This article is part of a longitudinal series on ear, nose and throat conditions.
Rhinology surgeries represent a diverse category of operations that vary in primary indication, surgical approach and resulting potential complications. Otolaryngological procedures are overall common, accounting for 12% of all elective surgical admissions in public hospitals for 2020–21.1 Complications stemming from surgery also vary in their incidence, with major complications being thought to occur in 1–3% of cases and minor complications occurring in up to 15% of cases.2,3 This, in conjunction with the paucity of otolaryngological education provided by both medical schools and subsequent speciality training programs, catalyses an environment in which patients can be left without a clear and timely treatment algorithm.4 This article aims to bridge this gap in knowledge by addressing common postoperative presentations and complications that can occur and highlighting strategies to manage these in the primary care setting.
Common postoperative presentations
Understanding complications following nasal surgeries is best done by appreciating that although certain rhinology cases can be complex and diverse, most elective rhinology procedures are performed in a uniform manner with similar at-risk end units and potential complications. The most common operations include turbinoplasty, septoplasty/septorhinoplasty (closed and open approaches) and endoscopic sinus surgery (Table 1).
| Table 1. Common nasal surgeries and their associated acute complications |
| Procedure |
Potential presentation |
| Endoscopic sinus surgery |
- Epistaxis
- Infective symptoms
- Nasal obstruction
- Nasal discharge
- Meningitic features
- Visual changes
|
| Turbinoplasty/turbinate reduction |
- Epistaxis
- Nasal obstruction
|
| Closed/open septorhinoplasty |
- Bruising/facial swelling
- Epistaxis
- Infection
- Nasal obstruction
- Nerve praxia/palsy
- Change in external nasal appearance
|
Following this, categorisation of symptomatology secondary to complications based on temporality from time of surgery also aids in identifying the underlying aetiology and appropriate management. Specifically, within the short term (within two to six weeks of surgery) and the longer-term postoperative period (greater than six weeks). Short-term complications and events can sometimes be temporised in a community setting, with appropriate consultation with the primary operator. Medium to long-term complications are issues that more often require otolaryngologist follow-up.
Assessment and management of frequent postoperative presenting complaints
Immediate postoperative period (first two weeks)
Epistaxis
A degree of epistaxis following most rhinology surgeries is to be expected within the first one to two weeks (Table 2). Reassuring features include bleeds that are small volume, darker pigmentation as opposed to fresh red blood and self-limiting bleeds. Initial examination should ensure that the patient is haemodynamically stable and not requiring immediate resuscitation. A brief examination of the nasal cavity can be performed with a head light (and speculum where available); should this not be accessible, an otoscope can provide a limited view of the nose (Figure 1). An examination of the oropharynx is also critical; a patient with significant active bleeding or clots visible in the oropharynx should be directed to their nearest emergency department with otolaryngology cover. As to initial investigations in the primary care setting, a full blood count can be informative, especially if recent investigations are at hand.
| Table 2. Common acute presentations, primary measures and when to escalate |
| Presentation |
Initial management |
Red flags |
Escalation |
| Minor epistaxis |
- Ensure haemodynamically stable
- Appropriate compression
- Cold pack/ice blocks
- Short course of oral tranexamic acid:
- Oral dose: tranexamic acid 500 mg, two to three times daily
|
- Large-volume bleed
- Haemodynamic instability
