This paper was prepared on behalf of the Primary Care Collaborative Cancer Clinical Trials Group
Cancer is the leading cause of disease burden in Australia.1 Primary care has an important role across the cancer continuum.2 General practice is essential for the prevention and early detection of cancer.2,3 The scope of involvement that general practitioners (GPs) and general practice have in cancer survivorship has continued to grow and evolve.4,5 Consequently, general practice has a critical role in the coordination of care, management of cancer and multimorbidity and the secondary prevention of cancer.5
To support this growing role, since 2009, Cancer Australia has funded the Primary Care Collaborative Cancer Clinical Trials Group (PC4) through their Support for Clinical Trials Program. The aim of this support is to build industry-independent cancer clinical trial protocols based in primary care, particularly in general practice. PC4 is part of the Department of General Practice at the University of Melbourne.
Despite the importance of a robust primary healthcare system, primary healthcare research continues to be undervalued and under-resourced.6 This continues, despite it being a medical research and innovation priority for 2022–24 for the Medical Research Future Fund.7 Primary care research continues to receive limited investment and poor representation in successful research grant funding.6,8 This disparity in research investment and resourcing is also seen internationally.9,10
Clear research priorities are important to target the development of new studies that have the greatest potential benefit and impact because funding, resources and capacity are limited or fragmented.8,11 The aim of this prioritisation study was to identify the top cancer research priorities relevant to general practice across the cancer continuum, from prevention to palliative care, in Australia. The goal was to generate evidence that could be used to inform the development of future research developed by PC4.
Methods
This prioritisation study was guided by an adapted nominal group technique. The method was informed by the James Lind Alliance (JLA) guidebook,12 where the approach involves shared voting or ranking, with further structured small group discussions followed by a final ranking or voting. The ranked orders for each item from each group are totalled and final priorities are selected. We adapted this method based on research by Badrick et al13 and Rankin et al14 to include wider consultation with stakeholders through a scoping survey and prioritisation validation survey. In addition, to assist with small group discussions and ranking, we created a tailored scoring rubric. The study was approved by the University of Melbourne. The Cancer Care Continuum was used as a framework to categorise priorities.3 This well-established framework covers cancer control and care from prevention through to palliative care.
Prioritisation involved five phases (Figure 1):
- Identification of existing priorities through a literature review
- National stakeholder consultation to identify priorities in local settings
- Preliminary expert review using the findings from the previous steps to refine and consolidate priorities
- To ensure initial priority ranking was reflected by other stakeholder groups, a second online survey to validate the priorities identified is conducted
- A final prioritisation workshop with members of PC4’s Advisory Committee, Scientific Committee and Community Advisory Group

Figure 1. Method used to identify and rank research priorities. Click here to enlarge
PC4’s Scientific Committee is a national multidisciplinary expert group of more than 20 members, including eight academic GPs, academic primary care and cancer nurses, medical oncologists, epidemiologists, exercise physiologists, implementation scientists, policy makers and consumers. Members join the Scientific Committee through a competitive expression of interest process, where their skill and expertise are reviewed by PC4’s Advisory Committee. The Community Advisory Group includes nine members with a lived experience of cancer or a carer or family member of a person who has had cancer.
Step 1: Literature review
A broad search strategy (Appendix 1) was used for Medline, Embase, Emcare and PsycInfo to identify papers describing cancer research priorities, not limited to primary care, published in English between January 2010 and February 2020. Using Covidence (Veritas Health Innovation, Melbourne, Australia), two researchers (KM, PD) independently screened papers and extracted priorities and descriptive data that included author, publication year, country, population of interest, cancer type/s and stakeholder group/s consulted. The review and interpretation of the research priorities were framed around whether the described priority currently includes or could include a role for general practice and/or primary care health professionals. To be eligible for inclusion, papers describing cancer research priorities needed to be conducted in a high-income country similar to Australia. Priorities that described research that clearly did not or was unlikely to involve general practice and/or primary healthcare professionals were excluded. A consensus approach with a third researcher (JDE), an academic GP, was used to resolve conflicts.
