Case
A man, aged 52 years, presented with a two- to three-week history of pruritic papular eruption involving the right leg. His medical history included type 2 diabetes, managed with metformin and dapagliflozin; hypertension, for which he had been prescribed olmesartan/hydrochlorothiazide; and depression, which was treated with mirtazapine. He had no known allergies and no personal and family history of skin disorders. He reported working as a mechanic with no exposure to unusual irritants. He was a smoker (10 pack-years) and social alcohol consumer (two to three standard drinks per day on weekends). On examination he was systemically well with afebrile and skin phototype 2 (White). He had discrete brownish-red and pink papules on the anteromedial aspect of the right leg (Figure 1), with no involvement elsewhere. Central erosions encircled by scales were evident on some of the papules. There was no evidence of infection locally or systemically. There was no history of diabetic neuropathy, and the patient reported no pre-existing pruritus and no rubbing or scratching to the area prior to eruption. His blood test results were unremarkable and non-contributory.

Figure 1. Pruritic papules on the right leg.
Question 1
What conditions would you include in your differential diagnosis, and what is the most likely diagnosis in this case?
Answer 1
The differential diagnoses for pruritic papular eruption involving the legs include pretibial pruritic papular dermatitis (PPPD), lichen amyloidosis, prurigo nodularis, hypertrophic lichen planus, lichen simplex chronicus and pretibial myxoedema.
1,2 Necrobiosis lipoidica can also be considered in the context of diabetes. The clinical and histopathological features of these dermatoses are outlined in Table 1.
| Table 1. Differential diagnoses of papular leg and their characteristics |
| Condition |
Characteristics |
Demography |
Typical histopathology |
| Pretibial pruritic papular dermatitis |
- Discrete brown–pink or red (flesh colour) round papules, involving the pretibial zone of leg
- Pruritus +++ (intense)
|
Middle age |
- Minimal compact orthokeratosis; superficial and mid-dermal lymphocytic infiltrate; superficial dermal fibrosis with stellate and multinucleated fibroblasts
|
| Lichen amyloidosis |
- Discrete red to dark brown keratotic papules, appearing on the anterior legs and infrequently on the extensor surface of upper limbs and back
- Pruritus +++ (intense)
|
Middle age, predominantly in skin phototypes III–V |
- Focal deposition of amyloid within the dermis with hyperkeratosis, acanthosis, papillomatosis or hypergranulosis of the epidermis
|
| Prurigo nodularis |
- Discrete and scattered brownish-red papules and nodules with a hyperpigmented border and scarring, occurring anywhere on the body within reach (eg limbs, torso)
- Pruritus +++ (intense)
|
Any age |
- Hyperkeratotic, acanthotic and parakeratotic epidermis with a dermal infiltrate of neutrophils, eosinophils, histiocytes and monocytes
- Notably thickened nerve fibres
|
| Lichen simplex chronicus |
- Various patterns of scaly, lichenified and pigmented papules to plaques anywhere on the body
- Pruritus +++ (intense)
- Can be associated with underlying skin conditions
|
Any age |
- Spongiosis, hyperkeratosis with focal parakeratosis, acanthosis, prominent granular cell layer, elongated rete ridges
- Papillary fibrosis with vertical streaking of collagen bundles
|
| Hypertrophic lichen planus |
- Various sized violaceous–brown papules to nodules, anywhere on the body but usually involving the lower limbs
- Pruritus ++ with/without pain
|
Mostly adult |
- Hyperkeratosis (without parakeratosis, acanthosis, papillomatosis) and saw-tooth rete ridges
- Band-like infiltration of the lymphocytes beneath the epidermis
|
| Pretibial myxoedema |
- From early non-pitting oedema evolving to plaques, nodules involving the pretibial area
- Usually bilateral and not pruritic
- Associated with thyroid disease
|
Usually adults; more common in women |
- Mucin (glycosaminoglycans) deposition throughout the dermis and subcutis
|
| Necrobiosis lipoidica (NL) |
- Various shaped red–brown papules, plaques or patches with central atrophy (shiny, pale and thinned) involving the leg
- Usually not pruritic
|
11–65% of NL is associated with diabetes or prediabetes |
- Granulomatous inflammatory reaction and destroyed collagen (necrobiosis)
|
Case continued
A punch biopsy was performed. Histopathological analysis revealed compact orthokeratosis and mild spongiosis, with a reduced granular layer and an excoriated epidermis. Within the dermis there was a chronic perivascular mononuclear inflammation with extravasation of red blood cells and focal fibrosis with plump fibroblasts, in line with PPPD (Figure 2). No amyloid was evident on special stains.
