This article is part of a longitudinal series on sleep.
Insomnia is a highly prevalent and debilitating condition in Australia.1,2 For six consecutive years, The Royal Australian College of General Practitioners’ (RACGP) Health of the Nation survey has found that sleep disturbance and mental health concerns are the most common presenting symptoms in general practice patients.3
Insomnia can be a short-term/subacute response to cognitive, physical or behavioural stimuli (less than two weeks), or an acute (less than three months) or chronic (three months or more) condition (Box 1).4,5 Acute insomnia is prevalent in approximately 30–50% of the adult general population, whereas 10–15% meet the criteria for chronic insomnia at any given time.1,6 In addition to causing daytime fatigue, concentration difficulties and poor mood, insomnia reduces quality of life and increases the risk of depression.
| Box 1. Diagnostic criteria and classification of insomnia disorder |
Diagnostic criteria for insomnia disorder
- Dissatisfaction with sleep quantity or quality associated with at least one of the following, occurring at least three nights per week:
- difficulties initiating sleep
- difficulties maintaining sleep (frequent or long awakenings)
- undesired early morning awakenings.
- Sleep disturbance causes significant distress or impaired social functioning (eg daytime fatigue, concentration difficulties, memory problems, poor mood, social, occupational, academic, educational or behavioural functioning).
- Sleep difficulty occurs despite adequate sleep opportunity.A
- Not better explained by another sleep–wake disorder.B
- Not due to comorbid mental and physical conditions.B
- Not attributable to physiological effects of a substance (eg drug of abuse, medication side effect).
Classification of insomnia
Insomnia can be classified as an acute (less than three months) or chronic (three months or more) disorder.
Insomnia disorder is diagnosed via self-reported symptoms.5 Patients with suspected sleep apnoea should be referred for an overnight sleep study or further investigation by a sleep physician. |
AInsomnia symptoms that are due to external factors reducing the opportunity for sufficient sleep quality and/or duration may not be suitable for cognitive behavioural therapy for insomnia (CBT-i; see note on perinatal insomnia in the Psychologist Referral section).
BIt is rarely possible to determine whether insomnia is better explained by comorbid sleep or mental or physical conditions based on pretreatment information. For this reason, targeted assessment and treatment for insomnia is strongly recommended. |
Insomnia is thought to result from a combination of predisposing, precipitating and perpetuating factors.7 Predisposing factors place an individual at greater risk of sleep disturbance (eg increased trait anxiety, stress or worry, genetically determined factors). Precipitating factors include any initial triggers of short-term sleep disturbance (eg acute pain, jet lag, medication side-effects, stressful events). Finally, perpetuating factors are any psychological, behavioural or physiological factors that maintain the insomnia over time, even after the initial precipitant has resolved.
Insomnia requires targeted assessment and management/referral, whether occurring as an independent condition or comorbid with other mental, physical or sleep disorders. Insomnia is no longer considered a secondary symptom of these other conditions, because it can be treated in the presence of these comorbidities,8 and successful treatment of insomnia often improves the subsequent management of comorbid disorders.8–11 For example, there is now overwhelming evidence that non-pharmacological treatment of insomnia improves symptoms of both insomnia and depression.9,12–14
Management of insomnia in general practice has often relied on pharmacotherapy (eg benzodiazepines, ‘Z-drugs’, melatonin; henceforth called ‘sleeping pills’), which can provide short-term symptomatic improvement for insomnia, but is associated with the risk of side effects, adverse events and patterns of dependence.15,16 Unlike cognitive behavioural therapy for insomnia (CBT-i), sleeping pills do not target the underlying perpetuating factors of chronic insomnia. Therefore, among patients with chronic insomnia, sleeping difficulties may return soon after medication cessation due to withdrawal effects and persistence of a conditioned insomnia response.17 In fact, the use of sleeping pills may contribute to the maintenance of insomnia through reinforcement of anxiety and avoidant mechanisms, psychological and physiological dependence. For example, patients may develop a fear of not being able to sleep without medication that could contribute to worse sleep-related anxiety/alertness on nights that sleeping pills are not consumed. Alternatively, patients who use sleeping pills intermittently (prn) may also indirectly reinforce patterns of dependence by misattributing any nights of better sleep quality to the presence of medication and misattributing nights of broken/poor quality sleep to the absence of medication (where, in