Sport is incredibly popular in Australia, with over half the nation’s population participating in sporting activities each year.1 Although this has many benefits for physical and mental health, knee injuries are common, particularly in pivoting and contact sports, such as Australian rules football, rugby league, rugby union, touch football, netball, soccer and basketball. Australia has the highest rate of anterior cruciate ligament (ACL) reconstruction in the world.2 Athletes who injure their knee are at increased risk of knee osteoarthritis at a younger age.3 Management ranges from simple first aid and bracing through to complex surgical reconstruction, but should always include supervised rehabilitation as well as individualised strategies to promote lifelong engagement in exercise and osteoarthritis risk reduction.4
Aim
The aim of this review is to summarise the management of common sporting knee injuries, including injuries to the collateral and cruciate ligaments, menisci and the extensor mechanism. Key findings on history, examination and imaging are highlighted, and treatment options are discussed.
Common acute sport-related knee injuries
Collateral ligament injuries
The medial collateral ligament (MCL) is commonly injured when a valgus (lateral to medial) force is applied to the knee.5 Patients typically present with medial knee pain and might have difficulty weight bearing (Box 1). Examination involves applying a valgus force to the knee with the joint held at 30° of flexion (Figure 1A) and then in full extension. MCL injuries can be graded according to Table 1. Laxity in extension implies damage to other structures, for example the ACL or posterior cruciate ligament (PCL). Magnetic resonance imaging (MRI) is the imaging modality of choice to confirm the diagnosis (Box 2; Figure 2). Isolated MCL injuries rarely require surgical intervention and might be treated according to Table 1. The exception is an MCL avulsion from the tibia, which usually requires surgical repair or reconstruction.
| Box 1. Case 1 |
| A man aged 35 years sustained a valgus injury to his right knee in a soccer tackle. He noticed immediate medial-sided knee pain but was able to limp from the field. His knee was moderately swollen the following morning. Examination findings were consistent with a Grade 2 medial collateral ligament (MCL) injury. A magnetic resonance imaging scan demonstrated a partial rupture of the proximal MCL (Figure 2) with no other pathology. He was managed in an unlocked range-of-motion brace for six weeks, full weight bearing. He made a complete recovery and returned to competitive soccer three months after injury. |

Figure 1. Special tests for knee pathology.
A. Examination of the medial collateral ligament at 30° of knee flexion. The examiner applies a valgus (lateral to medial) force to the knee, feeling for medial joint gapping and the presence of an end-point. B. Examination of the lateral collateral ligament at 30° of knee flexion. The examiner applies a varus (medial to lateral) force to the knee, feeling for lateral joint gapping and the presence of an end-point. C. Examination of the anterior cruciate ligament (ACL) with Lachman’s test. With the knee held at 30° flexion, the examiner stabilises the distal femur with one hand and applies an anteriorly directed force to the proximal tibia with the other hand, feeling for anterior translation of the tibia in relation to the femur and the presence of an end-point. For patients with large thighs or clinicians with small hands, stabilising the distal femur on the examiner’s thigh (as shown), is an acceptable alternative. D. Examination of the ACL with an anterior drawer test. With the knee at 90° flexion, the examiner applies an anteriorly directed force to the proximal tibia, feeling for anterior translation of the tibia in relation to the femur and the presence of an end-point. E. Eliciting a lever sign. The examiner places a clenched fist underneath the patient’s proximal tibia. A posteriorly directed force is applied to the patient’s distal femur. In an ACL-deficient knee, the foot will remain on the bed. In an ACL-intact knee, the foot will raise off the bed. F. Examination of the posterior cruciate ligament with a posterior drawer test. With the knee at 90° flexion, the examiner applies a posteriorly directed force to the proximal tibia, feeling for posterior translation of the tibia in relation to the femur and the presence of an end-point. G. Examination for a meniscal tear using Thessaly’s test. The patient stands on the injured leg, with the knee held in 20° flexion. With the examiner assisting the patient to maintain balance, the patient performs a twisting manoeuvre, moving the knee into internal and external rotation. Pain or mechanical clicking indicates a positive test.
