Australians commonly have significant ultraviolet (UV) radiation solar damage due to our Southern Hemisphere geography and the high population prevalence of fair skin types (ie Fitzpatrick types I–II). The degree of solar damage is proportionate to the risk of skin cancers. Many patients present with actinic keratoses (AKs), either as individually clinically discrete lesions or field disease. These AKs can eventually give rise to keratinocyte cancers (KCs), in particular squamous cell carcinomas (SCCs) and perhaps basal cell carcinomas (BCCs) as well. According to Bettering the Evaluation and Care of Health (BEACH) data from 2000 to 2016, approximately 5% of all Australian general practitioner consultations were skin cancer related, with approximately 30% of these involving AK management.1,2
A spectrum of keratinocyte dysplasia and neoplasia exists, ranging from a mildly dysplastic AK (keratinocyte intraepithelial neoplasia I [KIN I])3 to poorly differentiated, invasive SCC. Not only does differentiating the lesions in the middle of this spectrum pose a diagnostic dilemma but multiple lesions across the spectrum of dysplasia/neoplasia might be present in a given field.
‘Field cancerisation’ is at the severe end of the solar damage spectrum, where there is multifocal clinical atypia characterised by AKs and/or SCC in situ (with or without invasive disease) occurring in a skin field exposed to chronic UV radiation.4 The natural history of AKs can vary, and lesions might spontaneously disappear, persist or progress to invasive SCC. Typically, thicker AKs have a greater risk of progression to invasive cancer.5
Aim
This article will discuss an approach to managing patients with significant solar damage from a primary care perspective, focusing on the assessment and treatment of AKs as individual lesions and within a field.
Assessment of a patient with significant solar damage
Assessment includes focused clinical history assessing skin cancer risk (Table 1) and collateral history (if available) for lesions in areas not visible to the patient. When reviewing specific concerns, ‘SCAN’ (Sore, Changing, Abnormal and New) is a useful acronym for lesion-specific history-taking and patient education regarding ongoing self-assessment (Table 2).6 As the patient’s hands and face are usually uncovered during the consultation, a quick preliminary visual assessment of these areas can be conducted. Solar damage assessment can be undertaken opportunistically or performed when patients present with concerns regarding a specific skin lesion or requesting a skin check.
| Table 1. Focused clinical history for assessing solar damage and risk |
| Risk assessment history |
Relevant history to consider and elicit |
| Previous skin cancer history |
What type(s), when, where, age at first diagnosis (particularly for melanoma) |
| Family history of skin cancers |
First-degree relatives with melanoma aged ≤40 years at diagnosis, genetic syndromes (eg xeroderma pigmentosum, Gorlin–Goltz/basal cell naevus syndrome) |
| Previous treatments |
Surgery/excisions, cryotherapy, previous non-surgical treatments (eg topical, PDT, immunotherapy/targeted therapy, radiotherapy) |
| Immunosuppression |
CLL, AIDS, OTR, autoimmune disease medication (eg azathioprine, cyclosporin, methotrexate), biologics for rheumatoid arthritis and psoriasis |
| Surgical bleeding risk |
Antiplatelets and anticoagulants, any previous significant intraoperative or postoperative haemorrhage or haematoma formation |
| Implantable electronic devices |
Risk when using monopolar diathermy during procedures (eg pacemaker, defibrillator, cochlear implant, deep brain stimulator) |
| Allergies/intolerance |
Antibiotics, latex, intolerance to previously used field treatments, needle phobias, previous vasovagal episodes |
| Infection risk |
Type 2 diabetes, previous surgical site infections, previous MRSA infection/carrier |
| Recreational UV exposure |
Outdoor activities/sports (particularly long duration; eg golf, tennis, cricket, swimming, running), sunbathing practices, solarium use; specifically ask about previous blistering sunburns, especially at younger age |
| Occupation risks |
Outdoor worker (eg construction, agricultural, mining, transportation, police, firefighter, defence force, lifeguard and other on or near water occupations), welding (UVC radiation exposure), work with arsenic or coal tar |
