focal injections, although evidence for their effectiveness is limited. Trigger point injections seem better tolerated and more efficacious than dry needling. These injections are usually performed with a 25-gauge needle and 0.5–1% xylocaine. The needle is inserted into the trigger point and should elicit a twitch response. A small amount of xylocaine (0.1 mL) is then injected around the area.22
The particular techniques used for manual therapy and exercise prescription are manifold and no one approach has been found to be more efficacious than another. Responses seem to be very individual and must be tailored to the specifics of the patient’s presentation.
Conclusion
Patients with acute cervical spine pain will be frequently encountered in primary care in Australia. A thorough clinical evaluation will lead to safe and effective management in most patients. For those who are slow to recover, multidisciplinary care is appropriate. Patients with persistent pain despite appropriate care require further clinical assessment and consideration of specialist referral.
Key points
- Acute cervical spine pain is the fifth most common musculoskeletal presentation to Australian general practice.
- The evidence base for cervical spine pain is largely around chronic pain, yet early intervention of acute pain following general principles can minimise chronicity.
- Rule out red flags and address yellow flags early.
- Explain the diagnosis and generally good prognosis with active management.
- Follow a patient’s progress and implement interdisciplinary management if recovery is slow in the first four to six weeks.