Neurogenic thoracic outlet syndrome (nTOS) is a condition involving chronic compression of the brachial plexus. It is the most common of all thoracic outlet syndromes (TOS), accounting for approximately 97% of cases.1,2 This can result in a spectrum of symptoms from mild pain in the arm and shoulder on excessive use to disabling motor wasting and sensory disturbance at rest. nTOS frequently occurs in individuals in their second to fourth decades of life, with 70% of those affected being female.2 The estimates of the incidence of this condition vary widely, but a recent study reported three cases per year per 100,000 population in the US.2 Timely diagnosis and management are key, with time from symptom onset to therapy affecting patient outcomes.3
Objective
This article reviews the presentations, assessment pathways and management options for nTOS.
Clinical presentation and common differential diagnoses
The primary presenting symptom of nTOS is usually pain and paraesthesia of the affected upper limb without any localisation to a specific nerve distribution.4 Radiation of pain into the neck, shoulder and thoracic region of the back is common. Patients will likely describe exacerbation of symptoms following activities that require elevation of the arms above the head (eg hanging clothes, brushing hair) or at night, if the individual sleeps with the arm positioned overhead. Headache is common in nTOS and is likely due to secondary spasm of the paraspinal and trapezius muscles.5
A history of neck trauma is common among patient with nTOS. Neck trauma may be in the form of a single episode of neck extension (ie ‘whiplash injury’) or chronic injury in the form of repetitive strain injury.6,7 These chronic injuries classically occur with activities that either stretch the brachial plexus (eg driving with arms unsupported) or crowd the scalene triangle (eg activity with arms overhead).
On physical examination, patients will typically have tenderness at the point of plexus compression, the scalene triangle in the supraclavicular space or at the pectoralis minor insertion site at the coracoid process.8 Palpation at these areas may also reproduce neurological symptoms down the arm due to inflammation of the brachial plexus. Patients with long-standing or severe nTOS may present with motor disturbance and hand muscle wasting.
The patient should be assessed to exclude other pathologies that may be causing the presenting symptoms.9 Common differential diagnoses include degenerative cervical disc disease, cervical arthritis, rotator cuff tendinitis and carpal tunnel syndrome.4,7
Pathophysiology
nTOS is a compressive brachial plexopathy, often caused by the combination of predisposing anatomical features and triggered by the abnormal sequelae of neck trauma.
The brachial plexus is formed by spinal nerve roots C5 through T1, which interconnect as they pass through the thoracic outlet to the upper limb. The plexus nerve roots pass through the scalene triangle, which is bordered by the anterior and middle scalene in the neck along with the first rib at the base (Figure 1).10,11
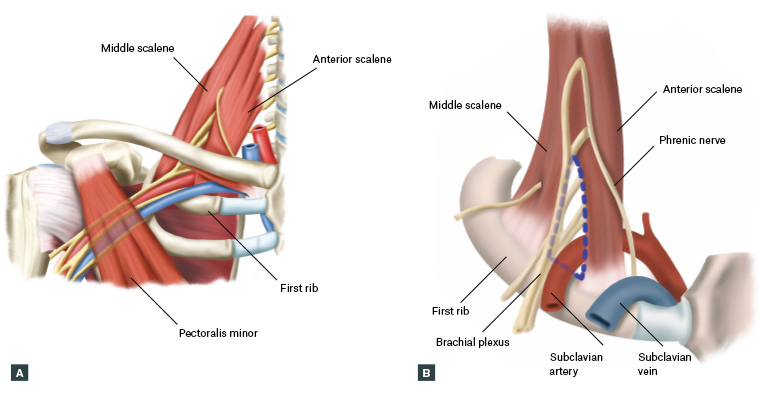
Figure 1. Diagrams showing A. the course of the brachial plexus, subclavian artery and vein through the thoracic outlet and
B. the anterior and middle scalene muscles, which, together with the first rib, form the borders of the scalene triangle (blue dashed line). Click here to enlarge
Patients with nTOS often have anatomical characteristics that make them more susceptible to ‘crowding’ of the brachial plexus within this triangle (Table 1). However, these anatomical variations are frequently found in the normal population, and less than 10% of patients with these features develop nTOS.12,13 These predisposing anatomical features are often insufficient to cause nTOS, but appear to lower the threshold towards developing nTOS in patients who experience neck trauma.