fact, the natural build-up and release of sleep pressure is more likely contributing to these intermittent nights of adequate/poor sleep quality). In addition, patients who use sleeping pills intermittently (prn) may develop a stronger dependence on medication by experiencing a greater contrast between better sleep on medicated nights following poor sleep and greater resultant sleep drive from unmedicated nights. A short course of sleeping pills at the lowest effective dose may be appropriate in a minority of specific circumstances, with close oversight of general practitioners (GPs) to prevent long-term dependence. Despite some evidence that rates of benzodiazepine prescribing for insomnia may be declining in Australia, the number of people on these medications long term is still a concern.18–20
Several evidence-based insomnia assessment and non-pharmacological management options exist and are becoming increasingly available to GPs. CBT-i is the recommended first-line treatment for insomnia.4,15,21 CBT-i is a multicomponent therapy (Table 1) that aims to identify and gradually treat the underlying factors that cause insomnia. For this reason, CBT-i improves insomnia, daytime function, mental health and quality of life, with these improvements persisting long after therapy cessation. CBT-i has historically been delivered by trained psychologists during weekly individualised treatment sessions over the course of six to eight weeks, but has also been translated to interactive online programs, brief behavioural programs and group-based programs, suitable for the general practice setting.22
| Table 1. Core treatment components of cognitive behavioural therapy for insomnia |
| CBT-i component |
Description |
| Sleep education/psychoeducation |
- Evidence-based information about sleep, insomnia and the factors that control the timing, duration and quality of our sleep (eg sleep cycles through deep and light sleep approximately every 90 min, with awakenings normally occurring at the ends of each cycle)
- Description of sleep pressure (Process S) and the biological clock (Process C) to help patients understand the rationale for behavioural treatment components
|
| Bedtime restriction therapy |
- Bedtime restriction therapy aims to temporarily reduce the time spent in bed over a number of consecutive nights/weeks to increase sleep pressure, reduce time spent awake in bed and overcome conditioned relationships between the bedroom and a state of alertness
- As sleep improves, time in bed can be gradually extended by 15–30 min from week to week, until a comfortable equilibrium between sleep pressure (sleepiness), sleep duration and time in bed is achieved
- Never restrict time in bed below 5.5 h
|
| Stimulus control therapy |
- Stimulus control therapy aims to reduce the association between the bed/bedroom environment and a state of conditioned psychological and physiological arousal
- Patients are instructed:
- To only use the bed/bedroom for sleep and intimacy
- To only go to bed when ‘sleepy’ (different from fatigue)
- If not asleep, or still feeling alert/worried/anxious, after approximately 15 min, to get out of bed and go to another room
- To do a relaxing activity to wind down (breathing exercises, light chores, stretching)
- To repeat Steps 2–4 until asleep
- To get up at the same time each morning, no matter how much they slept that night
- To avoid daytime naps longer than 15–20 min, especially naps occurring later in the afternoon or evening
- To use this technique each night of the week to gradually reassociate the bedroom with sleep and relaxation
|
| Relaxation therapy |
- Relaxation therapy includes a range of techniques to reduce arousal and anxiety at bedtime (eg progressive muscle relaxation, mindfulness meditation)
|
| Cognitive therapy |
- Cognitive therapy aims to identify, test and replace any potentially maladaptive or dysfunctional beliefs about sleep; some sleep-related beliefs (eg the anticipated consequences of sleep loss) can cause anxiety about sleep and result in maladaptive behaviours that interfere with sleep
|
For an overview of additional cognitive behavioural therapy for insomnia (CBT-i) components and adjunct treatments, see Winter et al.24
For a step-by-step model of general practitioner-delivered brief behavioural therapy for insomnia, including sleep education, bedtime restriction therapy and stimulus control therapy instructions, see Sweetman et al.25 |
‘Sleep hygiene’ includes information about diet, exercise, caffeine and technology use before sleep and in the bedroom. Although sleep hygiene is one of the most common approaches used to manage insomnia, most patients with chronic insomnia already engage in healthy sleep behaviours but experience little benefit. Consequently, sleep hygiene information is not an adequate standalone treatment for chronic insomnia.23
Aim
This article aims to present GPs with the knowledge and tools to identify and assess patients for insomnia symptoms, as well as provide an understanding of different treatment and referral options and further resources on insomnia assessment and management.
