Case
A man, aged 27 years, presented to a regional hospital after being thrown off a dirt bike at a speed of 30 km/h, landing on his left side. The patient was wearing full protective equipment. The patient was right-hand dominant and worked on a gas rig. He smoked five cigarettes per day.
On examination, there was an obvious step deformity to his left shoulder without an open wound (Figure 1). He exhibited a painful range of motion (ROM) with limited abduction to 70°.

Figure 1. Patient inspection on presentation.
Note the step deformity and bruising anterior to the left acromioclavicular joint.
Question 1
What is the provisional diagnosis?
Question 2
What is the initial management?
Answer 1
The provisional diagnosis is an acromioclavicular joint (ACJ) dislocation. The ACJ is formed by the lateral clavicle articulating with the acromion process (Figure 2). The joint is stabilised by the acromioclavicular (AC) and coracoclavicular (CC) ligaments tethering the lateral clavicle to the scapula.
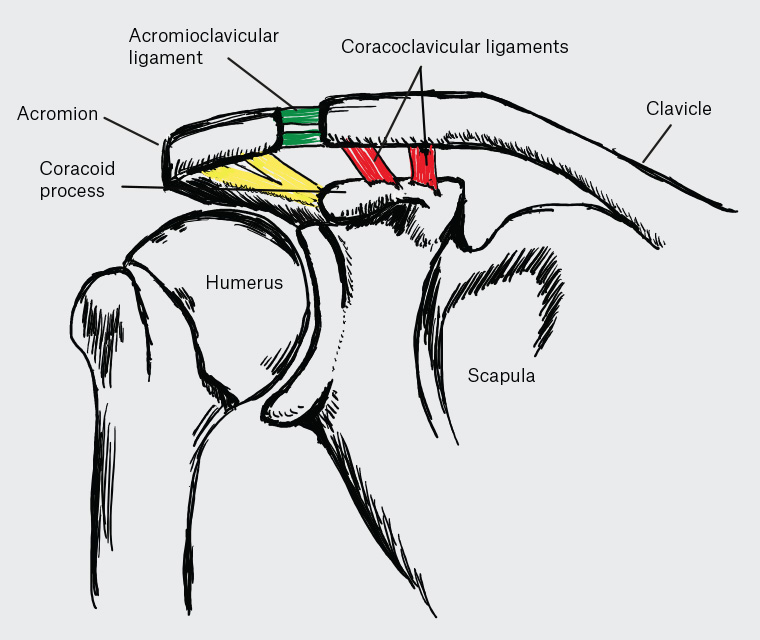
Figure 2. Anatomy of the coracoclavicular joint.
ACJ injuries are common in young adults, predominately men. ACJ dislocations result from a direct lateral blow to the acromion or ‘point’ of the shoulder; typically caused by falls from bicycles, contact sports or motor accidents. ACJ dislocations account for up to 50% of shoulder injuries in contact sports.1
ACJ dislocations are classified into six types using the Rockwood classification system (see figure 5.10 in ‘Acromioclavicular joint’ in the Radiology Key search engine).2 Injuries are classified based on X-ray findings, focusing on the relationship between the lateral clavicle, the acromion process and the coracoid process. Type 1 and 2 injuries represent intact CC ligaments with sequential widening of the ACJ. Type 3–6 injuries suggest rupture of the AC and CC ligaments differentiated by the distance and direction of distraction.3
Answer 2
It is important to exclude fracture in the setting of trauma. Plain film X-rays are the primary method of investigation. Appropriate views include the anteroposterior (AP), axillary and Zanca views. A Zanca view directs the X-ray beam 15° cephalad. AP views of the injured and contralateral shoulders can be used to characterise the displacement and direction of the injured clavicle.4 Physical examination should be undertaken to exclude neurovascular injury.
Acute dislocations are managed with sling immobilisation. It is important to encourage active ROM of the wrist and elbow during this period. Acute pain and swelling are managed with simple analgesia and icepacks. Type 1 injuries recover quickly. Type 2 injuries should be referred to a physiotherapy service for rehabilitation. Type 3–6 injuries should be referred to an orthopaedic service for consideration of surgical intervention.
Case continued
The patient was given a broad arm sling to rest. AP views of bilateral shoulders and axillary X-ray views were obtained (Figure 3).

Figure 3. X-ray images of acromioclavicular dislocation: (a) anteroposterior view bilateral shoulders and (b) axial view.
Question 3
What are the relevant radiographic findings?
Question 4
What is the indication for surgical intervention?
Answer 3
Figure 3A shows significant widening of the left CC interval compared with the uninjured right side. Figure 3B shows posterior translation of the lateral clavicle in relation to the acromion process. This represents a Rockwood Type 4 injury.
Answer 4
Type 1 and 2 ACJ injures can be managed non-operatively and do not require referral to an orthopaedic service. High-energy injuries that result in instability of the ACJ typically require surgical intervention. This incorporates all Rockwood Type 4, 5 and 6 injuries. Type 3 injuries represent a grey area, and treatment should be tailored to the individual patient.5 Patients with Type 3 ACJ injuries should be referred to an orthopaedic surgeon to discuss treatment options.
There are many surgical techniques to fix ACJ dislocations. Common techniques include temporary hook plate fixation and ligament reconstruction techniques. The aim is to restore the CC distance in order to allow ligament healing.6
Case continued
The patient underwent a left ACJ reconstruction (Figure 4). The reduction was held using a synthetic ligament device looped around the coracoid process and anchored to the lateral clavicle. Referral was made to the physiotherapy service for graduated ROM exercises. Smoking cessation advice was provided to improve surgical wound healing.

Figure 4. Zanca view X-ray film after acromioclavicular joint reconstruction.
Note the reduction in the coracoclavicular interval, compared with Figure 3A.
Question 5
What is the prognosis for ACJ dislocations?
Answer 5
ACJ dislocations show good return to function when appropriately managed. The average return to work is 13 weeks, although this period is longer in manual workers.7 Recent prospective trials have emphasised the importance of physiotherapy in the management of ACJ dislocations, with outcomes equal to surgical management in some cases.8
Case continued
At the three-month postoperative review, the patient had achieved equal ROM between the right and left sides. There was a minimal difference in muscle bulk between shoulders. The patient was advised against high-risk activities, including contact sports and dirt biking, for a further three months.
Key points
- The management of ACJ injuries depends on the structures injured.
- Type 1 and 2 injuries can by managed non-operatively with early ROM and physiotherapy considered for strength training.
- Type 3–6 injuries should be referred to an orthopaedic service for consideration of surgical intervention.