Close to one million abdominal ultrasounds were requested in Australia between January and December 2022.1 Conservative estimates based on older analysis of general practitioner (GP) imaging-requesting behaviour would suggest that GPs were responsible for at least 250,000 abdominal ultrasounds during this period.2,3 Of these abdominal ultrasounds, close to 0.5% will reveal an incidental finding of the gallbladder or biliary tract,4 including cholelithiasis, choledocolithiasis, biliary duct dilatation, porcelain gallbladder, sludge, adenomyomatosis, cholesterolosis, gallbladder cancer (GBC) and gallbladder polyps (GBPs).5
There is no consensus among radiologists on the reporting of these incidental findings and their respective follow-up, and there is an increasing onus on GPs to be aware of these incidental findings and to follow them up appropriately.6
GBPs are an important entity that GPs are increasingly identifying incidentally, and this clinical review aims to raise awareness of this disease and to provide GPs with an approach to management.
Aim
There are a number of consensus statements on the management of GBPs.5,7–9 The aim of this paper was to review and summarise the current literature and these consensus statements in order to provide GPs with an approach to management based on the available guidance.
A literature search was performed on Medline using the OVID platform and the MeSH terms ‘gallbladder’ AND ‘polyp’. All relevant English-language articles from the past decade (2012–22) were considered, with references in the included papers also screened.
What are gallbladder polyps?
GBPs are polypoid lesions that arise from the gallbladder mucosa and project into the gallbladder lumen.7–9 Patients are asymptomatic for GBPs, and GBPs are usually incidental findings on abdominal ultrasound, which has a sensitivity of 84% and specificity of 96% for detecting GBPs.10 Ultrasound population prevalence studies indicate that 4.3–9.5% of the population will have GBPs.11,12
GBPs can be broadly categorised as non-neoplastic or neoplastic.13 Most GBPs (65–97%) are non-neoplastic and include cholesterol polyps, fibromyoglandular polyps, metaplastic pyloric glands forming polypoid collections and inflammatory polyps.13 Neoplastic polyps are rare and include intracholecystic papillary-tubular neoplasm (ICPN; previously referred to as adenomas) and adenocarcinomas.14–16 Most ICPNs are benign, but a small percentage (5–23%) are believed to contribute to GBCs.7,17 The pathological sequence of the progression of ICPNs to GBC is not well established.18
Why is identifying malignant GBPs important?
GBC is rare, with the worldwide incidence reported as three per 100,000 individuals.7 Prognosis is poor, with five-year survival rates reported as low as 5% globally19 and 28.8% in the US.20 Prognosis is greatly improved by early detection, with a reported five-year survival rate in the US for Stage 1 GBC of 82.7%.21 This is the basis for an emphasis on the detection and surveillance of GBPs, which might be either premalignant lesions for GBC or early GBC. Most GBCs manifest as masses, initially arising from flat dysplastic epithelium,10 but 15–25% of cases might arise from a GBP.12
Which GBPs are malignant?