| Table 1. Anatomical features that predispose to neurogenic thoracic outlet syndrome |
| Musculofascial |
Narrow scalene triangle
- Less space for the brachial plexus to pass through
|
Scalene minimus muscle
- Extra muscle that passes between various roots of the brachial plexus
|
Fascial bands
- Passing across or between individual nerve roots
|
| Skeletal |
Cervical rib
- Extra rib off T1, present in 0.5–1.5% of the population4,7,8,31
|
Hypoplastic first rib
- First rib that lies higher in the neck and attaches to the second rib
|
Previous trauma
- Anomalies of the first rib with a thickened callous
|
Neck trauma can result in injury and inflammation of the scalene muscles, leading to adaptive changes. Histological assessment of scalene muscles from those with nTOS has shown chronic tissue remodelling, with significant muscle fibrosis and the predominance of type 1 (slow-twitch) muscle fibres.14,15 These changes culminate in brachial plexus compression in an already ‘crowded’ thoracic outlet. The result is temporary or permanent neurological dysfunction.
Diagnostic tests and imaging
There are numerous physical and imaging tests that demonstrate these anatomical features of nTOS and elicit symptoms of brachial plexus compression.
Provocative manoeuvres can be used to reproduce symptoms of nTOS and some common differential diagnoses (Table 2).8 The Elevated Arm Stress Test (Roos test) and Upper Limb Tension Test (Elvey test) have both been reported to have a high sensitivity of 85–94%.4,8 However, these manoeuvres, when performed in isolation, have poor sensitivities and half the normal population will test positive on either test alone .16,17 Positive results on these provocation manoeuvres are even more common in patients with cervical radiculopathy or carpal tunnel syndrome.17,18 Tests such as Spurling’s test and Tinel’s test are helpful for differential diagnoses.9,18,19
Several selected imaging and interventional tools can help rule out common differential diagnoses (Table 3). No single imaging test can ‘rule in’ nTOS. However, evidence of anatomical features (eg a cervical rib) may increase the treating clinician’s suspicion of the diagnosis. Other pathologies found during work-up (eg cervical nerve root compression) should be investigated and treated prior to any intervention for TOS.
| Table 2. Provocation manoeuvres in the diagnosis of neurogenic thoracic outlet syndrome |
| Test |
Purpose |
Description |
| Elevated Arm Stress Test (Roos test)4,9 |
Assess for nTOS |
- Patients place their arms in the ‘surrender’ position and repetitively open and close their fists for three minutes
- Reproduction of symptoms in the affected limb suggests nTOS
|
| Upper limb Tension Test (Elvey test) 4,9 |
Assess for nTOS |
- Arms are abducted to 90° with the elbows extended. Patients are asked to dorsiflex and tilt their head with their ear to their shoulder contralateral to the affected limb
- Reproduction of symptoms in the affected limb suggests nTOS
|
| Spurling’s test18 |
Assess for cervical nerve root compression |
- Passive cervical extension with rotation to the affected side with axial compression
- Radicular pain suggests cervical nerve root compression
|
| Tinel’s test |
Assess for carpal tunnel syndrome |
- Percussion of the median nerve at the wrist
- Paraesthesia along the median nerve distribution suggests carpal tunnel syndrome
|
| nTOS, neurogenic thoracic outlet syndrome. |
| Table 3. Diagnostic tests that can be performed in the diagnosis of neurogenic thoracic outlet syndrome |
| Test |
Purpose |
| Chest X-ray |
Assess for cervical/hypoplastic first rib or other skeletal abnormalities |
| Nerve conduction studies |
Investigate for peripheral nerve compression syndromes |
| MRI cervical spine |
Investigate for cervical spine disease with nerve root compression |
| MRI shoulder |
Investigate for rotator cuff injury |
| MRI brachial plexus (with provocation manoeuvres) |
Investigate for obvious compression of the brachial plexus on provocation |
| Anterior scalene muscle block |
Relax and resolve spasm of the anterior scalene muscle to relieve compression of the brachial plexus |
| MRI, magnetic resonance imaging. |
Anterior scalene muscle block with the injection of a local anaesthetic may be a particular valuable diagnostic test for nTOS. Temporary relief with injection is positively correlated with a diagnosis of nTOS and good relief from thoracic outlet surgery.19,20 In observational studies, positive outcomes after surgical treatment of nTOS have been reported in over 90% of block respondents, compared with 38–50% of non-respondents.20,21 Botulinum toxin injection into the scalene anterior can offer similar relief to local anaesthetic block, with a prolonged effect of up to three months.22
Management and outcomes
After thorough assessment and investigations (Figure 2), patients diagnosed with nTOS can be managed by a multidisciplinary team comprising the general practitioner, physiotherapist and surgical specialist. The initial management of nTOS is primarily through specialist physiotherapy with a practitioner experienced in the disorder.20,23,24 This is often combined with neuromodulating analgesic agents and psychosocial support. nTOS physiotherapy differs significantly from that for disorders of the neck, shoulder and upper extremity, and primarily focuses on areas of brachial plexus compression. Most patients with mild nTOS or those in whom therapy was started soon after symptom onset will have significant improvement.23 Long-term symptom relief (>12 months) and return to work has been reported in 59–88% of nTOS patients managed conservatively.22,23 Selected patients who have a poor response to conservative management can be considered for further intervention.
