Case
A male property agent aged 32 years presented to his general practitioner (GP) with a history of blurred vision worsening over the preceding three months. The patient had noted his vision in both eyes was blurry, particularly when alternating from bright to dark environments. He had been recently well, but reported increased work-related stress in the preceding months. The patient denied headaches, nausea, vomiting and previous sensory or motor disturbances. He had been in a stable relationship for over five years but acknowledged he might have had prior unprotected sexual exposures. The patient was otherwise well, took no regular medications, had no known allergies or significant family history.
On examination, his blood pressure was 118/78 mmHg and random blood glucose was 4.8 mmol/L. Neurological examination showed normal reflexes, muscle tone and power in all four limbs. The cranial nerve examination was normal, as was the remainder of the physical examination. Visualisation of the optic discs was limited with direct fundoscopy without access to dilating drops. The patient was referred for urgent ophthalmology review.
The patient was seen by an ophthalmologist, who reported a corrected visual acuity of 6/7.5 in each eye, with no pinhole improvement. Pupil reactions were normal in each eye, and there was no relative afferent pupillary defect. There was a full range of extraocular movements and no ptosis or proptosis. Anterior segment examination was unremarkable. Fundus examination revealed bilateral blurred optic disc margins. There were retinal folds in the right eye and retinal nerve fibre layer haemorrhages in the left eye. An abnormal vascular pattern was noted suggestive of optic disc neovascularisation (Figure 1). This can be a useful retinal finding in the diagnosis of neurosyphilis.1,2 The appearance was consistent with severe bilateral optic disc swelling, which was confirmed with optical coherence tomography (OCT) scanning of the optic nerves. Automated perimetry showed impaired visual fields bilaterally.
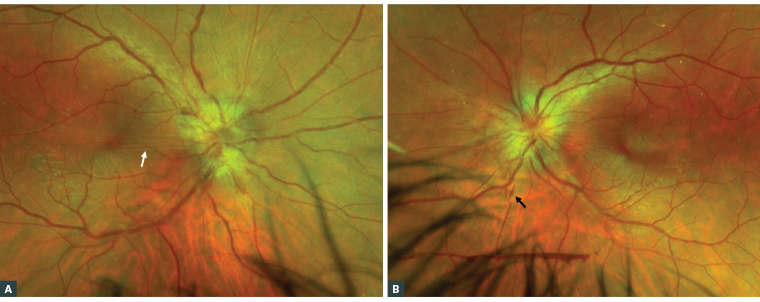
Figure 1. Bilateral optic disc swelling with blurred optic disc margins in the (A) right eye and (B) left eye. Note the retinal folds (white arrow) and retinal nerve fibre layer haemorrhages (black arrow).
Question 1
What are the differential diagnoses for bilateral optic disc swelling?
Question 2
What other tests/investigations could be useful to further investigate some of these diagnoses?
Answer 1
Differential diagnoses for bilateral optic disc swelling might be inflammatory or non-inflammatory, infectious or non-infectious, as follows:
- Inflammatory: Optic neuritis
- Non-inflammatory
- Vascular: Malignant hypertension, diabetic papillopathy, ischaemic optic neuropathy (arteritic and non-arteritic)
- Raised intracranial pressure: Idiopathic intracranial hypertension, intracranial space-occupying lesion
- Non-infectious: Multiple sclerosis, sarcoidosis
- Infectious: Syphilis, tuberculosis
Answer 2
Other tests/investigations to further investigate some of these diagnoses include:
- Neuroimaging: Urgent brain and orbits computed tomography (CT) with contrast or magnetic resonance imaging (MRI)/magnetic resonance angiography (MRA)/magnetic resonance venography (MRV) brain and orbits. Neuroimaging with an urgent brain and orbits CT with contrast or MRI/MRA/MRV is the most important immediate investigation. If an MRI cannot be readily obtained at short notice, then CT is the preferred initial investigation. In rural locations where assessment by an ophthalmologist might be delayed, the results of a prompt CT scan may help guide the appropriate referral destination.
- Haematological and biochemical screens:
- Serum angiotensin-converting enzyme
- QuantiFERON-TB Gold
- Syphilis serology.
Case continued
In this case, an urgent CT excluded a space-occupying lesion. Blood test results revealed positive syphilis serology, leading to a provisional diagnosis of neurosyphilis. The remainder of the blood tests were unremarkable.
Question 3
What other tests or issues should a GP consider?
Question 4
What are the stages of syphilis?
Question 5
How should this patient be further assessed and managed?
Answer 3
Patients with neurosyphilis should be investigated for other sexually transmissible diseases, including HIV, chlamydia and gonorrhoea. Syphilis is a nationally notifiable disease in Australia, and cases are monitored through the National Notifiable Diseases Surveillance System (NNDSS; www.health.gov.au/our-work/nndss). It is important that appropriate partner notification and contact tracing be performed. The Australasian Contact Tracing Guidelines (https://contacttracing.ashm.org.au) are a resource for medical professionals undertaking partner notification.
Answer 4
Syphilis is characterised into four stages: primary, secondary, latent and tertiary.3
The term ‘neurosyphilis’ is used to describe any central nervous system involvement, which can occur at any stage of infection. This can manifest with ocular signs, meningism and stroke-like symptoms due to cerebrovascular inflammation.4 Less commonly, neurosyphilis can progress to tertiary forms, such as general paresis.5
Answer 5
The patient was referred to a neurologist. Lumbar puncture revealed high titres on the Treponema pallidum particle agglutination assay (TPPA) and fluorescent treponemal antibody absorption (FTA). He was admitted for a 14-day course of 1.8 g intravenous benzylpenicillin, every four hours. This high-dose treatment is required to reach an adequate concentration in the cerebrospinal fluid.6 There was an improvement in the patient’s visual symptoms. The ophthalmologist reported an improvement in the bilateral optic disc swelling clinically and using optical coherence tomography scanning of the optic nerves over the subsequent three months.
Prognosis
Neurosyphilis has a good prognosis if identified and treated early. Although rare, it should be considered by GPs in the differential diagnosis of optic disc swelling.
Rising incidence of syphilis in Australia
The incidence of syphilis has increased fourfold from 2011 to 2019 (from 6.0 to 24.0 per 100,000 population).7 Syphilis rates have increased in particular among men who have sex with men and Aboriginal and Torres Strait Islander people, as well as in both remote and metropolitan regions.7 This has been correlated with a rising incidence of tertiary disease, as reflected by increasing neurosyphilis-related hospital admissions from 2014 to 2020.8
Key points
- Careful clinical examination is important in the management of blurred vision.
- In recent years, there has been an increased incidence of syphilis and neurosyphilis in Australia.
- Urgent neuroimaging is required in all patients with bilateral optic disc swelling to exclude a space-occupying lesion. In cases where neuroimaging is normal, alternative diagnoses, including neurosyphilis, should be considered.