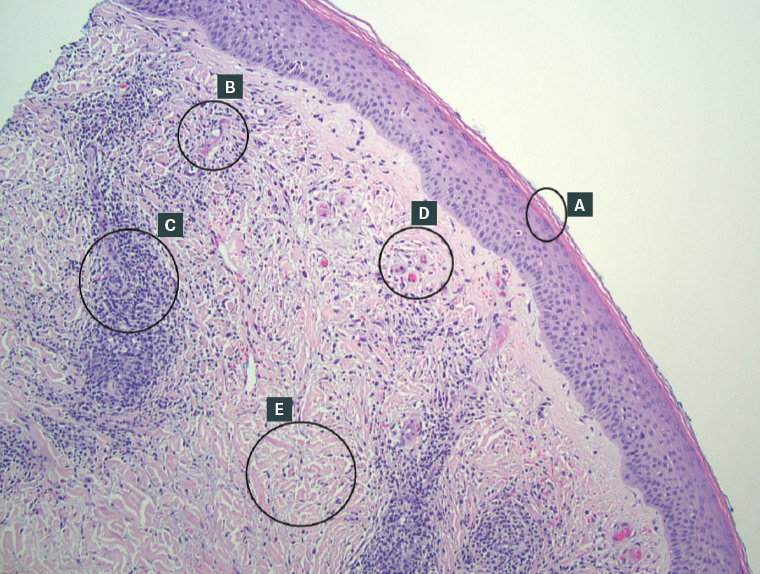
Figure 2. Histology of pretibial pruritic papular dermatitis. A. Compact orthokeratosis. B. Thickened blood vessel wall without vasculitis. C. Chronic perivascular inflammation. D. Congested blood vessels with extravasation. E. Dermal fibrosis with plump fibroblasts. (Haematoxylin and eosin stain, original magnification ×40.)
Question 2
What is PPPD and what is its epidemiology?
Question 3
What is the aetiopathogenesis of PPPD?
Question 4
What is the treatment for PPPD?
Answer 2
PPPD is a papular dermatitis of the leg, characterised by small pruritic bumps (papules), involving the pretibial zone of the leg. It is thought to arise from chronic rubbing. PPPD was first reported in 2006,
3–5 and is likely an under-reported condition. As such, epidemiological data are limited. Based on the two case series that are available (n=44+38=82),
3,4 the median age of onset is 50–60 years, with female dominance (1:3).
Answer 3
Little is known about the aetiopathogenesis of PPPD. Chronic gentle rubbing is considered to precipitate this condition.
3–5 Annessi et al, who first described PPPD, proposed for the aetiology a combination of multifactorial causes: genetics, cutaneous xerosis, contact with irritants, the modality of rubbing, the skin area and emotional distress.
3
Answer 4
There is no standardised treatment protocol, but potent topical corticosteroids have been reported to be effective.
3–5 Relapse is common. General measures, such as soap avoidance and the regular use of emollients, are important. Recalcitrant or unmanageable cases will warrant referral to the dermatologist.
Case continued
This patient was treated with mometasone furoate 0.1% ointment with a good response, as seen in Figure 3. The pruritus improved in one week and the papules flattened in three weeks. We propose that the good response in this case resulted from the short history combined with the application of potent corticosteroids under overnight occlusion with Tubigrip (Joya Medical Supplies, Arundel, Qld, Australia). The condition was still stable without recurrence at the three-month follow-up. Itchy papular lesions of the leg can span several diagnoses, and establishing a correct diagnosis clinically is difficult at times. A biopsy is required if a diagnosis cannot be determined clinically.

Figure 3. The right leg after 3 weeks of treatment.
Key points
- Leg dermatoses with or without pruritus are common presenting problems.
- Practitioners are encouraged to familiarise themselves with the characteristic morphology, because this guides diagnosis and management. Biopsy is indicated if a clinical diagnosis cannot be ascertained.
- PPPD is under-reported and under-recognised.
- Treatment with potent topical corticosteroids has been reported to be effective for PPPD, although the clinical response to this treatment might be variable.