| Box 2. Role of imaging in acute sport-related knee injuries |
| X-ray |
- First-line investigation for significant acute sport-related knee injuries
- Will demonstrate fractures, dislocations and abnormal patella positioning with extensor mechanism disruptions
- Lipohaemarthrosis suggests occult intra-articular fracture
|
| Ultrasound |
- Limited role
- May be used to diagnose quadriceps or patellar tendon ruptures if MRI not available
|
| Computed tomography |
- Limited role
- May be used to detect occult fractures
- Useful for preoperative planning for intra-articular fractures
|
| MRI |
- Investigation of choice for collateral, cruciate and meniscal injuries
- May be used to diagnose tendinous disruption of the extensor mechanism
- Will also demonstrate chondral injuries and occult fractures
|
| MRI, magnetic resonance imaging. |

Figure 2. Proton-density, fat-suppressed, coronal magnetic resonance imaging reconstruction of the right knee demonstrating a partial thickness tear of the proximal medial collateral ligament (red arrow).
| Table 1. Medial collateral ligament injuries5,25 |
| Grade |
Examination findings |
Treatment |
| 1 |
0- to 4-mm medial joint gapping with valgus stress at 30° knee flexion |
Rest, ice, compression, NSAIDs, physiotherapy within one week for supervised early return to activity |
| 2 |
5- to 10-mm medial joint gapping with valgus stress at 30° knee flexion with a firm end-point
No laxity in extension |
Unlocked ROM brace for three weeks or more, full weight bearing, early physiotherapy while in brace for lower limb strengthening and neuromuscular retraining |
| 3 |
>10-mm medial joint gapping with valgus stress at 30° knee flexion without a firm end-point
Laxity in extension implies injury to other structures (eg ACL or PCL) |
Unlocked ROM brace for six weeks or more, full weight bearing for isolated MCL injury
Consider reconstruction if associated with injury to other structures |
| ACL, anterior cruciate ligament; MCL, medial collateral ligament; NSAIDs, non-steroidal anti-inflammatory drugs; PCL, posterior cruciate ligament; ROM, range of motion. |
Lateral collateral ligament (LCL) injuries are less common than MCL injuries, and rarely occur in isolation.6 They generally occur when a varus (medial to lateral) force is applied to the knee and are often associated with posterolateral corner (including the popliteus tendon, popliteofibular ligament and biceps femoris tendon) and PCL injuries. Examination involves applying a varus force to the knee with the joint held at 30° of flexion (Figure 1B) and then in full extension. LCL injuries can be graded according to Table 2. Laxity in extension implies damage to other structures; for example, the ACL or PCL. MRI is important to quantify the degree of LCL injury and to assess for other pathology (Box 2). Treatment options are presented in Table 2. Early orthopaedic referral is vital, because concomitant posterolateral corner injury, if present, often requires surgical intervention.7
| Table 2. Lateral collateral ligament injuries8 |
| Grade |
Examination findings |
Treatment |
| 1 |
0- to 5-mm lateral joint gapping with varus stress at 30° knee flexion with a firm end-point |
- Unlocked ROM brace for six weeks, full weight bearing, early physiotherapy while in brace for lower limb strengthening and neuromuscular retraining
|
| 2 |
6- to 10-mm lateral joint gapping with varus stress at 30° knee flexion with a firm end-point |
- Unlocked ROM brace for six weeks, full weight bearing, early physiotherapy while in brace for lower limb strengthening and neuromuscular retraining
|
| 3 |
>10-mm lateral joint gapping with varus stress at 30° knee flexion without a firm end-point
Laxity in extension implies injury to other structures (eg ACL or PCL) |
- LCL repair or reconstruction depending on acuity
- Repair or reconstruction of other injured structures
- Bony avulsions from the fibula can be directly repaired
|
| ACL, anterior cruciate ligament; LCL, lateral collateral ligament; PCL, posterior cruciate ligament; ROM, range of motion. |
Cruciate ligament injuries
ACL ruptures are typically sustained during non-contact pivoting manoeuvres or with valgus-directed force to the knee.8 Classically, the patient feels a ‘pop’ in the knee and experiences swelling within 60 minutes due to the development of a haemarthrosis7 (Box 3). The initial pain from the injury can settle quite quickly, but early examination might be challenging due to significant knee swelling. Delayed examination reveals a positive Lachman test (Figure 1C) and a positive anterior drawer test (Figure 1D). For patients with large thighs or clinicians with small hands, the lever sign (Figure 1E) may be elicited as an alternative to the Lachman test.9 MCL and lateral meniscus injuries are commonly associated with ACL ruptures, and these structures also need to be assessed on clinical examination. MRI confirms the diagnosis and demonstrates concomitant injuries (Box 2; Figure 3). Where timely access to MRI is not available, early X-ray should be performed to exclude an avulsion fracture of the tibial spine. This is particularly important in children, where surgical fixation might be indicated.
