Climate change is one of the biggest threats facing the healthcare sector. Multiple studies have linked an excess of greenhouse gases (GHGs) to the steadily increasing mean temperature across the globe, which is threatening the environment.1,2 Globally, carbon dioxide (CO2) is the most abundant of the GHGs. It makes up an average 74% of total GHG emissions.3 It is mainly generated by the burning of fossil fuels and industry production.3 Other GHGs include methane (17% worldwide), nitrous oxide (6%) and trace gases (2%).3 In New Zealand, the GHG emissions are predominantly CO2 (46%), methane (42%) and nitrous oxide (10%).4
Given the small population size, the total GHG emissions produced by New Zealand are low. In 2018, the gross GHG emissions were 70.7 million tonnes CO2 equivalent (CO2e), and in 2019, 82.3 million tonnes CO2e.3,4 This amount is minuscule compared to the largest emitter, China, which produced 1.7 billion tonnes of CO2e in 2018.3 The per capita emissions in New Zealand are also low compared to other high-income countries, at 4.55 t per person in 2018, compared to 15.6 t for Australia, 14.5 t for the USA and 16.4 t for Canada.3 Low-income countries, such as India, consistently produce far lower per-person rates. Despite being third overall for total GHG emissions in 2018, India produced an average of 1.8 t of CO2e per person.3
Transportation is one of the largest contributors to GHG emissions. Worldwide transportation accounts for 21% of all CO2 emissions, with road vehicles comprising 75% of the CO2 emissions.5 In New Zealand, transportation is responsible for 43% of all CO2 emissions, of which road vehicle emissions make up 91%.4
The healthcare sector contributes significantly to GHG emissions, making up an estimated 4–5% of total GHG emissions globally and 3–8% of total GHG emissions in New Zealand.6,7 Climate change has been linked to numerous poor health outcomes. These occur because of direct environmental injuries (eg due to droughts, heatwaves and bushfires); changes in access to water and food; and changes to food, water and vector-borne diseases.8 This can create great inequality. The lowest-income countries, despite contributing the least to GHG emissions, will be the most likely to experience adverse health outcomes secondary to climate change.
Telemedicine is the process of using technology to enable healthcare delivery remotely. It has been increasing in popularity, particularly since the COVID-19 pandemic has limited in-person assessment.9 The potential role of telemedicine in reducing CO2 emissions through reduced transportation is a developing area of interest.10,11 A systematic review of 31 studies assessing the CO2 saving from telemedicine across all disciplines reported carbon savings ranging between 0.69 and 893 kg CO2e per consultation.12 Holmner et al and Masino et al reviewed real-time telemedicine consultations and concluded that they significantly reduced CO2 emissions.13,14 Holmner et al completed a life cycle assessment of CO2 based on 238 virtual consultations in Sweden.13 They found that the total CO2 emissions from the telemedicine consults were 602 kg CO2e or 1.4–2.8% of the CO2 from estimated in-person reviews.13 Masino et al reviewed 840 consultations in Canada, which resulted in an estimated 757,234 km saved or 185,159 kg CO2e.14 Both studies report the use of videoconferencing equipment to be the main contributor to CO2 emissions for telemedicine consultations. A study from the USA looked at virtual consultations for the management of isotretinoin.15 They report a saving of 5137 kg CO2e through the reduction in travel during the eight-month study period.15 A limitation of these studies is the minimal reporting of store-and-forward methods of telemedicine and the assumption that all in-person travel is by private vehicle.
Given the significance of timely diagnosis and intervention of skin lesions to improve patient outcomes, telemedicine has been increasingly used to enable prompt assessment, particularly for those living in rural areas.16,17 The use of telemedicine has increased significantly since 2020 due to the restrictions enforced by the COVID-19 pandemic.9
Our department has been using an established teledermatology referral pathway since 2017. A skin lesion advice service was developed in 2017, after introducing electronic referrals, allowing images to be sent in by general practitioners (GPs). This Suspected Skin Cancer (SSC) pathway is an advice service specifically designed for skin lesions. It accounts for half of all referrals to the Dermatology Department at Te Whatu Ora Waikato, with the rest using the ‘general’ assessment template. The SSC template requires specific information about the patient and the lesion. The referrer must send regional, close-up and dermoscopy images of the lesion to receive diagnostic and management advice. Previous studies have shown this to be an effective and favourable assessment pathway.18,19
This study aimed to assess the estimated carbon footprint of skin lesion assessment by teledermatology from primary care electronic referrals in the SSC pathway compared to the estimated equivalent for in-person review.