| AIDS, acquired immunodeficiency syndrome (secondary to human immunodeficiency virus infection); CLL, chronic lymphocytic leukaemia; MRSA, methicillin-resistant Staphylococcus aureus; OTR, organ transplant recipient; PDT, photodynamic therapy; UV, ultraviolet; UVC, ultraviolet C. |
| Table 2. SCAN approach to lesion specific history6 |
| Lesion-specific history |
Symptoms and appearance |
| S – Sore or SymptomaticA |
Bleeding, itchy, tender, scaly and not resolving after 6 weeks |
| C – Changing and/or ConcernB |
Change in size, shape, colour or texture over time (weeks to months) – any lesion that is a patient concern needs to be examined carefully and, unless an unequivocal benign lesion, needs close follow-up or biopsy |
| A – Abnormal |
Looks different to the surrounding lesions or ‘stands out’ – clinically also known as an ‘ugly duckling’ |
| N – New |
Recently noticed lesion that has not resolved typically by 4–6 weeks – any new ‘mole’ after the age of 40 should be carefully examined |
AThe author has added ‘or Symptomatic’ to the established ‘SCAN’ approach.
BThe author has added ‘and/or Concern’ to the established ‘SCAN’ approach.
Adapted with permission from Skin Cancer College Australasia. Check your skin. SCAN Your Skin 2022. |
A full-body skin examination should follow a systematic physical exam technique so that all available skin can be examined.2 Covered areas should be enquired about and examined with patient permission if there is patient concern.
Examination of each lesion should include inspection (with good illumination and magnification if required), palpation and dermoscopy. When observing initially with the naked eye, the lesion should be considered individually and in the context of the ‘field region’. Dermoscopy has been found to significantly increase the diagnostic specificity and sensitivity of the trained clinician.7–11
Both benign and malignant hyperkeratotic lesions may be difficult to tell apart. See table 3 for a list of features present in common hyperkeratotic lesions that may be present on examination to help decide what the diagnosis is more likely to be and to help guide management.
| Table 3. Examination features of AKs, KCs and some common hyperkeratotic skin lesions in patients with significant solar damage10,11 |
| Lesion |
Inspection |
Palpation |
DermoscopyA |
| AK |
- Scale
- Erythematous background
- ‘Dull’ complexion
- Might be hyperkeratotic
|
- Rough
- Sandpaper like
- Usually non-tender
|
- Scale
- Four-dot clods (rosettes)
- White circles on an erythematous background in non-pigmented AK (strawberry pattern) or white circles on a pigmented background in pigmented AK
- Pigmented facial AKs might share lentigo maligna clues: grey dots/annular-granular structures
|
| SCC |
- Hyperkeratotic (well-differentiated lesions)
- Raised – nodular or plaque like
- Pink, vascular ‘fleshy’ in poorly differentiated
|
- Raised
- Firm
- Tender
- Might be indurated signifying depth of invasion
|
- White circles
- White structureless areas
- Central keratin (not poorly differentiated)
- Radial, linear and looped vessels (polymorphic vessels)
|
| SCC in situ/Bowen’s disease |
- Scale (might be more than AK)
- Thickened base
- Might be hyperkeratotic
|
|
- Coiled vessels in linear arrangement
- Pigmented dots in linear arrangement
- Might be pigmented with segmental radial lines
- White circles
|
| BCC |
- Shiny pink
- Flat or nodular
- ± ulceration
- ± telangiectasias
- ‘Rolled edge’ might be visible
- Variable amount of pigment might be present in pigmented BCC
- Aggressive subtypes might be ‘whiter’ than the surrounding skin
|
- Smooth, although some exhibit scale and ulcerated BCCs might have an adherent clot
- Aggressive subtypes might be firm and indurated
|
- Serpentine/branched well defined vessels
- Ulceration
- Polarised specific perpendicular white lines
- Blue clods
- Converging radial lines
|
| Seborrhoeic keratosis |
- Well-demarcated border
- ‘Stuck-on’ appearance
- Wide variety of appearances
- Irritated lesions might mimic SCC
|
- Rough, waxy surface
- Palpable
- Can be crusty, raised and hyperkeratotic
- Might be friable
|
- Comedo-like openings
- ‘Crypts and fissures’
- Milia-like cysts
|
| Psoriasis |
- Might mimic SCC in-situ but usually several present
- Erythematous plaques with surface scale
|
|
- Scale
- Monomorphic dot vessels in a diffuse arrangement
|
AThis is not a comprehensive list.