Currently, differentiating which GBPs are malignant based on history, clinical examination and imaging characteristics is not possible.9 However, a combination of patient and polyp characteristics can be used to guide risk of malignancy, and international consensus statements base their recommendations on this.5,7–9
Patient characteristics that confer risk include age, a history of primary sclerosing cholangitis and being of North Indian, East Asian or North/South American Indigenous ethnicity. These groups have been associated with a higher incidence of GBC.5,7–9,22–24
Polyp characteristics that confer risk include the following:
- Polyp appearance: numerous studies have shown a higher percentage of neoplastic or malignant polyps with a sessile rather than pedunculated appearance.25–27
- Polyp multiplicity: solitary GBPs have been found to be independent risk factors for malignancy.25
- Polyp size: neoplastic polyps have been shown to be significantly larger (mean 18.1–21 mm) than non-neoplastic polyps (mean 4.1–12.6 mm).5,10,22 Malignant polyps appear to be even larger, with most measuring >20 mm.10 Recent systematic reviews and cohort studies corroborate that malignancy is often seen in GBPs >10 mm in size and almost absent in GBPs <6 mm in size.22,23,25,28–32 The risk of malignancy in GBPs >10 mm has been reported as 7.6–8.5%.22,23
- Polyp growth: increases and decreases in GBP size ≥2 mm are common and growth of this magnitude might be a part of the natural history of many polyps.29,30 Longitudinal cohort studies have also suggested that growth might not confer risk of malignancy.28–30,32,33 However, growth is conceptually concerning and there have been reports of GBC in GBPs that have grown from 7 to 16 mm over six months34 and from 2 to 18 mm over 24 months.35
- Concomitant cholelithiasis: although GBC is strongly associated with concomitant cholelithiasis,16 this has not been shown to confer risk of malignancy in GBPs.9
Management of GBPs in general practice
Patients with high-risk GBPs based on patient and polyp characteristics should be referred on for further input, including:
- patients with symptoms of biliary colic, who require further evaluation because their symptoms cannot be explained by the GBP8
- patients aged >50 years or with a history of primary sclerosing cholangitis or of North Indian or East Asian ethnicity5,8,9
- GPB ≥6 mm in size8
- GBP exhibiting growth ≥2 mm within 24 months7,8
- when recommended by the reporting radiologist.
Referrals should be made to the local general surgeon or general surgical department. Cases with a high degree of preoperative concern for malignancy should be referred to a hepatobiliary or upper gastrointestinal tract surgeon for further assessment and management.
The large majority of GBPs identified will not meet the aforementioned indications for referral and, if ≤5 mm in size, can be discharged from further follow-up.5,7–9 For low-risk GBPs 6–9 mm in size, all current consensus statements advise surveillance.5,7–9 However, the duration of surveillance varies greatly between each consensus statement, with some recommending surveillance for two years7,8 and others for five years.5 The largest longitudinal cohort study to date showed that the majority of GBCs were detected within one year of polyp detection and that after four years and 137,633 person-years of follow-up, only one additional GBC was detected.29 On the basis of these findings, prolonged surveillance longer than five years is unlikely to be beneficial to patients.
The above approach is shown in the decision tree in Figure 1.
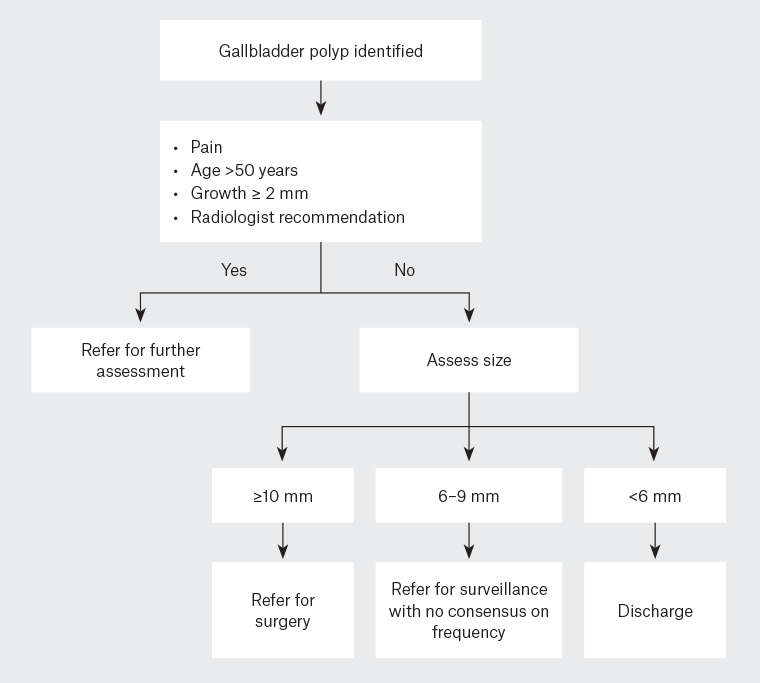
Figure 1. Approach to managing gallbladder polyps in general practice.