Methods
This retrospective study estimates the carbon footprint of virtual consultations for skin lesions assessed by an established store-and-forward method of teledermatology. The Health and Disabilities Committee of New Zealand determined the study to be out of scope for formal ethics approval because it is an audit or related activity. Locality approval was obtained from Te Whatu Ora Waikato. We evaluated electronic referrals sent to the Waikato Dermatology Department by GPs with close-up and dermoscopy images. The carbon footprint was estimated for consultations from 1 July to 31 December 2020, accounting for the use of computers, monitors, lighting and heating based on New Zealand Ministry for the Environment data (emissions of 0.98 kg CO2e per employee per day based on an eight-hour workday).20 This carbon footprint was compared to the equivalent had in-person reviews taken place, based on the average transportation modalities in New Zealand (86% private vehicle [car], 4% public transport [bus] and 10% other [non-vehicle forms of travel including walking and cycling]) based on national survey data) and vehicle emissions (0.27 kg CO2e per km for the average private vehicle and 0.16 kg CO2e per km for the average bus).20,21 Travel distance was based on a round trip from the patient’s listed address to the hospital using Google Maps.
The calculation of GHG emissions is outlined in Figure 1. The GHG for virtual consultations through the store-and-forward referral method were calculated using the following equation, where 1/48 is based on a 10-minute average per consultation (or 1/48 of the eight-hour workday estimate): Number of referrals × (1⁄48 × 0.98 kg CO2e).20 This figure was doubled to account for equivalent referrer use, given the time-consuming referral method that requires additional information and multiple images, including a dermoscopy image. The estimated emissions for equivalent in-person reviews were calculated using the sum of three equations: (Number of referrals × (1⁄48 × 0.98 kg CO2e), (Number of referrals × 86%) (0.27 kg CO2e × Median km) and (Number of referrals × 4%) (0.16 kg CO2e × Median km). The first equation relates to the equivalent use of computers, monitors, lighting and heating as for the virtual consultations (but not doubled as the referral is likely to require less time). The second equation calculates the average private vehicle emissions for 86% of referrals.20,21 The third equation calculates the average bus emissions for 4% of referrals estimated to travel by public transport.20,21
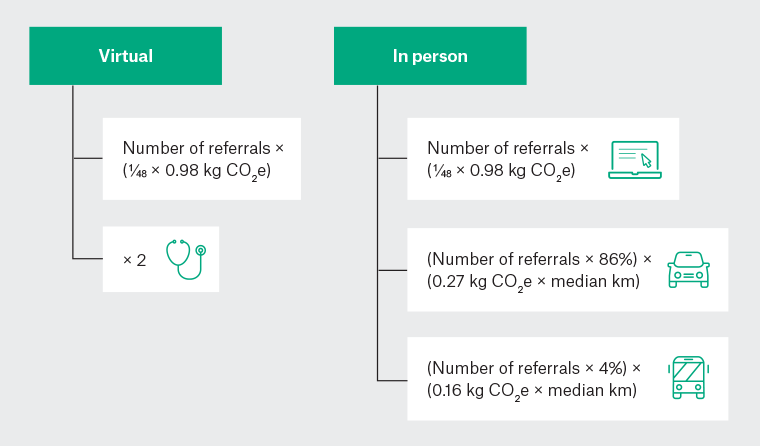
Figure 1. Carbon footprint calculations for virtual and estimated in-person assessment.
Calculations are based on the New Zealand Ministry for the Environment measuring emissions 2022 guideline.
CO2e, CO2 equivalent.