AK, actinic keratosis; BCC, basal cell carcinoma; KC, keratinocyte cancer; SCC, squamous cell carcinoma. |
Treatment approach
In a patient with significant solar damage, AKs are usually found as field disease rather than isolated lesions, and in this context, treatment of individual visible AKs will always be suboptimal to field treatment.5 Field treatment typically results in a cosmetically superior outcome over cryotherapy to individual lesions, with patients also reporting an improvement in the complexion and uniformity of the treated skin.12
Due to the malignant potential of AKs, the need for exclusion of SCCs should be assessed. This assessment should encompass specific history and examination findings, including:
- polymorphic vessels on dermoscopy
- history of rapid growth
- tenderness
- hyperkeratosis
- thickness of the base
- induration
- surrounding erythema.
For potential KCs, the initial biopsy can be conducted using a partial biopsy technique, with punch favoured over shave biopsy for hyperkeratotic lesions, as the base of the lesion needs examination by the pathologist for accurate diagnosis.13 Diagnostic sampling error might occur with partial punch biopsies due to SCC (both in situ and invasive) potentially being focal within an AK lesion.
Definitive management of suspicious individual lesions might be arranged as first-line therapy or following initial histopathological analysis, with options including excision, curettage and diathermy, topical treatment, and cryotherapy. Cryotherapy is the gold standard treatment for individual AKs, using liquid nitrogen with an open spray technique. A treatment requires a long enough duration, so the frozen region is maintained for 10–15 seconds (two or three short spurts is usually enough to achieve this). Cryotherapy might be considered for treating SCC in situ and will require longer (30-second) freeze cycles.2,8 Caution is advised when treating SCC in situ in terminal hair-bearing areas (eyebrows and scalps, including bald scalps), as the cancer might tract deep down the epidermis that surrounds the hair follicle infundibula. Although the lesion is still in situ, the depth might mean that superficial destructive treatment (cryotherapy, curettage and diathermy, and topical treatment) is inadequate. As such, these lesions are better managed with surgical excision, particularly when of larger size, present for longer duration and in the setting of immunosuppression.
For patients requiring field treatment, several options are available (Table 4). Suitability is determined by field site, patient factors (eg work schedule, personal commitments, personal preference and expectations) and the treating doctor’s assessment and expertise. Treatments are usually performed in the cooler months. Combined with provision of adequate verbal and written information, open discussion with the patient regarding the benefits and limitations of each treatment is vital to ensure patient adherence and treatment efficacy. Cryotherapy of individual (thicker) lesions pre-field treatment might reduce the burden of disease further.5 Pretreatment use of a keratolytic containing salicylic acid (eg CeraVe SA®) for two weeks prior can improve treatment efficacy by reducing the amount of surface keratin present. Areas of field cancerisation might require a multimodal approach of a combination of lesion-directed treatments as well as one or more field treatments performed a few weeks apart.