Step 2: Priority identification survey
To supplement the priorities identified through the literature search, an online survey for stakeholders was developed in Research Electronic Data Capture (REDCap)15,16 in consultation with the Scientific Committee expert group. A second survey for the public was developed in consultation with the Community Advisory Group. A snowballing approach was used to promote the priority identification survey nationally. It was promoted via Twitter and PC4’s email member newsletter, which has an audience of over 700 members. Members of the Scientific Committee shared the survey with their professional networks. In addition, email invitations were sent to external stakeholder groups such as Australian-based cancer clinical trial groups, consumer organisations, primary health networks, academic primary care professional bodies and cancer services.
Step 3: Preliminary expert review, consolidation and ranking
Priorities identified from the existing literature and survey were combined by two researchers (KM, PD). These combined priorities were categorised using the Cancer Care Continuum as a framework.3 Priorities were allocated to one of five domains: prevention, early detection (including cancer screening), survivorship, palliative care, or cross-cutting research.2 Cross-cutting research priorities spanned across areas of the continuum, different healthcare groups and different healthcare settings. Priorities specifically limited to the acute cancer treatment phase, which did not include aspects such as ongoing management of comorbid conditions, management of long-term effects of treatment and management of toxicities related to treatment, were excluded from the prioritisation exercise because they are outside the scope of PC4’s research remit. Expert working groups for each of the five domains were established where members of PC4’s Scientific Committee self-selected into one or more working groups. Priorities were discussed by working groups in two to three one-hour Zoom meetings. Each group then discussed the language and intent of the priorities and, where appropriate, refined the priority to improve the clarity around the role of primary care or consolidated similar priorities. A weighted ranking rubric was developed, guided by considerations for developing useful clinical research outlined by Ioannides.17 The first question was used as a screening question, where priorities listed as ‘no’ were not further discussed. Working groups provided responses for all questions except question five, which was only answered by the Community Advisory Group. The weighting (%) was allocated through internal discussions of the research team and is provided in parentheses in the list below.
- Would the research and its methods fit within PC4’s research strengths and scope?
- Is this priority big/important enough to fix? (15%)
- Is there enough existing evidence that already addresses this priority? (10%)
- Does the priority reflect real life? (15%)
- Does the priority reflect top patient priorities? (20%)
- Would addressing this priority be worth the money? (15%)
- Can addressing this priority be feasibly conducted? (15%)
- Does this priority target a low participation group or group with poorer outcomes? (10%)
Each group then used the above rubric to rank all priorities and select a top 10. When more than one priority was ranked in 10th position, individual members of the working group and the Community Advisory Group were asked to vote. The final top 10 priorities based on their score, in each domain, were reviewed at a Scientific Committee meeting before moving forward with developing the priority validation survey.
Step 4: Priority validation survey
To validate the top 10 priorities from each domain, we used an allocation survey where respondents were asked to allocate $100 of theoretical funding between the priorities, according to established procedures.14,18 The distribution of funds was then used to re-rank the priorities. We used a paid feature of SurveyMonkey to ensure greater community involvement by collecting a minimum of 300 complete responses from the Australian general population, limited to people in Australia aged over 18 years who answered ‘yes’ to the initial screening question:
Do you have a lived experience with cancer? A lived experience of cancer could be that a person has had cancer, is living with cancer, knows or cares for someone who has, or had cancer, and/or has an interest in cancer research and helping people.
The language within the community survey was developed in consultation with the Community Advisory Group. In addition, the survey was promoted to primary care stakeholders similar to the process described above. To minimise order effects, priorities were randomly ordered for each participant.
Step 5: Final ranking
A final workshop was held (25 May 2021) to review the results of the validation survey to discuss and finalise the top three priorities for each area of the continuum. This workshop included working group members, but also new participants who were members of PC4’s Advisory Committee (Appendix 2).
Results
In Step 1, we identified 218 priorities (Appendices 3 and 4) in the literature. The survey used in Step 2 helped identify an additional 93 priorities. Nearly two-thirds of these 311 research priorities were focused on either cancer early detection or survivorship (Figure 2). Fifty-three people responded to the survey: nine consumers and 44 primary care/cancer professionals (Table 1). Respondents were predominantly from Victoria and New South Wales, with half the professionals working within a local health district and three-quarters of respondents having at least five years’ clinical experience.