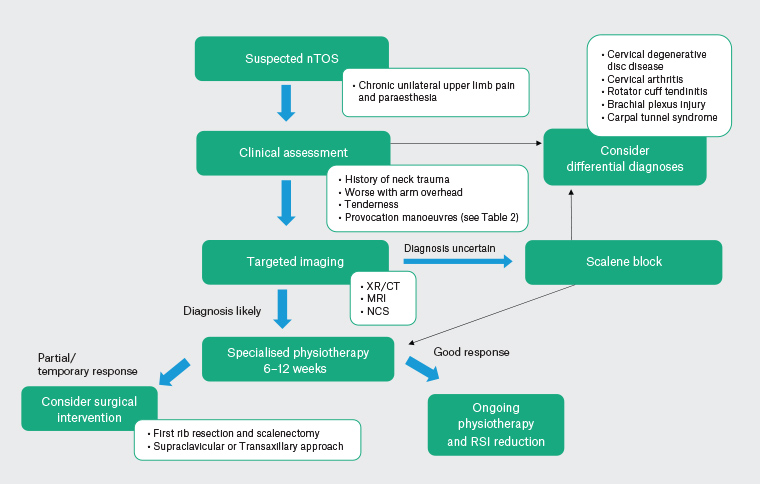
Figure 2. Proposed neurogenic thoracic outlet syndrome (nTOS) work-up and treatment algorithm. Click here to enlarge
CT, computed tomography; MRI, magnetic resonance imaging; NCS, nerve conduction studies; RSI, repetitive strain injury; XR, X-ray.
In addition to its aforementioned role as a diagnostic test, botulinum toxin injection in the scalene muscles has been proposed as a treatment modality for nTOS, but did not demonstrate significant improvement in pain, paraesthesia or function compared with placebo in a randomised controlled trial.25
Patients with nTOS with significant persistent symptoms requiring a more permanent solution are considered for surgical management. In Australasia, nTOS is predominantly managed by vascular surgeons, with some spinal and thoracic surgeons also offering intervention. Decompression of the brachial plexus can be achieved through first rib resection, along with anterior scalenectomy. This is done primarily via a supraclavicular or, occasionally, transaxillary approach. Many surgeons prefer a supraclavicular approach because it allows for concurrent thorough brachial plexus neurolysis. Those patients with a cervical rib classically will have both the cervical rib and the first rib removed within the same procedure. Patients with evidence of compression in the subpectoral space may benefit from an accompanying pectoralis minor tenotomy. In a meta-analysis of 10 observational studies, 56–89% of patients with nTOS had symptom improvement after surgery.26 Among the patients with nTOS who did not respond to initial physiotherapy, a recent randomised controlled trial showed that decompressive surgery was more effective than ongoing conservative management in improving symptoms and function in the short term.27 The risks of thoracic outlet surgery include brachial plexus injury (<1%), phrenic nerve injury (<1%), major vascular injury (1%), chyle leak (1–3%), pneumothorax (5%) and recurrent symptoms (2-4%).28–30 Physiotherapy should continue postoperatively to allow the patient to return to an optimal level of function.
Conclusion
nTOS can be a disabling disorder and predominantly affects younger women. Patients presenting with chronic upper limb neurogenic symptoms may warrant the clinician to consider nTOS as a potential differential diagnosis. Early referral and diagnosis are critical to achieving optimal outcomes for these patients.
Key points
- nTOS is the most common form of TOS, but often the most challenging to diagnose.
- The diagnosis of nTOS is primarily clinical, with imaging primarily used to exclude other differential diagnoses.
- Common differential diagnoses include cervical disc herniation, peripheral nerve compression syndromes, rotator cuff pathology and spinal canal stenosis.
- Affected patients often have predisposing anatomical factors, with the onset of symptoms following an inciting neck trauma.
- Initial management of nTOS usually consists of focused physiotherapy, with first rib resection considered in selected cases.