| Table 4. Options for field treatment for AKs |
| Field treatment modality |
Brand name |
Frequency of application |
Duration of treatment |
Review periodB |
| 5-FU 5% |
Efudix® or APOC 5-FU® |
Twice daily |
2–4 weeksA |
2, 4 weeks |
| 5-FU 4% |
Tolak® |
Once daily |
2–4 weeksA |
2, 4 weeks |
| 5-FU 5% + calcipotriol 0.005% |
(Compounded) |
Twice daily |
4 days (face), 6 days
(scalp/body)A |
Day 6 (face), 8 (body) |
| Imiquimod 5% |
Aldara® |
Once daily 3 days/week |
4 weeks |
2, 4 weeks |
| PDT 5-ALA 20% |
(Compounded) |
Statim |
10–20 min |
Day 2 and 14 |
| PDT (conventional) MAL 16% |
Metvix® |
Statim |
10–20 min |
Day 2 and 14 |
| PDT (daylight) MAL 16% |
Metvix® |
Statim |
2 h |
Day 2 and 14 |
| Diclofenac 3% |
Solaraze® |
Twice daily |
8–12 weeks |
4, 8 weeks |
ACessation of treatment should be when erosive stage is achieved.
BReview can be performed in person or with photos sent prior to a telehealth consult. Patients who have performed field treatments before might proceed to complete the treatment without needing follow-up to ensure efficacy during the treatment.
5-ALA, 5-aminolevulenic acid; MAL, methyl aminolevulinate; PDT, photodynamic therapy. |
5-Fluorouracil
Topical 5-fluorouracil (5-FU) is the original field treatment option, continuing to demonstrate strong efficacy and safety profiles, with the ability to treat larger fields of up to 500 cm2 (eg whole face or hand/forearm).14 5-FU is also used to manage SCC in situ, albeit typically with a longer treatment duration (six weeks). 5-FU is a cytotoxic/chemotherapy drug selective for proliferating cells as encountered in precancerous AKs and skin cancers. The typical formulation is 5% concentration (Efudix®, aqueous cream vehicle) applied twice daily by the patient themselves as a fine smear for 2–4 weeks. A newer 4% formulation (Tolak®, arachis oil vehicle) applied once daily for two to four weeks appears to be equally effective.15 Patients are advised to avoid direct sun exposure to the treatment site.
Treatment efficacy is dependent on the patient’s ability to tolerate the treatment until the desired ‘erosive stage’, as judged by the treating clinician, which manifests as dark adherent scabs/crusting with surrounding erythema (Figure 1). If treatment is ceased early, when lesions are erythematous only rather than scabbing/crusted, efficacy is reduced. How therapy is tolerated varies between patients, with treated skin often itchy and painful towards the end of the treatment. Reaction will only occur if AKs or skin cancers are present and will typically start to appear around day 4 or 5.

Figure 1. A man, aged 72 years, with field cancerisation and several biopsy-proven SCC in situ arising within a field of surrounding AKs. (A) Pretreatment close-up: the small orange circle indicates a biopsy proven SCC in situ found using dermoscopy; the large orange circle indicates multiple AKs. (B) Treatment with 5-FU 5% twice daily at 3 weeks: the green circles indicate ‘dark scabs’, indicative of the ‘erosive stage’, which is an adequate reaction if treating AKs only. (C) Treatment at 6 weeks: a more severe crusting reaction. Longer duration is required due to in-field SCC in situ. (D) Follow-up at 6 weeks showing adequate field clearance.
AK, actinic keratosis; 5-FU, 5-fluorouracil; SCC, squamous cell carcinoma.
There is typically a compromise between treating a large enough area to be worthwhile while small enough that the patient can tolerate the side effects. For treatment-naive patients, a smaller initial treatment area is suggested to gain familiarity with the expected side effects and with the resolution phase. For patients who struggle to achieve the desired erosive stage reaction, a two-day break and/or reduction in frequency to daily instead of twice daily application might prove useful. Patients are advised that the reaction takes two weeks to resolve and use of a topical steroid (eg methylprednisolone aceponate [Advantan Fatty Ointment®]) will reduce symptom duration. Usually, the face and chest require a shorter treatment than the arms and scalp, with lower limbs requiring longer treatment durations.
An off-label combination of topical 5-FU and calcipotriol has proven efficacy with a shorter treatment duration, noting that off-label status needs to be clearly communicated during patient consent.16,17 As calcipotriol cream is not readily available in Australia, the treatment requires the services of a compounding pharmacy. Recommended duration is four days for the face and six days for body sites, and peak reaction should be two days following cessation. In the author’s experience, four days does not produce adequate reaction for many patients. A day 6 review allows assessment of efficacy and whether a longer duration is required.