- Clot in the oropharynx
- Critically low haemoglobin (<70 g/L)
|
- If progressive or worsening, refer to primary operator or nearest otolaryngology centre
|
| Moderate/major epistaxis |
- Ensure haemodynamically stable
- Appropriate compression
|
- Large-volume bleed
- Haemodynamic instability
- Clot in the oropharynx
- Critically low haemoglobin (<70 g/L)
|
- Refer to nearest centre with otolaryngology cover in all cases
|
| Nasal obstruction |
- Appropriate history and examination to ensure not haematoma or abscess
- Increased nasal irrigation
- Short burst of nasal decongestant:
- Decongestant dose: oxymetazoline, two sprays (45 mcg ×2), twice a day for a maximum of three days
|
- Febrile illness
- Pain out of keeping with clinical findings
- Temperature or febrile illness
- Elevated white cells or acute phase reactants
|
- If progressive, abnormal examination or concerns, refer to primary operator or nearest otolaryngology centre
|
| Infective symptoms |
- Swabs with microscopy and culture where appropriate
- Oral and/or topical antibiotics:
- Topical agents: gramicidin/neomycin/nystatin/ triamcinolone or mupirocin ointment 1 cm to affected area
- Oral agents: cephalexin 500 mg, twice daily; amoxicillin/clavulanic acid 875/125 mg, twice daily
|
- Haemodynamic instability
- Temperature or febrile illness
- Elevated white cells or acute phase reactants
|
- Notify primary operator in all cases
- If systemic and/or progressive, refer to nearest otolaryngology centre
|
| Bruising/facial swelling |
- Appropriate eye examination
- Cold compresses
- Topical emollients
|
- Eye signs
- Temperature or febrile illness
- Elevated white cells or acute phase reactants
|
- If associated with eye symptoms, urgent referral to nearest centre with otolaryngology or ophthalmology cover
|
| Rhinorrhoea |
- Appropriate history and examination to exclude CSF leak
- Specimen jar to collect discharge where appropriate with pathology form for beta‑2‑transferrin test
- Short burst of nasal decongestant:
- Decongestant dose: oxymetazoline, two sprays (45 mcg ×2), twice daily for a maximum of three days
|
- Clear, continuous and thin rhinorrhoea
- Associated features of meningitis
|
- If persistent, notification to the primary operator is warranted
- If associated with features of meningitis, refer to nearest otolaryngology centre
|
| Paraesthesia |
- Appropriate reassurance
- Exclusion of other causes
|
|
- If persistent, notification to the primary operator is usually appreciated
|
| Impaired olfaction |
- Exclude cacosmia (unpleasant parosmia) and potential infection
- Increased nasal irrigation
- Intranasal steroid spray
- Smell retraining
- Intranasal steroid agents:
- Mometasone spray, two sprays (50 mcg ×2), each nostril, twice daily
- Mometasone 0.1% hydrogel, 1 cm in saline nasal irrigation, daily
|
- Infective symptoms
- Temperature or febrile illness
- Elevated white cells or acute phase reactants
|
- If persistent, notification to the primary operator is usually appreciated
|
| Visual change |
- Appropriate history and examination
- Refer to nearest centre with otolaryngology or ophthalmology cover
|
|
- Refer to nearest centre with otolaryngology or ophthalmology cover in all cases
|
| CSF, cerebrospinal fluid. |
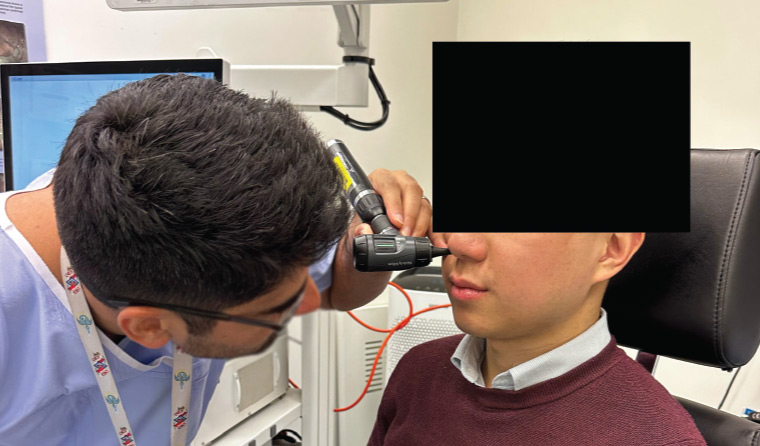
Figure 1. Otoscopic examination of the nasal cavity.
In the case of minor bleeds (ie self-limiting episodes of spotting), appropriate first-aid measures, such as compression over the lower third of the nose, an ice pack over the nasal dorsum/forehead/nape of neck or getting the patient to suck on an ice cube, may be applied.5 Following this, consideration of a short course of tranexamic acid orally might be of some benefit in patients without contraindications (Table 2).6
Bruising and facial swelling
Bruising and facial swelling in the context of open septorhinoplasty is to be expected. Bruising and swelling should be transient and resolve substantially within the first two weeks.