How are high-risk GBPs managed?
The risk from GBPs ≥10 mm in size is routinely addressed with laparoscopic cholecystectomy.5,7,8 Laparoscopic cholecystectomy is a safe procedure, with mortality ranging between 0.08% and 0.14% and the risk of bile duct injury ranging between 0.32% and 0.52%.36 These risks are greater in patients with increased comorbidity and operative complexity, and in such patients the surgical risk from cholecystectomy for GBP must be carefully weighed.
Concerning GBPs 6–9 mm in size can be further characterised using advanced imaging modalities, such as endoscopic ultrasound, colour Doppler imaging, contrast-enhanced ultrasound, contrast-enhanced magnetic resonance imaging and diffusion-weighted magnetic resonance imaging.8,9,37 These modalities have all shown advantages in characterising gallbladder polyp morphology, enhancement, vascularity and malignant invasion due to their high spatial and temporal resolution.9,37–39 Complex cases should be discussed in a multidisciplinary setting with radiologists present.
What guidelines exist on the management of GBPs?
Four recent consensus statements have been published on the management of GBPs: the World Federation of Ultrasound in Medicine and Biology position paper published in 2022;7 the Society of Radiologists in Ultrasound recommendations published in 2022;9 the European Society of Gastrointestinal and Abdominal Radiology, European Association for Endoscopic Surgery and other Interventional Techniques, International Society of Digestive Surgery–European Federation and European Society of Gastrointestinal Endoscopy joint guidelines updated in 2021;8 and the Canadian Association of Radiologists Incidental Findings Working Group recommendations published in 2020.5 The main findings of each of the consensus statements are summarised in Tables 1–4.
| Table 1. World Federation of Ultrasound in Medicine and Biology management strategies for gallbladder polyps7 |
| Criteria |
Guidance |
| Polyp size ≥10 mm |
Cholecystectomy |
| Polyp size 7–9 mm AND any risk factorA |
Cholecystectomy |
| Polyp size 7–9 mm |
Ultrasound at 6, 12 and 24 monthsB |
| Polyp size ≤6 mm AND any risk factorA |
Ultrasound at 6, 12 and 24 monthsB |
| Polyp size ≤6 mm |
Discharge |
AHistory of primary sclerosing cholangitis, Indian ethnicity and ultrasound high-risk features as specified in table 1 of Jenssen et al.7
BFor growth ≥2 mm, further evaluation with any of high-resolution ultrasound, contrast-enhanced ultrasound or endoscopic ultrasound may be performed.7 Discontinue surveillance if the polyp disappears, there is no growth ≥2 mm or no appearance of ultrasound high-risk features as specified in table 1 of Jenssen et al.7 |
| Table 2. Society of Radiologists in Ultrasound recommendations for gallbladder polyps9 |
| Criteria |
Guidance |
| ‘Extremely low-risk’ polypA |
| Polyp size ≥15 mm |
Surgical referral |
| Polyp size 10–14 mm |
Ultrasound at 6, 12 and 24 monthsB
Surgical referral acceptable alternative |
| Polyp size ≤9 mm |
Discharge |
| ‘Low-risk’ polyp |
| Polyp size ≥15 mm |
Surgical referral |
| Polyp size 10–14 mm |
Ultrasound at 6, 12, 24 and 36 monthsB
Surgical referral acceptable alternative |
| Polyp size 7–9 mm |
Ultrasound at 12 months |
| Polyp size ≤6 mm |
Discharge |
| ‘Indeterminate-risk’ polyp |
| Polyp size ≥7 mm |
Surgical referral |
| Polyp size ≤6 mm |
Ultrasound at 6, 12, 24 and 36 monthsB
Surgical referral acceptable alternative |