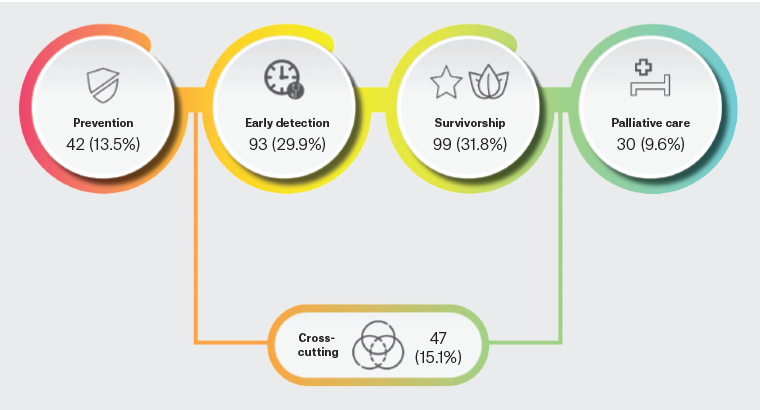
Figure 2. Initial priorities identified across each domain of the cancer continuum (Steps 1 and 2). Click here to enlarge
| Table 1. Participant demographics for initial priority identification survey and resource allocation survey (combining all stakeholder groups) |
| |
Priority identification survey (n=53) |
Resource allocation survey (n=388) |
| State/territory |
|
| Australian Capital Territory |
0 (0) |
5 (1.3) |
| New South Wales |
16 (30.2) |
111 (28.6) |
| Northern Territory |
0 (0) |
2 (0.5) |
| Queensland |
4 (7.5) |
72 (18.6) |
| South Australia |
6 (11.3) |
44 (11.3) |
| Tasmania |
1 (1.9) |
15 (3.8) |
| Victoria |
24 (45.3) |
113 (29.1) |
| Western Australia |
2 (3.8) |
26 (6.7) |
| Profession |
|
|
| Consumer |
9 (17) |
337 (86.9) |
| General practitioner |
3 (5.7) |
12 (3.1) |
| Primary care nurse |
0 (0) |
1 (0.3) |
| Academic researcher |
14 (26.4) |
20 (5.2) |
| State government employee |
9 (17) |
2 (0.5) |
| Representative of: |
|
|
| PHC/cancer-related NGO |
4 (7.5) |
2 (0.5) |
| Hospital or secondary/tertiary care provider |
5 (9.4) |
5 (1.3) |
| Patient or consumer association |
0 (0) |
2 (0.5) |
PHC research association or research institute |
0 (0) |
1 (0.3) |
| Other |
9 (17) |
6 (1.5) |
| Organisational roleA |
|
|
| Employee |
16 (36.4) |
31 (60.8) |
| Project leader |
12 (27.3) |
7 (13.7) |
| Working group/department head |
8 (18.2) |
5 (9.8) |
| Head of the organisation |
3 (6.8) |
2 (3.9) |
| Other |
5 (11.4) |
6 (11.8) |
| LevelA |
|
|
| Local/regional |
24 (54.5) |
32 (62.7) |
| State |
13 (29.5) |
9 (17.6) |
| National |
4 (9.1) |
7 (13.7) |
| International |
3 (6.8) |
3 (5.9) |
| Speciality areaA,B |
|
|
| Epidemiology |
8 (7.4) |
9 (8.9) |
| Prevention |
16 (15.1) |
13 (12.9) |
| Early detection |
18 (17.0) |
12 (11.9) |
| Treatment |
22 (20.8) |
20 (19.8) |
| Survivorship |
24 (22.6) |
28 (27.7) |
| Palliative care |
18 (17.0) |
19 (18.8) |
| ExperienceA,C (years) |
|
|
| <1 |
2 (4.5) |
2 (5.0) |
| 1–5 |
9 (20.5) |
6 (15.0) |
| 5–10 |
11 (25.0) |
16 (40.0) |
| >10 |
22 (50.0) |
16 (40) |
Data are presented as n (%).
AResponses from healthcare professionals only, where the level indicates at what jurisdictional level the respondent fulfils the majority of their work activities.
BRespondents could select all that applied.
CAnswered by respondents with at least one speciality.
NGO, non-governmental organisations; PHC, primary healthcare. |
The top 10 priorities in each domain of the continuum (Step 3) were then validated. We received 388 responses (337 consumers, 51 healthcare professionals; Table 1; Step 4).