Results
A total of 484 consultations were evaluated (Table 1); 262 patients (60%) were from an urban location, 172 (36%) were from semi-rural areas, and 20 (4%) were from rural areas, based on Statistics New Zealand Urban Accessibility Classification.22 Twenty-four (5%) of the referrals had images that were inadequate for diagnosis. The total estimated in-person emissions were 5425.83 kg CO2e, compared to 19.75 kg CO2e (0.4% of in-person) for virtual consultations. The use of virtual consultations led to a reduction of 11.17 kg CO2e per consultation. Extrapolating this figure to account for all virtual skin lesion referrals for 2020 (2614 consultations) resulted in a savings of 29,277 kg CO2e for 2020. This is the equivalent of powering 3.7 houses or 6.3 petrol cars for one year.23
| Table 1. Patient demographics |
| |
Virtual consultations
n (%), N=484 |
| Age (years) |
| Overall mean (SD) |
55 (21) |
| 0–9 |
10 (2) |
| 10–19 |
24 (5) |
| 20–29 |
34 (7) |
| 30–39 |
44 (9) |
| 40–49 |
58 (12) |
| 50–59 |
73 (15) |
| 60–69 |
101 (21) |
| 70–79 |
86 (18) |
| 80–89 |
43 (9) |
| 90+ |
11 (2) |
| Sex |
| Female |
310 (64) |
| Male |
174 (36) |
| Ethnicity |
| New Zealand European |
406 (84) |
| Maori |
34 (7) |
| Pasifika |
3 (1) |
| European, other |
26 (5) |
| Asian |
11 (2) |
| Other |
4 (1) |
| Patient location |
| Urban |
292 (60) |
| Semi-rural |
172 (36) |
| Rural |
20 (4) |
| SD, standard deviation. |
Discussion
The carbon emission reduction found in this study is comparable to those of similar studies. The 11.17 kg CO2e per consultation saving falls within the lower end of the range reported by Purohit et al in a systematic review of telemedicine carbon emissions savings across all healthcare specialities (0.69–893.00 kg CO2e per consultation).12 The heterogeneity of these results is influenced by several factors: the geography of the country, which directly affects the average distance travelled for appointments; the method of telemedicine consultation (video appointments, which require more energy compared to store-and-forward consultations); and potentially the healthcare speciality, as more specialised areas might have limited accessibility, requiring increased travel. Most of the studies included by Purohit et al utilised video consultations. The one study using store-and-forward consultations for 9034 patients found an average saving of 21 km and 3.25 kg CO2e per consultation.24 This was comparable to our results when adjusted for the average distance saved (48 km and 11.17 kg CO2e, respectively). Another study of 1476 real-time teledermatology appointments reported savings of 38 miles (61 km) per consultation.25 Masino et al report on carbon emission savings for a telemedicine service in Canada. Despite using real-time consultations, they show significantly higher per consultation savings compared to our results (220 kg CO2e compared to 11.17 kg CO2e), likely related to transportation distance, with an average saving of 901 km per consultation.14 Interestingly, they estimated the telemedicine equipment to have low emissions at 0.04 kg CO2e per consultation, compared to an estimated range of 1.85–8.43 kg CO2e by Holmner et al.13,14 This difference likely relates to the longer appointment times and allowances for dedicated videoconferencing equipment in addition to desktop-based video consultations in the latter.
The main strength of our study is the adjustment of in-person calculations based on real-life transportation modality. Most studies assessing the carbon emissions of consultations (eg Lee et al, Vidal et al and Holmner et al) assume all patients would have travelled by private vehicle, falsely increasing the carbon emission estimates.13,15,24 The choice of transportation modality is significantly influenced by the patient’s location and availability of public transportation. There were several assumptions made during the virtual consult calculations. The estimated times for dermatologists and GPs to complete the SSC referrals were based on limited survey data self-estimates. It is assumed that dermatologists work separately using separate lighting and heating when, in reality, sometimes shared office spaces are used. This study is limited by using a single carbon estimate rather than allowing for multiple scenarios with sensitivity analyses, and the carbon footprint associated with image storage needed to be accounted for in the estimates. The carbon emission calculations were based on the most common cars and buses during the period, and the results might need to be updated as engine efficiency improves and electric vehicles are increasingly used. A further limitation was the theoretical nature of in-person reviews. Like most countries, public dermatology appointments in New Zealand are extremely limited and in-person skin checks are rarely offered in Waikato. Despite this, there might be some cases where a subsequent in-person assessment was still required, as seen in other studies.26 We used postcode data for distance estimates rather than residential address, reducing the accuracy of distance assessment.
There is ongoing planning and research into ways to minimise GHG emissions in the healthcare sector. This study highlights the role of virtual consultations in contributing to lower GHG emissions. Perhaps the results of this and similar studies will enable the development of algorithms to estimate the carbon footprint reduction expected for a given service to move to virtual consultations based on the geography of the area serviced and the type of telemedicine system proposed.
In addition to telemedicine for skin lesion assessment, several other strategies can be used in general practice to reduce carbon emissions. These include offering virtual appointments to patients, undertaking audits to reduce waste from procedures and encouraging patients and staff to use active and public transportation.27–29
Conclusion
Efforts to minimise GHG emissions in the healthcare sector are ongoing. Our study highlights the role store-and-forward telemedicine assessment of skin lesions can play in contributing to this reduction. In addition to the previously reported benefits of telemedicine to enable the timely diagnosis of skin lesions, we show the potential environmental benefits of this service. This is particularly true where patients have a long way to travel for specialist consultations.