Initial examination should include a thorough examination of eye movement and visual acuity and notation of any chemosis or proptosis. If any of these examination findings are abnormal, an urgent referral to the nearest tertiary otolaryngology service is warranted.
Nasal obstruction
Nasal obstruction is common in the short-term postoperative period in the context of post-surgical oedema and crusting, especially with surgeries such as septoplasties and turbinoplasties. Other causes might include the presence of splints, as in the case of septoplasty, or retained absorbable and non-absorbable packing material (Table 3). In these cases, the symptoms are usually self-limiting. However, nasal obstruction can also be a herald of septal haematoma or abscess, which requires immediate attention by an otolaryngologist.
| Table 3. Management of common postoperative dressings, sutures and packing materials |
| Postoperative dressing, sutures and packing materials |
Management |
Escalation |
- Dissolvable packing
- Common products:
- NasoPore
- Merocel
- Surgicel
- Merogel
- Floseal
- Surgiflo
- Chitogel
- PureRegen
- PuraStat
|
Routine gentle saline nasal irrigation |
Retained packing will require nasal toileting performed by an otolaryngologist |
- Non-dissolvable packing
- Doyle splints
- Silastic splints
|
Leave in place |
If dislodged or retained, contact primary operator urgently |
- External nasal splints
- Aluminium
- Thermoplastic
- Plaster
|
Can be removed at one week postoperatively, or in accordance with primary operator recommendations |
If dislodged, contact primary operator |
|
|
Can be replaced as required, can be refashioned from tubular net dressing and gauze |
N/A |
- External nasal sutures
- Usually non-absorbable PDS or nylon
|
Usually topical ointment (medicated or unmedicated) until removal or as per primary operator recommendations |
If painful, erythematous or purulent, contact primary operator urgently |
- Internal nasal sutures
- Usually dissolvable vicryl, chromic
|
Routine gentle saline nasal irrigation |
If painful, erythematous or purulent, contact primary operator urgently |
| PDS, polydioxanone. |
Identification of these entities can be performed through an appropriate history and examination and assessment with a set of observations including temperature and potentially bloods examining white cells and acute phase reactants. Haematoma or abscess will present with progressively worsening obstruction that can be unilateral or bilateral; this can also be associated with significant pain/fever.7 Examination with a speculum or otoscope might reveal an area of fluctuant swelling with associated erythema (Figure 1). In the case of a recent septoplasty and worsening obstruction, timely notification to the primary operator is usually warranted. A short course of intranasal decongestant of up to three days can be considered, but this will not relieve anatomical causes of obstruction, such as haematoma (Table 2).
Infective symptoms
Infections and their course can be varied depending on the surgery. Acute episodes of sinusitis can present with all nasal surgeries secondary to obstruction of mucosal outflow drainage tracts and result in patients presenting with symptoms akin to acute sinusitis, including purulent discharge, frontal and facial congestion/pain and systemic fevers. Nasal examination might reveal frank discharge and purulence and potentially a site/cause of obstruction. Initial investigations should include a set of observations, a nasal swab if obvious purulence is identified and basic bloods examining inflammatory markers. Initial therapy should include rigorous nasal irrigation, antibiotics for acute sinusitis as per local guidelines with or without the addition of a burst course of oral steroids and/or a short course of intranasal decongestant (Table 2). In patients who are haemodynamically unstable, exhibit changes in vision or have a significant degree of periorbital or preseptal swelling, referral to the nearest otolaryngology centre and prompt notification to the primary operator is warranted. Likewise, any features of meningism necessitate urgent referral to the nearest emergency department.
Infections along incision lines within the nose or external portions of the nose can also present a significant challenge. Often this will present with localised erythema, oedema and pain. Initial investigation should include a wound swab of any overt discharging purulent site. Initial treatment can include topical antibiotic preparations as well as appropriate oral antibiotics, but this should be done in close consultation with the primary operator and local guidelines (Table 2).
Rhinorrhoea
A degree of rhinorrhoea can be common after surgeries, either from post-surgical irritation of the mucosal lining of the nasal cavity or because of temporarily retained saline nasal irrigation solution. Rhinorrhoea that is persistent, thin, not associated temporally with saline irrigation and accompanied by a salty or metallic taste or features of meningism can suggest a leak of cerebrospinal fluid and should be urgently referred on to the nearest tertiary centre.