Figure 3 summarises the final results, outlining the top three priorities for each domain. Appendix 2 summarises the results of Steps 3–5 to achieve the final ranking shown in Figure 3. The top priorities for cancer prevention related to interventions to test prevention strategies for breast, ovarian and colorectal cancer, as well as personal risk communication. Early detection priorities focused on reducing disparities in screening and improving the pathway and time to diagnosis in patients who present symptomatically. Survivorship priorities included strategies for detecting cancer recurrence, to influence behaviour change and tools for assessing different aspects of survivorship. The resource allocation, Step 4, impacted the priority ranking particularly for survivorship and palliative care priorities, where some initially lower-ranked priorities were upvoted and influenced discussions and ranking during the final workshop (Appendix 5, available online only). Palliative care priorities related to service setting, location, availability and improvement. Lastly, cross-cutting priorities were about the overall improvement of the quality of cancer care, including the implementation of models such as patient navigation and models to manage psychosocial needs of rural patients.
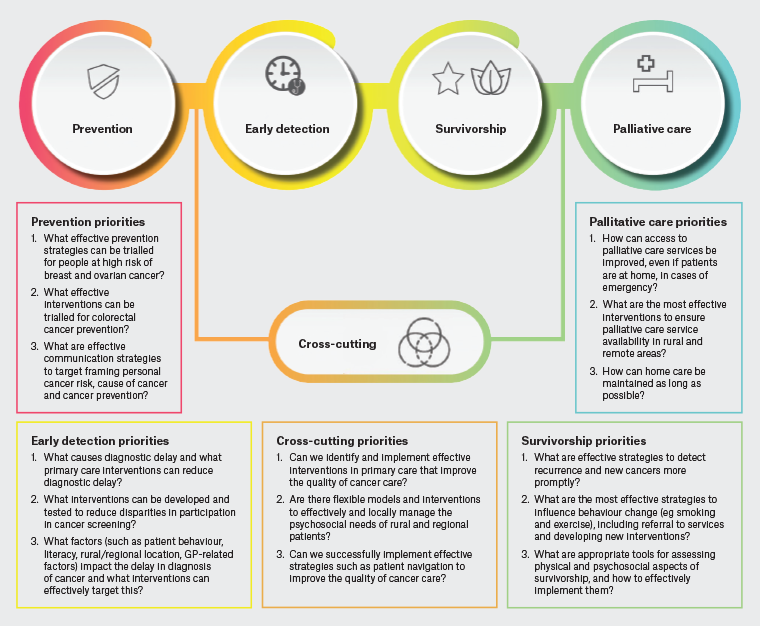
Figure 3. The top 15 cancer in general practice research priorities across the cancer continuum. Click here to enlarge
GP, general practitioner.
Discussion
This is the first Australian-based study to identify cancer research priorities in primary care across the continuum from prevention to palliative care. By including a literature review, expert review and national survey, the study has attempted to create a robust approach that gathered a wide range of priorities and input from multiple sources to inform the development of future research by PC4. It might provide evidence for researchers, funding bodies and the primary care sector to focus the investment of money, time, labour and skill into research development in priority areas with the goal of improving outcomes for Australians at risk of cancer or living with and beyond cancer.
The current limited literature describing cancer-related research priorities in primary care has focused on a single area of cancer research, such as genetic testing,19 or specific continuum domains, such as early detection13 or survivorship.20 The present study provides a broader view of priorities across the cancer continuum, outside the acute treatment phase.
In cancer prevention and early detection, Hamilton et al19 identified the need to move beyond descriptive research related to cancer genetic testing in primary care and that important research gaps included effective patient–provider communication about genetic risk and genetic testing, which is partially encompassed within our priority around effective communication strategies for framing personal cancer risk. Focusing directly on early detection of cancer, Badrick et al13 identified the need for new screening tests for cancers that are not currently screened for. This contrasts with the focus of the screening priority identified in our study, to reduce disparities in participation for existing screening programs. Both Hamilton et al19 and Badrick et al13 identified the need to further explore factors that influence patient decisions to report symptoms of cancer early.