Insomnia management in general practice
A GP insomnia assessment, management and referral model is presented in Figure 1. Assessment considerations, specific screening tools and management options are described in the corresponding sections below.
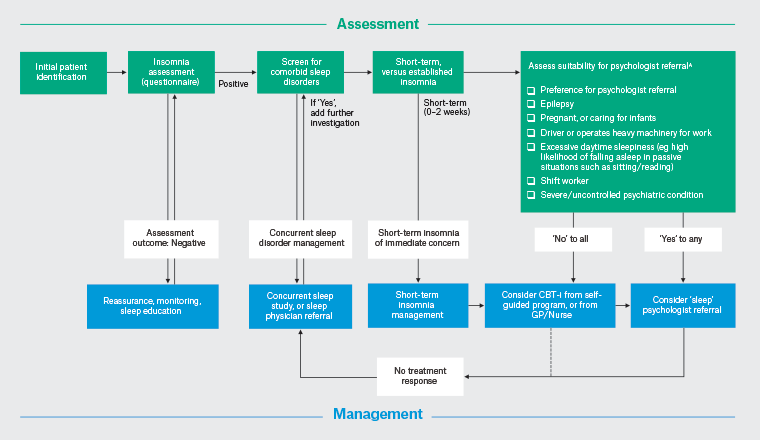
Figure 1. Flow diagram of general practitioner (GP) assessment and management of insomnia.
AFull psychologist referral criteria: www.sleepprimarycareresources.org.au/insomnia/referral-to-psychologist
CBT-i, cognitive behavioural therapy for insomnia. Click here to enlarge
Insomnia is a heterogeneous disorder. The management model presented in this article can be used as a general guide and adapted to each individual’s sleep pattern, comorbidities, setting, access to trained clinicians locally and via telehealth, and circumstances as required.
Identification of patients with insomnia
Patients with insomnia are relatively easily identified if their primary presentation is with sleeping difficulties. However, many patients with insomnia may not mention their sleeping difficulties to their GP. The primary reason for attending may be for management of another condition and the patient may consider their sleep problems to be of secondary importance or that there are no effective treatments for insomnia other than medications, which many patients wish to avoid. The risk of missing insomnia is particularly high among patients who present with mental health symptoms, chronic pain and chronic respiratory or cardiac disease, because these conditions are known to be associated with a high prevalence of insomnia.1,3 This can be avoided by proactively asking simple questions about the presence and frequency of any sleeping difficulties, and impacts on daytime function. Questions about sleep difficulties can also be asked during the preparation of a chronic disease management plan or a mental health treatment plan. Finally, it may be useful to audit electronic medical records to identify patients with recent or historical prescriptions of medicines used for insomnia (eg benzodiazepines, Z-drugs, melatonin, quetiapine) to identify patients for alternative or additional non-pharmacological management.26
Insomnia assessment
Among patients with suspected insomnia, GPs can assess for insomnia severity and chronicity with brief standardised questionnaires or conversations with patients (Table 2). Patients with clinically significant nocturnal insomnia symptoms that cause daytime distress or functional impairment may be suitable for further management and/or referral. Interactive insomnia assessment questionnaires are available on the RACGP-approved sleep health primary care resource.