| Box 3. Case 2 |
| A man aged 23 years sustained a non-contact pivoting injury to his left knee while decelerating and changing direction during a basketball game. He felt a ‘pop’ in his knee and was unable to weight bear. He was assisted from the court and noticed immediate swelling in the knee. Examination in the acute phase was limited by pain and swelling; however, the collateral ligaments were clinically intact. A magnetic resonance imaging scan demonstrated a complete, mid-substance anterior cruciate ligament (ACL) rupture (Figure 3). After a six-week course of ‘pre‑habilitation’, the patient underwent an ACL reconstruction with an autologous hamstrings graft. He completed a 12-month course of postoperative rehabilitation. Although he made a full functional recovery, he elected not to return to competitive basketball. |
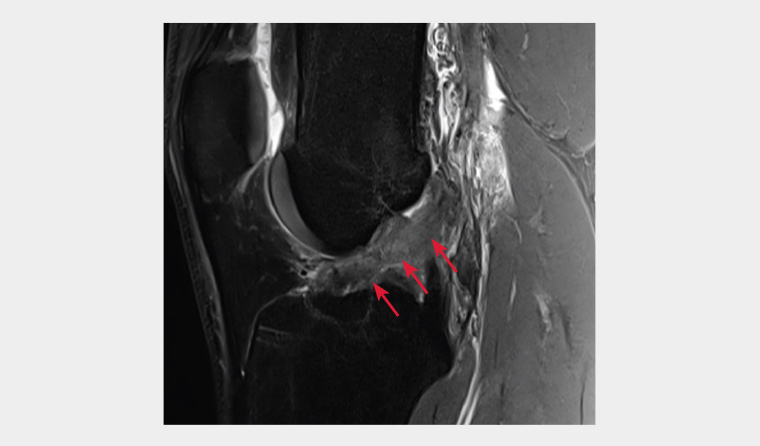
Figure 3. Proton density, fat suppressed, sagittal magnetic resonance imaging reconstruction of the left knee demonstrating a full thickness rupture of the anterior cruciate ligament (red arrows).
Treatment should be individualised and depends on the age and functional goals of the patient, as well as any concomitant injuries sustained. For younger patients aiming to return to pivoting sports, ACL reconstruction is recommended. For older patients engaging in lower-demand, non-pivoting activities, a trial of non-operative treatment with a physiotherapy-led rehabilitation program might be appropriate, but this decision should be made in consultation with an orthopaedic surgeon.10 In non-elite athletes, similar pain and disability outcomes are observed between early operative and trialled non-operative management with optional delayed surgery if an acceptable functional level cannot be achieved.11 Non-operative rehabilitation is contraindicated in patients with a repairable or obstructive meniscal tear or repairable chondral defect.10
Physiotherapist-supervised rehabilitation is vital and should begin as soon as possible in both the pre- and postoperative stages in the form of oedema management, range of motion and neuromuscular retraining.12,13 Exercise therapy should be individually prescribed and progressed based on tissue healing times (according to the surgeon’s instructions), the patient’s symptom response (minimal pain and swelling) and the patient’s performance against various neuromuscular criteria.12 Numerous criteria-driven guidelines have been described, with accepted criteria for return to driving, running and sport.12,14 Return to sport should be a controlled and supervised transition, where the patient is gradually exposed to more challenging (and fear-provoking) drills.4 Safe return to sport often takes 12 months or longer, and pre-injury level of participation is not achieved in many instances.15 Psychological factors, including fear of reinjury and reactive depression or anxiety, are one of the strongest predictors of an athlete not returning to sport.16 It is recommended that treatment providers pay attention to psychological recovery alongside physical criteria for return to sport.12 Regardless of operative or non-operative management, high rates of premature osteoarthritis and reduced health-related quality of life are observed after ACL injury.3,17 It is important to counsel patients about this early on in the decision-making process after the injury. Postinjury management should include education and self-management strategies for knee health, such as lifelong physical activity and healthy weight management.4
PCL ruptures are less common than ACL ruptures.18 In the sporting context, they occur either through a posteriorly directed force to the proximal tibia with the knee flexed or through a hyperextension injury. They might occur in isolation or in combination with a posterolateral corner injury. On examination, a posterior sag sign might be noted, and a posterior drawer test is positive (Figure 1F). PCL injuries might be graded according to Table 3. MRI is useful to assess for other pathology (Box 2). Isolated PCL injuries generally have good outcomes with non-operative treatment because there is usually minimal rotational instability (Table 3).