Polyps are categorised based on ultrasound appearance as ‘extremely low risk’ if they are pedunculated ‘ball-on-the-wall’ or pedunculated with thin stalk; as ‘low risk’ if they are pedunculated with a thick or wide stalk or sessile; and as ‘indeterminate risk’ if there is focal gallbladder wall thickening ≥4 mm adjacent to the polyp.9 The Society of Radiologists in Ultrasound recommends referring to gastroenterological specialist guidelines for patients with gallbladder polyps and primary sclerosing cholangitis.9
AIn the case of factors conferring a high risk of malignancy, such as local incidence or North Indian and North/South American Indigenous ethnicity, ‘extremely low-risk’ polyps can be considered as ‘low-risk’ polyps.9
BFor growth ≥4 mm in ≤12 months, surgical referral is recommended. For a decrease in polyp size ≥4 mm, discontinue surveillance.9 |
| Table 3. European Society of Gastrointestinal and Abdominal Radiology, European Association for Endoscopic Surgery and Other Interventional Techniques, International Society of Digestive Surgery–European Federation and European Society of Gastrointestinal Endoscopy updated joint guidelines on gallbladder polyps8 |
| Criteria |
Guidance |
| Polyp size ≥10 mm |
Cholecystectomy |
| Polyp size 6–9 mm AND any risk factorA |
Cholecystectomy |
| Polyp size 6–9 mm |
Ultrasound at 6, 12 and 24 monthsB |
| Polyp size ≤5 mm AND any risk factorA |
Ultrasound at 6, 12 and 24 monthsB |
| Polyp size ≤5 mm |
Discharge |
AAge >60 years, a history of primary sclerosing cholangitis, Asian ethnicity, sessile ultrasound appearance, wall thickening ≥4 mm.8
BFor growth ≥2 mm within the 24-month follow-up period, multidisciplinary discussion might be considered to decide on further surveillance versus cholecystectomy. Discontinue surveillance if there is no growth ≥2 mm or if the polyp disappears.8 |
| Table 4. Canadian Association of Radiologists Incidental Findings Working Group recommendations for gallbladder polyps5 |
| Criteria |
Guidance |
| Polyp size ≥10 mm |
Surgical referral |
| Polyp size 7–9 mm AND any risk factorA |
Ultrasound at 6 months, then every 12 months for 5 years |
| Polyp size 7–9 mm |
Ultrasound every 12 months for 5 years |
| Polyp size ≤6 mm |
Discharge |
| AAge >50 years, a history of primary sclerosing cholangitis, Indian ethnicity, sessile ultrasound appearance, single polyp.5 |
What lies in the future in this space?
Recent large cohort studies have found the same incidence of GBC in those with and without GBPs, and the same incidence of GBPs in those with and without GBC, challenging the very association between GBPs and GBC.3 Given the rarity of malignant GBPs and the rarity of neoplastic GBPs that transform into malignancy, further large prospective longitudinal studies are required to assess the cost-effectiveness and GBC risk reduction that GBP surveillance aims to address.
Conclusion
The management of GBPs is largely dictated by size, with minor variation between consensus statements. Small GBPs (≤5 mm) are almost universally recommended to be discharged from further surveillance due to their low risk of malignancy. Overmanagement of these small GBPs can cause patients harm through unnecessary anxiety, costs and surgery. Large GBPs (≥10 mm) are almost universally recommended to be referred for laparoscopic cholecystectomy due to their relatively higher risk of malignancy and the benefit from early treatment of GBC. Given the increasing detection of incidental GBPs, greater awareness of GBPs and guidance on their management is imperative for GPs.
Key points
- GBPs are being increasingly identified.
- Most GBPs are benign, but a few are at risk of becoming, or are, malignant GBCs.
- Age >50 years, North Indian, East Asian and North/South American Indigenous ethnicity and polyp size ≥6 mm are independently associated with greater risk.
- Cases meeting the above criteria should be referred to a general surgeon or general surgical department.