Case
A 74-year-old man with a long-term indwelling urinary catheter due to neurogenic bladder presented with recurrent urinary tract infections. He had a background of uncontrolled hypertension, longstanding poorly controlled type 2 diabetes and end-stage renal failure. An ultrasound of the urinary system revealed bilateral renal parenchymal disease with left mild hydronephrosis with incidental findings of two well-defined hypoechoic structures within the pelvis that appeared to be in communication. Further, computed tomography urography revealed a left extrarenal pelvis with no hydronephrosis. The urinary bladder wall was diffusely thickened, measuring 0.7 cm. A large, thin, smooth-walled, ovoid cystic structure was seen posteriorly and in communication with the urinary bladder. This structure measured 8.8 cm × 11.0 cm × 13.6 cm and appeared larger than the urinary bladder. A smooth, oval-shaped, radiopaque structure was seen within this cystic structure (Figures 1,2).
The patient was treated for the urinary infection with oral antibiotic cefuroxime 500 mg twice a day for seven days and regular two-weekly indwelling urinary catheter change. This patient refused any surgical intervention for the large cystic mass.
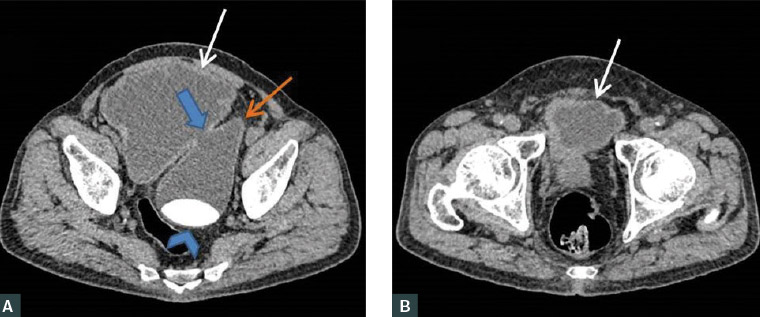
Figure 1. A. Axial contrast-enhanced computed tomography scan images showed the urinary bladder (white arrow) and the site of communication (blue arrow) with the outpouching cystic structure (orange arrow). A large radiopaque ovoid structure (blue arrowhead) was noted within the diverticulum. B. Axial contrast-enhanced computed tomography scan image inferiorly, showed the urinary bladder (white arrow) with thickened wall.
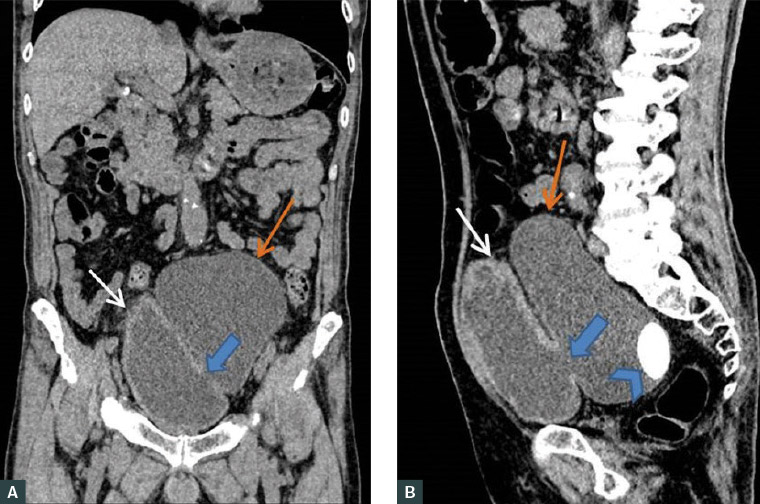
Figure 2. A. Coronal and B. sagittal contrast-enhanced computed tomography scan images showed a urinary bladder with a thickened wall (white arrow), the site of communication (blue arrow) with the large outpouching cystic structure (orange arrow) and a radiopaque structure (blue arrowhead) within the diverticulum.
Question 1
This is a man diagnosed with urinary bladder cystitis and a giant urinary bladder diverticulum with calculus formation within. What are the key management priorities?
Question 2
What are the potential risks of malignancy and the best plan for surveillance?
Question 3
What are the non-surgical management options for him?
Answer 1
Immediate management of this patient would include appropriate antimicrobial treatment for urinary tract infection and regular change of the indwelling catheter with an urgent urological review for treatment options of a bladder diverticulum presenting with calculus formation, which may include elective surgical excision, endoscopic care or conservative non-operative therapy.1
Answer 2
Urinary bladder diverticulum results from herniation of the mucosa and submucosa through the muscularis propria of the urinary bladder wall. It can be congenital or acquired.2 Acquired cases of a bladder diverticulum are more commonly seen among men over 60 years of age. Causes are varied, which include bladder outlet obstruction, neurogenic vesicourethral dysfunction or iatrogenic causes.2
Neoplastic changes may occur in a diverticulum with potential spread beyond the urinary bladder because the diverticulum wall consists only of urothelium without muscle.3
Urothelial cell carcinoma is the commonest cancer type seen in a diverticulum, preceded by squamous cell carcinoma, seen between the ages of 65 and 75 years.3,4 The occurrence of tumours in the diverticula ranges from 2% to 10%, and prognosis is usually poor due to the lack of a smooth muscle layer. The aggressiveness of these tumours, likelihood of spread and clinical consequences remain uncertain.3,4
Patient counselling and surveillance will include empathic education regarding the likelihood and prognosis of malignant changes, with precise information regarding red flags to be aware of, such as haematuria, dysuria and other lower urinary tract symptoms.2 The length and scheduling of surveillance are not objectively defined, but surveillance consists of regular symptom review, urine investigation (including cytology) and regular cystoscopy examinations.2
Answer 3
This man with a symptomatic large urinary bladder diverticulum requires a diverticulectomy with bladder diverticula calculus removal due to the risks of diverticular obstruction, new bladder calculus formation, enlargement of current bladder calculus, infections and carcinogenesis.1,2,5 However, he had refused surgery.
Non-surgical management options include conservative non-operative therapy and endoscopic care, which includes periodic monitoring of symptoms, red flags, urine cytology and cystoscopy.2 There is a role for clean intermittent catheterisation in patients who cannot proceed with the surgical removal of the diverticulum or those who remain symptomatic despite the relief of obstruction.2
Additionally, oral alkalinising agents and increased fluid intake can reduce the risk of developing new calculus. Manipulation of urinary pH has important consequences on antibiotic potency, but the interactions between alkalising agents and antibiotics are largely untested clinically.6 Theoretical in vitro experiments found synergic effects of ciprofloxacin and co-trimoxazole at higher urine pH.7 However, there was no change in amoxicillin activity noted at a higher urine pH.7 Despite limited clinical trials, physicians should exercise caution and continue to monitor for potential side effects from antibiotics in patients with urinary tract infection who are also receiving urine alkalinising agents.
Key points
- Acquired causes for a bladder diverticulum vary from bladder outlet obstruction to neurogenic vesicourethral dysfunction to iatrogenic causes.
- Complications of a bladder diverticulum are urinary retention, recurrent urinary tract infections, diverticular calculi and neoplastic changes.
- Non-surgical treatment options for a bladder diverticulum include conservative non-operative therapy and endoscopic care.