Visual changes
In the context of recent rhinology surgery, all visual changes warrant urgent consultation with the primary operator and/or referral to the nearest tertiary centre.
Greater than two weeks
Epistaxis
Bleeding that is recurrent and/or occurring beyond two weeks of the postoperative period can potentially signal an underlying disorder and thrombophilia screening can be considered. In any case of significant or concerning epistaxis in the post-surgical setting, the primary operator or operating facility should be notified.
Bruising/facial swelling
Complete resolution of all soft tissue swelling often takes several months. In cases of non-progressive bruising/swelling without associated symptomatology, the use of topical agents such as topical emollients (Arnica montana and bromelain) and cold compresses might be of benefit.8,9
Bruising and swelling in other rhinology procedures is much less common. In these circumstances, disruption of the anterior ethmoidal artery and/or progressive haematoma must be investigated. Concerning elements of the history would include progressive bruising/swelling, asymmetrical bruising/swelling, visual change and associated pain.
Nasal obstruction
Nasal obstruction related to postoperative soft tissue swelling and inflammation is common beyond two weeks and might take several weeks to settle. Delayed-onset nasal obstruction might also occur in turbinoplasty through the formation of synechiae between the nasal septum and turbinate. Nasal irrigation continues to be a mainstay of management in these circumstances. Features that should prompt escalation and further investigation include a rapid increase in nasal obstruction, no improvement in nasal obstruction, features of haemorrhage and infective features. Work-up and investigation of these features after two weeks is identical to that aforementioned.
Paraesthesia
Irritation and secondary temporary neuropraxia to the anterior ethmoidal nerve and nasopalatine nerve can result in temporary paraesthesia along the skin of the nose and upper front incisors. This is most commonly observed in surgeries such as open septorhinoplasty or septoplasty and although this can most often resolve, permanency of symptoms can also occur.
Impaired olfaction
Impaired olfaction, specifically hyposmia, is common after the majority of rhinology surgeries given occlusion of the olfactory groove from post-surgical oedema, packing material and silastic stents. Cacosmia can also be present in the setting of acute infection. Progressive obstruction can be due to sinister aetiologies such as haematoma or abscess. Initial examination can include an examination with an otoscope just to assess for retained debris or packing material. Initial management should include more frequent nasal saline irrigation, the use of a steroid-based nasal spray and smell retraining where available. In the finding of acute infection, notification to the primary surgeon should be pursued.
Changes in external nasal appearance (uncommon)
Changes in the appearance of the nose other than what is surgically intended are uncommon. In the early stages of healing, the nares might be more dilated due to the presence of surgical packing and splints, but this is expected to recover. Necrosis of the septal cartilage, although uncommon, might present long term with a saddle nose deformity. In the case of open septorhinoplasty, a scar at the base of the columella is expected to be present long term and should fade over time. Changes in the appearance of the nose and any associated functional impairment should be referred back to the treating otolaryngologist.
Conclusion
This article serves as a guide to acute presentations that can occur in the primary care setting in patients who have recently undergone rhinology procedures. It addresses initial measures that will temporise and/or alleviate the majority of non-urgent concerns and, importantly, will aid in reassuring the patient and general practitioner in the postoperative setting. Common presenting complaints, including epistaxis, facial swelling and bruising and nasal obstruction, can usually be safely managed with conservative measures. Any clinical concern or patient concerns that are out of keeping with the expected postoperative course, including those that persist despite temporising measures, should be brought to the attention of the primary operator or local otolaryngology unit. When in doubt, reassessment by the surgeon is the safest means of escalation.
Key points
- Rhinology procedures are common and diverse. In the case of complications, they provide a diagnostic dilemma for general practice because it is often difficult to identify what exactly has been performed.
- Familiarity with the gamut of complications that can arise and thorough history, examination and preliminary investigations are helpful in triaging and the initial management of complications.
- Complications and persistent symptoms outside of the immediate postoperative period should be referred back to the treating surgeon or unit.
- Many complications can be resolved safely in the community. When in doubt, discuss with your local otolaryngology provider or unit.
- Red flag complications requiring urgent escalation include: evidence of septal haematoma/abscess, visual change, large volume haemorrhage or features of sepsis.