| Table 2. Insomnia questionnaires and interpretation |
| Questionnaire |
Description and interpretation |
| Insomnia Severity Index28 |
Seven-item measure of global insomnia severity (assessment of symptoms, does not reflect diagnosis)
Higher scores indicate greater insomnia severity
- Scores ≥15 indicate clinically significant moderate insomnia; however, patients below this threshold may also be appropriate for CBT-i
|
| Sleep Condition Indicator29 |
Eight-item measure of insomnia that maps on to diagnostic criteria
Lower scores indicate greater insomnia severity
- Scores ≤16 indicate possible insomnia disorder; however, scores above this threshold may also be appropriate for CBT-i
|
| One-week sleep diary25 |
Allow patients to self-report time in bed, sleep time, time to first fall asleep, number of awakenings and total duration of awakenings, each morning after getting out of bed, for one week
Different sleep diary formats/structures are available (eg visual, text-based, online sleep diaries)
Sleep diaries are a very useful tool in the initial assessment of insomnia and during the delivery of CBT-i |
All of these measures are available online at sleepprimarycareresources.org.au
CBT-i, cognitive behavioural therapy for insomnia. |
Many patients with long-term sleeping pill use may be suitable for CBT-i. CBT-i is effective in the presence of sleeping pill use (which can mask insomnia symptoms) and can help patients gradually withdraw from sleeping pills by attenuating withdrawal symptoms, treating the underlying causes of insomnia and providing confidence to commence a gradual withdrawal schedule.17
When assessing insomnia symptoms, it can also be useful to use questionnaires such as the Flinders Fatigue Scale27 and a depression scale to assess for comorbid mental health symptoms.
Subclinical insomnia symptoms
Patients with subclinical symptoms (eg mild nocturnal symptoms without any daytime impact) may benefit from reassurance and the provision of sleep education resources (eg the Sleep Health Foundation produces evidence-based sleep and insomnia fact-sheets; Box 2). Advice about healthy sleep habits, diet, alcohol and caffeine consumption, exercise and regular sleep–wake rhythms may be useful in preventing the development of insomnia. However, such sleep hygiene information is not a sufficient standalone treatment for chronic insomnia. Although most cases of mild/acute insomnia remit after resolution of the underlying precipitant (eg work stress, jet lag, acute pain), a minority of patients experience a worsening of symptoms and the development of chronic insomnia.30 Therefore, patients with subclinical insomnia should be monitored and encouraged to seek further care if symptoms persist or become worse.
| Box 2. Insomnia education and treatment resources for general practitioners |
General practitioners (GPs) interested in accessing the most recent evidence-based sleep disorder information, education events, assessment, treatment and referral pathways are encouraged to join the Australasian Sleep Association Primary Care Sleep Health Implementation Network. Contact: Alexander Sweetman, alexander.sweetman@sleep.org.au
Specific cognitive behavioural therapy for insomnia (CBT-i) education programs for GPs and psychologists are being developed to increase the availability of clinicians with CBT-i training and experience.
GP education resources and clinical guidelines include:
- GP Insomnia and Sleep Apnoea Guideline (www.sleepprimarycareresources.org.au)4
- gpLearning ‘Managing insomnia in general practice’ module (www.racgp.org.au/education/professional-development/online-learning/gplearning)
- A step-by-step guide to GP delivery of a brief behavioural treatment for insomnia25
- SA Health’s Insomnia Management Kit46
- The Royal Australian College of General Practitioners’ benzodiazepine guideline.15
Insomnia treatment and referral options include:
- The Sleep Health Foundation website (www.sleephealthfoundation.org.au), which has a wide range of patient fact sheets
- Reconnexion, a Victorian benzodiazepine dependence service (www.reconnexion.org.au)
- Online CBT-i programs that are often freely available through clinical research trials (GPs with an interest in accessing implementation trials for sleep disorders are encouraged to contact Alexander Sweetman, alexander.sweetman@sleep.org.au)
- This Way Up, a free online insomnia program (www.thiswayup.org.au)
- A Mindful Way, an at-cost online mindfulness + CBT-i program (www.amindfulway.com.au)
- Specialist sleep psychologists, who are available in most Australian capital cities and can be accessed via telehealth for patients in rural/remote settings. The Australasian Sleep Association is collaborating with the Australian Psychological Society to develop psychologist CBT-i education opportunities, as well as registries of psychologists with experience and training in CBT-i.