Imiquimod
Imiquimod 5% (Aldara®) is an effective alternative if 5-FU is not tolerated, noting that patients require an intact immune system.16,18 Treatment is limited to 25 cm2; exceeding this field size increases the risk of systemic flu-like side effects. Like 5-FU, imiquimod will typically be lesion selective and only cause a reaction if AKs or skin cancers are present. A crusting reaction, not unlike that for 5-FU but usually more severe, indicates the end of treatment.
Imiquimod is TGA-approved for the treatment of AKs but also superficial BCCs. For AKs, patients are managed with one or two courses of imiquimod (separated by four weeks between courses). Current guidance directs self-application once daily three days per week for four weeks, although a study by Serra-Guillén et al (2018) advocates for a 12-day continuous regimen.19 For management of superficial BCC, application increases to five days per week for six weeks.
Photodynamic therapy
Photodynamic therapy (PDT) utilises a photosensitising topical medication (5-aminolevulenic acid [5-ALA] or methyl aminolevulinate [MAL; Metvix®]) applied to the field area. After incubation for two to six hours (depending on the protocol used), the field is subjected to a light source.16 The conventional light source is a light-emitting diode lamp (red light, blue light, or both) for a short duration, typically applied for 10–20 minutes depending on the source strength. Laser light of the same wavelengths can also be used. An alternative daylight PDT regime with MAL uses outdoor sun exposure for two hours with concurrent application of sunscreen.
Evidence for efficacy in the treatment of pigmented AKs is mixed.20 For example, Nguyen et al (2019) demonstrated that pretreatment with 5-FU or calcipotriol prior to PDT increased efficacy but reported an increase in adverse events.21
Because PDT is administered as a single treatment, it inherently provides a compliance advantage over patient-administered treatments.21 There is, however, no opportunity to tailor therapy based on the patient’s response.
Conventional PDT can be a painful experience, with options for pain management including use of moderate to strong analgesia, topical anaesthetic one hour prior or nerve blocks. The use of cooled air directed onto the treatment field can also improve the experience. Patients require 48–72 hours of strict avoidance of sunlight or bright light exposure post-treatment.
Sunscreen
Sunscreen is considered a field treatment for patients with significant solar damage, with the Nambour Skin Cancer Prevention Trial and subsequent studies demonstrating a reduction in the acquisition of new AKs, SCCs and melanomas with sunscreen use.22–24 Broad spectrum sunscreens (covering UVA and UVB rays) with a sun protection factor (SPF) rating of SPF30 and above are recommended.25
Sunscreen should be applied 15–20 minutes before exposure for efficacy and is generally recommended for a UV index of 3 and above. The recommended amount of sunscreen applied for an adult is one teaspoon per limb, one for the front of the body, one for the back and one for the head (ie seven teaspoons or 35 mL for the whole body). It should be reapplied every two hours and after sweating or swimming.25
Other treatment options
Other field treatment options include volumetric modulated arc therapy (VMAT), radiotherapy, diclofenac 3% and tirbanibulin. Ingenol mebutate (Picato®) is no longer recommended, as it was found to increase the incidence of skin cancers.26
VMAT radiotherapy is available after referral to radiation oncology centres that offer it. Use is restricted to severe field cancerisation that has been refractory to conventional field treatment measures.27 Although highly effective, potential issues with management arise when recurrent disease occurs in the treated field.28
Diclofenac 3% (Solaraze®) is applied topically twice daily over three months. Although side effects are usually mild, treatment efficacy is generally less than for other field treatments, and the longer duration of treatment limits adherence.16
Tirbanibulin is a new treatment approved in Europe and the USA but not yet available in Australia. It is approved for application to a 25-cm2 field area once daily for five days.16
Nicotinamide and acitretin are chemoprophylactic oral agents also available for patients with field disease, with studies of both drugs reporting reduction in AKs and KCs.16
See Figure 2 for a decision-making flow diagram.