| Table 3. Posterior cruciate ligament injuries18 |
| Grade |
Examination findings |
Treatment |
| 1 |
1- to 5-mm posterior tibial translation on posterior drawer test |
- Physiotherapy within one week for quadriceps-focused strength and neuromuscular rehabilitation and graduated return to activity
|
| 2 |
6- to 10-mm posterior tibial translation on posterior drawer test |
- Physiotherapy within one week for quadriceps-focused strength and neuromuscular rehabilitation and graduated return to activity
- Consider using a PCL brace
|
| 3 |
>10-mm posterior tibial translation on posterior drawer test |
- PCL brace for 6–12 weeks
- Early physiotherapy while in brace for quadriceps-focused strength and neuromuscular rehabilitation
- Consider surgical fixation for bony avulsions
- Consider reconstruction if other structures injured
|
| PCL, posterior cruciate ligament. |
Meniscal injuries
Meniscal injuries are common in pivoting and contact sports.19 They might occur in isolation or in conjunction with ligamentous injuries. Lateral meniscal tears often occur in association with acute ACL ruptures, whereas medial meniscal tears are more common in ACL-deficient knees.20 Patients typically present with localised joint line pain and might have mechanical symptoms in the knee. Joint line tenderness is noted on examination, and meniscal provocation tests might be positive. However, McMurray’s test, Apley’s test and Thessaly’s test (Figure 1G) have limited diagnostic accuracy, and MRI is indicated if there is clinical concern for a meniscal injury.21 MRI will define the location and pattern of the meniscal tear, along with any associated chondral or ligamentous injuries (Box 2). Although some meniscal tears in young athletes can be managed non-operatively, many require arthroscopic repair or debridement. The general principle is to repair menisci wherever possible, to improve stability and prevent early cartilage damage and the development of osteoarthritis.22 Although degenerative meniscal tears in older patients can present acutely, these should be managed non-operatively.
Extensor mechanism injuries
The extensor mechanism of the knee comprises the quadriceps muscle (rectus femoris and vastus lateralis, intermedius and medialis), the quadriceps tendon, the patella, the patellar tendon and the tibial tubercle. Disruption of the extensor mechanism can occur through mid-substance tears or avulsions of the quadriceps or patellar tendons, or through fractures of the patella or tibial tubercle. Typically, these occur in older athletes via excessive eccentric loading of the extensor mechanism; for example, during jumping, landing or slipping. On examination, the patient will be unable to extend the knee, even with gravity eliminated. Plain X-rays will demonstrate fractures and an altered position of the patella on the lateral view (Box 2). Tendonous disruption might be confirmed on ultrasound or MRI.19 Early surgical intervention is required to restore the integrity of the extensor mechanism.
Fractures and dislocations
Fractures about the knee can occur in contact sports. These often require surgical treatment to restore articular congruity and maintain alignment of the lower limb. Red flags for fracture are the inability to weight bear, bony tenderness and an inability to flex the knee, and particular caution should be exercised in skeletally immature athletes (aged under 14 years) due to the possibility of growth plate injuries.23
Patellar dislocations are common, particularly in adolescent girls.8 Initially these might be related to minor trauma, but subsequent episodes are often atraumatic. A history of mechanical locking of the knee after a dislocation episode might indicate an osteochondral loose body, necessitating surgical intervention. Simple patellar dislocations are managed conservatively, with initial first aid management followed by a course of rehabilitation focused on lower limb kinematic retraining and quadriceps strengthening. Surgical patellofemoral stabilisation is indicated for recurrent instability failing conservative care.
Knee (tibiofemoral) dislocations are rare but devastating injuries.24 They typically occur in high-energy trauma, but are occasionally seen in contact sports. Knee dislocations generally involve multiligamentous disruption of the ACL and PCL, and either the MCL or LCL. There is a high incidence of concomitant vascular and neurological injury. Urgent surgical intervention is required.
Conclusion
Sports-related knee injuries are common in Australia. Initial assessment involves taking a thorough history and performing a careful physical examination. MRI is the imaging modality of choice to define ligamentous and meniscal injuries. Some knee injuries are managed non-operatively with physiotherapy-led rehabilitation, whereas others require surgical intervention. Patients should be educated on measures they can take to improve their lifelong knee health.
Key points
- Sport-related knee injuries are common in Australia.
- Isolated MCL, LCL and PCL injuries can often be managed non-operatively.
- ACL reconstruction is recommended for young patients aiming to return to pivoting sports.
- Meniscal tears and extensor mechanism disruptions often require surgical intervention.
- Multidisciplinary involvement of general practitioners, physiotherapists, sports and exercise physicians and orthopaedic surgeons will facilitate optimal patient care.