|
Consider comorbid sleep condition/s
It is also important to consider the presence of comorbid sleep conditions, such as sleep apnoea,31 restless legs syndrome and circadian rhythm disorders.32,33 GPs can refer patients with suspected sleep apnoea who meet the self-report criteria for an overnight sleep study, or can refer patients to a sleep physician for further assessment.4
Sleep study or sleep physician referral
GPs can refer patients with a high risk of sleep apnoea for a home-based or laboratory sleep study with Medicare Benefit Schedule (MBS) items introduced in 2018 if they have an Epworth Sleepiness Scale score ≥8 and either an OSA50 score ≥5 or a STOP-Bang score ≥3.34,35 Referral to a sleep physician does not preclude concurrent assessment and management of insomnia in the general practice setting through a coordinated approach between the patient, GP and sleep physician.
Short-term insomnia
Although CBT-i is the recommended first-line treatment for insomnia, it does not provide immediate relief. Therefore, CBT-i may not be a suitable first-line approach for a small minority of patients presenting with severe short-term insomnia (eg persisting for less than two weeks) that is causing immediate and significant distress or impaired functioning. For example, among patients with very short-term insomnia caused by an obvious underlying sleep-disrupting precipitant such as acute bereavement, severe work stress or an acute medical episode, a short course of sleeping pills could be considered in order to provide more immediate relief from insomnia symptoms, combined with follow-up CBT-i if sleeping difficulties persist.15 Short-acting benzodiazepines and Z-drugs are efficacious for the short-term management of insomnia, but can increase the risk of withdrawal symptoms, including rebound insomnia upon rapid dose reduction or cessation.15 Orexin receptor antagonists may have a more favourable risk–benefit and dependence profile for insomnia management, but are not currently listed on the Pharmaceutical Benefits Scheme (PBS).36 Patients should be provided education about the risks of tolerance and dependence associated with sleeping pills, and a structured gradual withdrawal plan could be developed.17 Reconnexion is a Victorian benzodiazepine-dependence service (www.reconnexion.org.au/), with several online resources available to patients and clinicians throughout Australia.
The majority of patients presenting with insomnia that has lasted for more than one to two months will have developed patterns of more established insomnia that is maintained by underlying psychological and behavioural factors, and will therefore be more suitable for CBT-i.26
CBT-i from self-guided programs, GPs and/or practice nurses
It is expected that most general practice patients with insomnia symptoms will be suitable for CBT-i from an evidence-based online program, GP and/or practice nurse.
Therapist-delivered CBT-i has been translated to self-guided online programs.37 Several evidence-based online CBT-i programs are routinely available in Australia including through clinical trials (Box 2).26,38–40 Digital CBT-i programs are currently under active investigation in the Australian community and in primary care (Australian and New Zealand Clinical Trials Registry: ACTRN12622001463763).
GPs and/or practice nurses can administer CBT-i in the general practice setting (Table 1).41 A previous Australian Journal of General Practice article provides a detailed, manualised, step-by-step model for GP-delivered brief behavioural therapy for insomnia.25 GPs with Level 2 Focussed Psychological Strategies training with further specific sleep skills training can administer CBT-i with the additional mental health MBS item numbers.42 In collaboration with the General Practice Mental Health Standards Collaboration (GPMHSC), Flinders University is currently developing a CBT-i education program for GPs.
There is limited evidence to guide which patients are most suitable for different CBT-i options. Although face-to-face CBT-i from an experienced clinician yields slightly greater overall improvements in insomnia than other modalities, patient preference, clinician availability, cost, presenting symptoms/comorbidities/lifestyle factors and the shortage of specialist sleep clinicians should be considered.22 Some patients may have an immediate preference for online versus GP-delivered CBT-i versus referral to a psychologist. For example, people who work full-time may find it difficult to attend multiple weekly CBT-i sessions with a clinician. Self-guided programs can require more motivation to complete weekly sessions and enact treatment recommendations. GPs may wish to contact patients who are referred for online CBT-i after the first two weeks to provide motivational support and discuss treatment recommendations and strategies (ie enacting a hybrid therapist-guided online CBT-i approach).43 Patients who are not responding to either online or GP-delivered CBT-i may be considered for referral to a sleep psychologist or a sleep physician in the case of a suspected comorbid sleep disorder.