There are five key domains in the cancer survivorship care quality framework developed by Nekhlyudov et al.21 The results of our study map to the domains of recurrences and new cancers, health promotion, physical effects and psychosocial effects.21 To better integrate primary care into cancer survivorship, Nekhlyudov et al suggested future research needs to focus on models of care in different settings, which was also identified in our cross-cutting research priorities, and better addressing the role of primary care within these models.20 Jaffee et al22 similarly suggest that future health services research should address the need for better models of survivorship care, particularly shared care between primary care and specialists, which is reflected in the US blueprint for cancer research.23 Our results appear to highlight the importance of cancer survivorship to stakeholders with twice as many survivorship priorities identified compared with other areas of the cancer continuum. This is reflected locally by the cancer charity Cancer Council Australia, which has invested more in survivorship research. In 2020, Cancer Council Australia invested $54 million into cancer research, over 50% of which was awarded to survivorship research.24 This is not necessarily mirrored in cancer research funding more broadly, because only 8% of funding is awarded to research focused on cancer control, survivorship and patient outcomes.25 A recent Australian general practice priority setting study conducted ranking of disease-specific priorities.26 Cancer, including treatment and survivorship combined together, ranked ninth out of 24 items, behind mental health, chronic pain and alcohol and substance abuse disorders as the top three placed priorities.26 Our first ranked survivorship priority, namely ‘What are effective strategies to detect recurrence and new cancers more promptly?’, maps closely to the Clinical Oncology Society of Australia’s (COSA) current survivorship research priorities, outlined in the study by Crawford-Williams et al.27 The priorities from Crawford-Williams et al were also mapped to the cancer survivorship quality care framework.21 In that study, the cancer recurrence and progression was the highest-ranked physiological outcomes priority, fear of recurrence was the highest-ranked psychosocial priority, research focused on rarer or under-represented cancers was the highest-ranked population group priority and, finally, quality of care was the highest-ranked health services priority.27
In terms of palliative care, a priority that was retained from the literature review to our final top three priorities was about strategies that can support patients to receive home care for as long as possible. This priority was originally identified by Sakashita et al when scoping research questions for bereaved family members of palliative care cancer patients in Japan.28
Our sampling strategy was designed to identify healthcare professionals, researchers and consumers who could provide an informed perspective relating to cancer services and the role of primary care. We looked to improve community engagement by ensuring a minimum number of responses, but this impacted results by over-representing this community stakeholder group compared with healthcare professionals. Because this prioritisation exercise was undertaken to inform PC4’s research priorities, the final ranking was conducted by an expert panel, which allowed PC4 to take into consideration the over-representation of community responses when discussing priorities during the final ranking workshop. In addition, the types of healthcare professions represented might have contributed to the number of survivorship priorities identified. For example, some disciplines, such as nursing, might be more likely to place higher importance on survivorship, whereas oncologists often focus on acute cancer treatment,29 which was not included in the scope of this study. There is strong representation of healthcare professionals working in cancer survivorship among the members of PC4. A possibility to mitigate this could have been the inclusion of an open-ended question within the resource allocation survey to identify why respondents allocated their funding as they did.30 Lastly, a limitation in the interpretation of these results is the representation and applicability of the priorities in a rural or regional setting. We did not capture survey respondent location apart from state or territory. Although members of the expert group are involved in developing cancer in primary care research focused on or including rural and regional settings, the representation might not have been enough to adequately tease out the difference in research needs between settings to impact wording and scope within individual priorities.
The current literature on cancer research priority studies has a wide scope, with a broad range of approaches and levels of stakeholder consultation, but often with a strong focus on basic science or hospital-based research and care.22,23,27,31–38 The involvement of primary care in establishing priorities or the consideration of the role of primary care, for general practice, has often been poorly described.33,36–40 The present prioritisation study, led by a primary care research-focused organisation, is therefore important because research conducted in hospital settings is generally not applicable to general practice or to patients in general practice.8,26,41
An additional strength of the present study is that it combined priorities already defined in the literature with those from a wide range of stakeholders and attempted to elicit national engagement from healthcare professionals working in different healthcare settings. This approach produced priorities that articulated broad overarching concepts, as well those with a narrow focus, which made discussions during ranking more difficult. During review by expert working groups, the consolidation of priorities aimed to strike a balance between creating a more feasible list to rank while still retaining the sentiment and language of the original submissions.
This exercise has identified key priority areas in the primary care cancer research field. It provides a framework to underpin the development of new, targeted research planning for a national collaborative cancer in the primary care clinical trials group, PC4. It could be used to inform wider research development and funding to improve the quality of care and outcomes for Australians at risk of cancer or living with and beyond cancer. These results could be used by funding bodies and policy makers to inform discussions about future investment to ensure value for money and to maximise the impact of research outcomes.