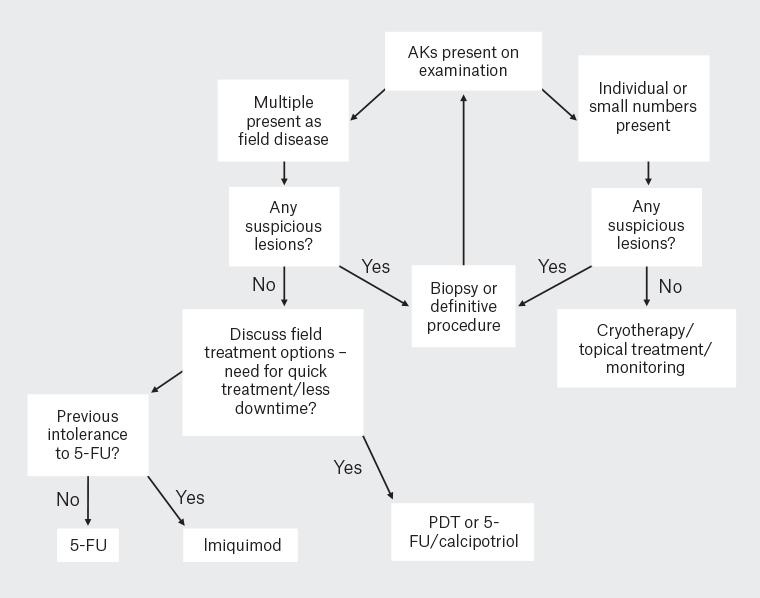
Figure 2. AK treatment decision making. Note this is a simplified management diagram and other patient factors and physician factors such as experience and modality availability will play a role. PDT and 5-FU/calcipotriol are still options for those patients that do not require a quick treatment. Start back to the top of the diagram following field treatment review at 6–8 weeks and for future skin examinations.
AK, actinic keratosis; 5-FU, 5-fluorouracil; PDT, photodynamic therapy.
Review following field treatment
Clinical review typically occurs 6–8 weeks following cessation of field treatment, allowing time for the inflammation associated with treatment to subside. The review should also explore the patient’s experience, address concerns and revisit pretreatment expectations. Any residual lesion present at six weeks usually persists. These should be assessed clinically and with a dermatoscope, with biopsy or definitive treatment often indicated to exclude malignancy.
Regular skin examinations should be scheduled depending on individual patient risk. The author reviews patients with significant skin damage with a history of AKs at least yearly, and patients with a history of skin cancers at least six monthly. Regular review allows for timely detection of new primary skin cancers and AKs in previously treated areas and consideration of the need for further lesion-specific or field treatment. How effective the prior field treatment was and the patient’s subsequent UV protection strategies will determine the interval between field treatments.
Conclusion
Significant solar damage is typified by the presence of AKs, typically manifesting as field disease. There are several different treatment options available for management of these patients, including topical therapy, PDT and oral treatments. The specific regime will differ between individual patients, the area being treated and local expertise. Field treatments should be combined with sunscreen use and regular follow-up appointments.
Key points
- A focused history is required to assess overall risk. SCAN is a useful approach to elicit a lesion specific history of a lesion(s) concerning the patient.
- Some hyperkeratotic lesions require a lesion-specific management approach prior to field treatment, depending on clinical appearance and biopsy results.
- If field disease is present, a field treatment is required to adequately manage the disease burden and reduce the future risk in the treated area. Field cancerisation might require a multimodal approach.
- Several field treatment modalities exist. Tailoring the available options to the patient and the treatment sites requires careful assessment and discussion to ensure adherence and efficacy.
- If a lesion persists 6–8 weeks following field therapy, it should be treated as suspicious. Ongoing regular follow-up of patients (6–12 monthly) is required to assess for new primary skin cancers, the adequacy of prior field treatment and the need for future treatments.