Assess requirement for psychologist referral
A minority of patients with insomnia may require personalised treatment from a psychologist or GP specialising in insomnia management. For example, patients with seizure disorders, a history of mania or a predisposition to psychiatric episodes may be suitable for specialist management instead of an automated online program or a manualised behavioural program (Figure 1).
Sleep problems occurring during the perinatal period may require investigation by a specialist sleep clinician. Sleep problems during the perinatal period may be due to a combination of conditioned insomnia and external factors that disrupt sleep quality and/or duration (eg sleep disruption caused by waking during pregnancy due to pain, discomfort and fetal movements; or during the postpartum period due to infant sleep–wake–feeding patterns disrupting sleep).44 Careful investigation of these underlying causes of sleep disruption can guide the appropriate choice of treatment components during the perinatal period.
Patients who drive or operate heavy machinery for work or report excessive daytime sleepiness may be more suitable for referral to a clinician with expertise in balancing the safety and effectiveness of bedtime restriction recommendations from week to week of CBT-i. This is due to the potential for increased daytime sleepiness during the initial weeks of bedtime restriction therapy and stimulus control therapy.
Shift workers may also require more nuanced treatment approaches that accommodate shift schedules (and, consequently, are contradictory to several treatment components of CBT-i, including regularisation of sleep timing and bedtime restriction therapy).45
Referral pathway to a sleep psychologist
Insomnia is an eligible condition for a GP Mental Health Treatment Plan (MHTP) referral, which subsidises the cost of psychology sessions.42 Despite this subsidy, sessions with a psychologist often incur a co-payment, which may be a barrier for many patients. Specialist sleep psychologists can often manage patients throughout Australia via telehealth consultations. There are sleep research and clinical institutes in most capital cities that include psychologists specialising in the management of sleep disorders. Education programs are being developed by the Australasian Sleep Association and Australian Psychological Society to increase the number of psychologists with CBT-i training and expertise.
Follow-up assessment of treatment response
Although CBT-i is the most effective treatment for insomnia, not all patients experience complete remission of insomnia following treatment. Self-report insomnia questionnaires, and sleep diaries can be useful clinical aids to reassess insomnia symptoms after treatment (Table 2).
Patients with persistent insomnia following online CBT-i or brief CBT-i delivered in general practice may be considered for referral to a sleep psychologist for more in-depth cognitive therapies. GPs may also consider referral to a sleep physician for assessment and the management of any suspected or confirmed comorbid sleep disorder that may be contributing to persistent insomnia symptoms (eg sleep apnoea, restless legs syndrome).
Conclusion
Insomnia is a highly prevalent and debilitating disorder that can be managed in Australian general practice (Box 3). CBT-i is the recommended first-line treatment for insomnia. CBT-i is effective in patients presenting with insomnia as an independent condition, insomnia comorbid with mental and physical health conditions and in the presence of sleeping pill use. Brief standardised tools to assess for insomnia are readily available for primary care clinicians to use, and patients can access evidence-based CBT-i through self-guided online programs, GPs or practice nurses or referral to psychologists (with an MHTP).
| Box 3. Practice points |
- Insomnia is a prevalent condition in general practice
- Insomnia assessment tools can be found on the Australian Sleep Association’s primary care sleep health resource
- Cognitive behavioural therapy for insomnia (CBT-i) is the recommended first-line treatment
- Insomnia is an eligible condition for a Mental Health Treatment Plan
- CBT-i can be delivered via self-guided online programs or suitably trained general practitioners, practice nurses and psychologists
|
Key points
- Insomnia is a prevalent and debilitating condition in Australian general practice.
- Insomnia can be treated in the presence of other mental and physical health conditions.
- The most effective treatment is CBT-i.
- GPs can assess patients for insomnia with brief standardised self-report instruments.
- CBT-i can be delivered through patient self-guided online programs, or suitably trained GPs, practice nurses and psychologists.