The clinical and cost-effectiveness of cardiac rehabilitation (CR) in preventing further morbidity and mortality following a cardiac event is well established.1–4 However, rates of CR referral, attendance and completion are staggeringly low. Global statistics indicate that less than 50% of eligible patients participate in CR programs.3,5–7 An Australian CR referral data audit between 2013 and 2015 showed that only 30% of eligible patients are referred for CR, with only 28% of those referred attending the program.8 Our recent audit of this dataset between 2016 and 2021 has shown modest improvement, with 32% of eligible patients being referred, 37% of these commencing CR and 78% of those commencing CR completing the program.9 Like global trends, both these audits show disproportionate outcomes by gender, location and socioeconomic status. Women, patients living in rural and remote areas and those of low socioeconomic status have worse statistics.10–12 Australians in rural and remote areas experience more cardiovascular disease (CVD) risk factors and have a greater risk of CVD hospitalisation and mortality.13,14 Poorer outcomes for these communities could be explained by the inverse care law, where the availability of healthcare is inversely related to the needs of the population. However, a study examining this concept in the delivery of CVD prevention services through community pharmacies revealed that services were more frequently available in rural communities and those with low socioeconomic status.15 Known barriers to CR for these populations include poorly defined referral pathways, no access to centre-based services and a general lack of awareness or acceptance of virtual services via telephone or video.16–18
Current tertiary hospital/centre-based CR is not ideal for patients in rural and remote areas due to limited access and extended care arrangements needed for them to attend. In addition, the system between hospital discharge and CR delivery is disconnected, resulting in low referral and attendance rates.
The work reported in this paper was part of the Country Heart Attack Prevention (CHAP) project, which applied the four-step model for large-scale knowledge translation, the RE-AIM (Reach, Efficacy, Adoption, Implementation, and Maintenance) framework,19,20 to develop and implement a model of care for CR in rural and remote Australia.21 CHAP is addressing four known barriers to CR translation into practice, namely:
- a lack of alternative modes of delivery for CR (through the co-design of a web-based CR program;22 participants in the codesign process had a mean age of 66 years and both genders were equally represented [males, 51%; females, 49%])
- low referral rates (by promoting endorsement of CR among clinicians through monthly continuing professional development sessions)
- heterogeneous quality of CR services (by promoting CR quality improvement through an accreditation program of CR services)
- a lack of mechanisms to sustain CR and secondary prevention for life (by proposing a business model that uses Medicare reimbursement through the chronic disease management plan [CDMP] to deliver CR in primary care).
This paper discusses the business model designed to address the last barrier, a lack of mechanisms to sustain CR and secondary prevention for life.
Aim
The proposed business model aims to incentivise the GP practice in managing the CR program by using the CDMP and existing Medicare items to improve CR access, especially for patients in rural and remote areas with no health centre‑based CR.
The business model
The business model was developed in the context of the cardiac rehabilitation referral system coordinated by the Integrated Cardiovascular Clinical Network (iCCNet) through the Country Access To Cardiac Health (CATCH) database. This current model of CR is shown in Figure 1.
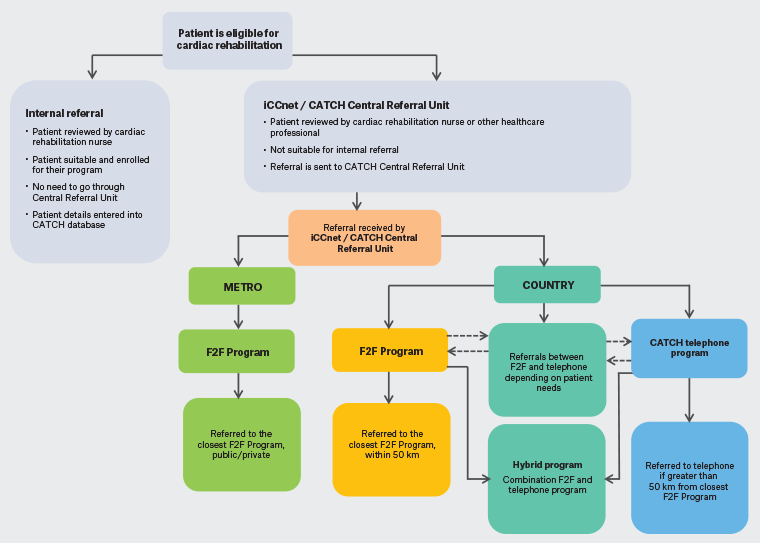
Figure 1. Delivery of cardiac rehabilitation in South Australia. Click here to enlarge
CATCH, Country Access to Cardiac Health; F2F, face-to-face; iCCnet, Integrated Cardiovascular Clinical Network; Metro, metropolitan; SA, South Australia.
In designing the business model, we used the general practitioner management plan (GPMP) for the delivery of CR as a chronic disease that requires management for life, which was rightfully stated by our participants in the codesign workshops as ‘heart health for life’.22 The use of GPMP items is standard care for a range of chronic conditions. The application of GPMP items to support local GP-led CR supported by a practice nurse and the CR nurse through CATCH and integrated with remote services through iCCNet is the adaptation used to deliver CR locally in a way that is accessible and cost-effective. This model was reviewed by Medicare prior to publication, with details provided elsewhere.23 We have interrogated Medicare items to identify what additional items patients in rural and remote areas are eligible for and can access through their GPs as the central pillar for CR (Figure 2). This model incorporates remote access to allied health practitioners (both through the GP and CATCH), home medication review by a pharmacist, active involvement of the practice nurse and the use of the web-based CR designed by the CHAP program as a bridge.
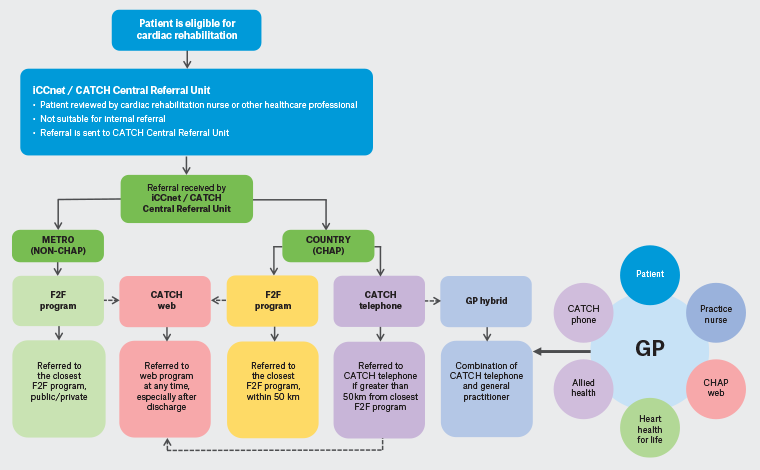
Figure 2. Proposed delivery of cardiac rehabilitation in South Australia with the general practitioner at the centre. Click here to enlarge
CATCH, Country Access to Cardiac Health; CHAP, Country Heart Attack Prevention; F2F, face-to-face; GP, general practitioner; iCCnet, Integrated Cardiovascular Clinical Network; Metro, metropolitan.
We then demonstrate the economic benefit of these additional items to the GP practice. This paper summarises and discusses the items presented in the model. A full report is provided on the CHAP website.23 Developing the business model and value proposition involved four major steps:
- Investigating operational practicalities in rural or remote GP practices for implementing a viable and achievable service model of CR care.
- A review of both published and the grey literature on previous business models for other GPMP programs run in a primary care setting.
- