Background
Australia and New Zealand have the greatest burden of skin cancer in the world. General Practitioners (GPs) are the first interaction for most patients with skin cancer concerns and are well placed to provide information regarding primary and secondary skin cancer prevention.
Discussion
GPs can help reduce the incidence of skin cancer by identifying high-risk individuals in primary care clinics, enrolling them in a surveillance program and tailoring skin cancer prevention advice. GPs should encourage patients to practise sun safety through the use of shade, photo-protective clothing, sunglasses and sunscreen and being aware of the ultraviolet index through tools such as the SunSmart App to guide behaviours and activities.
Australia and New Zealand experience the highest incidence of skin cancer in the world.1 The most common skin cancer subtypes are basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma. Skin cancer is the most common type of cancer managed by general practitioners (GPs) in Australia, and consultations related to skin cancer account for 3% of all issues managed in primary care.2 Skin cancer is highly amenable to primary prevention and early detection, and GPs are well placed to diagnose and treat skin cancers, as well as advocate prevention strategies. This article discusses primary and secondary prevention of skin cancer in Australia.
Primary prevention
It has been estimated that 95% of skin cancers are caused by exposing the skin to ultraviolet (UV) radiation.3 The high incidence of skin cancer in Australia and New Zealand is due to the very high ambient UV radiation, combined with a population where a large proportion of people have Anglo-Celtic ancestry and minimal protection from melanin in the skin. Unfortunately, in Australia, this is coupled with the desire for a ‘healthy tan’, which has been part of the Australian culture since the mid-1900s.4
Primary prevention of skin cancer involves reducing exposure to UV radiation by modifying time outdoors and using sun protection. Australia has led the world in the development of sun protection and public awareness campaigns, starting with the implementation of the ‘Slip, Slop, Slap’ campaign, which was released by the Cancer Council in 1981. In 2007, the slogan was updated to ‘Slip, Slop, Slap, Seek, Slide’.5 The National SunSmart Schools Program was launched in 1998, with the goal being for each school involved to implement an approved sun protection policy, addressing 10 key areas of sun protection across three areas: environment, behaviour and information.6 The ‘Dark Side of Tanning’ campaign was implemented in 2007–08, aiming to increase awareness of the increased risks of melanoma associated with obtaining a tan.4 After a decade of campaigning, led by the Cancer Council and featuring Clare Oliver’s message ‘No tan is worth dying for’, commercial solariums were banned in 2015.7
Studies show that these public awareness campaigns have been effective in changing knowledge, attitudes and behaviours with respect to sun exposure. National surveys during summers between 2003–04 and 2016–17 suggest that there has been a reduction in Australian’s pro-tanning attitudes, as well as increased sunscreen use and reduced sunburns.3 However, there is still inadequate uptake of sun protection strategies and too many people are still being sunburnt; GPs can play an important role in increasing sun protection awareness through education and counselling.
The UV index is a way of describing the daily danger of solar UV radiation intensity. Current sun protection advice is that sunscreen should be applied as part of the usual daily routine on all days when the UV index is forecast to reach 3 or more, at any part of the day, based on evidence that daily sunscreen application reduces the risk of SCC, melanoma and keratoses.8–10 It provides a baseline level of protection during incidental sun exposure. In addition, if planning on being outdoors at times of the day when the UV index is 3 or more, all five sun protection measures should be used (ie slip on a shirt, slop on sunscreen, slap on a hat, seek shade and slide on sunglasses). Clothing should be used to cover as much skin as possible, as, in general, it provides greater protection than sunscreen. Apps such as the SunSmart App (Figure 1) can be used to guide behaviours and activities. GPs should aim to educate their patients about the UV index and its implications for sun protection (Table 1).
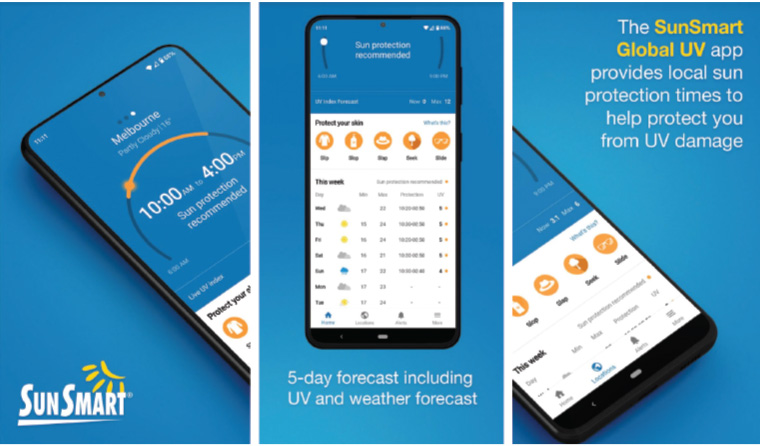
Figure 1. The SunSmart App.
Reproduced with permission from SunSmart Victoria.
Given that it has been estimated that 50% of the total dose of UV radiation received up to age 60 years occurs before age 20 years,11 it is also vital that GPs advocate for extra care with childhood sun exposure. It is well documented that excessive sun exposure in childhood (especially burns) increases the risk of basal cell carcinoma and melanoma.12–14 SCC, in contrast, has a more linear relationship with total lifetime exposure to UV radiation and with immunosuppression, including declining immune function in the elderly.15 Given that babies aged under six months have highly absorptive skin, it is not recommended that they wear chemical sunscreens and instead should rely on physical barriers and shade (Table 1).15
| Table 1. How to answer common patient questions about skin cancer and sun safety in general practice |
| ‘While I am here, can you look at this spot on my skin?’ |
This is not an uncommon request at the end of a consultation. Take adequate time to take a history and examination. If the patient would benefit from a full skin check, consider asking them to rebook for this. If you do not feel comfortable providing a firm diagnosis of a skin lesion or you are not trained in use of the dermoscopy, advise them of this and refer them appropriately. |
| ‘What sunscreen do you recommend using?’ |
At least SPF 30+. Ensure the sunscreen that they are using is approved for sale or supply in Australia and is listed in the ARTG. These products can be identified by an AUST L number on the label.16 Lotions and creams should be used. Sprays are not recommended, as they deliver minimal sunscreen to the skin.17 Relying on sun protection from makeup is not recommended (eg foundation, BB creams), as it is unlikely that the patient will wear enough product to confer protection.
The most important factors for sunscreen efficacy are adherence and application, so ensure that the patient is applying enough product and reapplying every 2 h when outdoors.
Check that the patient is engaging in other sun safety measures, as sunscreen is only one component. Patients should understand that sunscreen only reduces exposure to UV radiation, and it is still possible to accumulate UV radiation-induced damage and to sunburn even while wearing sunscreen. |
| ‘I don’t like using sunscreen.’ |
There are many reasons that patients do not like to use sunscreen. Exploring these reasons can help elucidate barriers to use. Sunscreens with a higher SPF might feel thick or sticky, which can be a barrier to use.18 Some patients might also experience sensitivity to the ingredients found in sunscreen, such as irritant or allergic contact dermatitis or, more rarely, photo contact dermatitis.19 There are many different sunscreen products on the Australian market, so patients are likely to be able to find a sunscreen that they can tolerate. If patients are still reluctant to use sunscreen, they should be reminded that sunscreen is only one aspect of photoprotection, and they should still engage in other sun protective measures: use of shade and photoprotective clothing (eg hats, sun sleeves or sun wraps, and sunglasses). |
| ‘Why do I need to be mindful of skin cancers beneath my underwear? I never sunbaked naked!’ |
Not all skin cancers are caused by UV radiation. In addition, clothing does not block all UV radiation, with some clothing manufacturers providing UVPF. The more protective clothing tends to have a tighter weave and darker colours. Naturally, we tend to favour thinner clothes with less skin coverage when it is hot. A crude test for patients is to hold clothing up and see if visible light passes through it as an indicator of the degree of protection from UV radiation. |
| ‘I heard about this app that helps detect skin cancers. Why can’t I just use that?’ |
There are several smartphone skin cancer or mole-checking apps now available to monitor and photograph moles. Some of these apps will also provide some form of automated diagnosis. At present, research has shown that these apps have poor and variable performance in the role of skin cancer diagnosis, so should not be relied on to detect skin cancers.20 Current guidelines do not recommend the use of smartphone apps for patients to self-diagnose skin cancer. |
| ARTG, Australian Register of Therapeutic Goods; BB, blemish balm; h, hour; SPF, skin protection factor; UV, ultraviolet; UVPF, ultraviolet protection factor. |
Secondary prevention
Secondary prevention focuses on identifying skin cancer early by encouraging individuals to present to a doctor with lesions of concern and by enrolling high-risk individuals in a surveillance program. Unlike several other cancers (eg breast, bowel and cervical), there is no population-based screening program for either melanoma or non-melanoma skin cancer in Australia.
In regard to melanoma, the Royal Australian College of General Practitioners (RACGP) recommends that individuals at high risk for melanocytic skin cancer receive 6–12 monthly skin examinations by a trained clinician.21 As an example, see the information in Table 2 regarding suggested screening for melanoma.21 The ‘Scan Your Skin’ risk prediction tool by the Skin Cancer College Australasia can help identify patients at high risk for melanoma.22 Although tools and guidelines can be helpful to guide clinicians, it is important for GPs to note that there is no current consensus that these tools or guidelines should be implemented nor, if implemented, at what age surveillance should start and what the surveillance interval should be. Genetic counselling and frequent screening are recommended for individuals affected by naevoid basal cell carcinoma syndrome or who have a mutation in the CDKN2A gene.
| Table 2. Melanocytic skin cancer: Identifying risk16 |
| Who is at risk? |
What should be done? |
How often? |
References |
Average risk:
- Medium/dark skin colour and no risk factors
|
Primary preventive advice (III, B) |
Opportunistically |
60 |
Increased risk:
- Family history of melanoma in first-degree relative (RR=1.7)
- Fair complexion, a tendency to burn rather than tan, the presence of freckles, high naevus count (>100), light eye colour, light or red hair colour
- Presence of actinic damage (RR=2)
- Past history of NMSC (<40 years of age higher risk)
- People with childhood high levels of UV exposure and episodes of sunburn in childhood (RR=2)
|
Primary preventive advice and examination of skin (III, B) |
Opportunistically |
60, 65 |
High risk (risk >6 times normal):
- Previous history of melanoma (RR>10)
- >5 atypical (dysplastic) naevi (RR=6)
|
Preventive advice, examination of skin (with or without photography) and advice on self-examination (III, C) |
Every 6–12 months (Practice Point)
Frequency of follow-up examinations for people who have had melanoma is based on disease stage |
66
64 |
| NMSC, non-melanocytic skin cancer; RR, relative risk; UV, ultraviolet. |
GPs can educate patients on how to examine their own skin between formal skin checks by a doctor. High-risk patients should be advised to perform self-examinations every three to four months, and average to low-risk patients should be encouraged to examine their skin annually and be reviewed by a doctor if they note a lesion of concern.23 For people at high risk of melanoma, particularly those with multiple dysplastic naevi, total body photography can assist in monitoring lesions and identifying change.24
Chemoprevention in high-risk patients
Chemoprevention for keratinocyte cancer can involve regular sunscreen use and chemoprophylaxis. These methods can also reduce and prevent actinic keratosis, which might progress into an SCC if left untreated. In addition to regular sunscreen use, chemoprophylaxis with vitamin B3 (also known as nicotinamide or niacinamide) or acitretin can be considered for individuals with a heavy burden of keratinocyte skin cancers. Vitamin B3 is sold in shops and pharmacies and is currently recommended at an oral dose of 500 mg twice daily as a chemo-preventative adjunct in high-risk, immune-competent patients with a history of multiple keratinocyte cancers. In the Oral Nicotinamide to Reduce Actinic Cancer (ONTRAC) trial, oral vitamin B3 was shown to have possible efficacy in participants with at least two keratinocyte skin cancers in the previous five years.25 At this point, it is not recommended for lower-risk individuals without a history of keratinocyte cancer.26 One study has been conducted in a small cohort of transplant patients and shows no benefit in this group.27
Acitretin is an oral retinoid with proven efficacy in the reduction of SCC, including human papillomavirus-induced neoplasia and actinic keratoses in both immunocompetent and solid organ transplant patients.26 Numerous contraindications and side effects require careful patient selection and monitoring, as treatment needs to be continued to maintain efficacy. The main concerns are mucocutaneous dryness, hair shedding, hypertriglyceridaemia and teratogenicity. Long-term use can result in calcification of tendons and ligaments and diffuse idiopathic skeletal hyperostosis (DISH), with rare cases of hepatoxicity.
In Australia, acitretin requires referral to a dermatologist for prescription. There are no clear criteria for when acitretin should be started and this is decided on a case-by-case basis. Higher doses will result in greater clearance of actinic damage and lowered incidence of SCC but will be limited by side effects. Doses of 10–20 mg daily are usually tolerated with resultant benefit.28
Conclusion
Australia and New Zealand have the greatest burden of skin cancer in the world. GPs are the first interaction for most patients with skin cancer concerns and are well placed to provide information regarding primary and secondary prevention. Identifying high-risk individuals in primary care clinics, enrolling them in a surveillance program and tailoring skin cancer prevention advice might be more beneficial than generic advice. GPs should encourage patients to practice sun safety by using shade, photo-protective clothing, sunglasses and sunscreen and being aware of the UV index through tools such as the SunSmart App (Figure 1) to guide behaviours and activities.
Key points
- Australia and New Zealand have the greatest burden of skin cancer in the world.
- Primary prevention for skin cancer in Australia and New Zealand includes both public health campaigns and tailored interventions to individuals through primary care.
- GPs are uniquely placed to identify high-risk patients in the Australian and New Zealand population and to facilitate screening interventions.
- High-risk patients with a history of keratinocyte cancer should be considered for chemoprophylaxis.
- GPs should encourage patients to practice sun safety through use of shade, photo-protective clothing, sunglasses and sunscreen and being aware of the UV index.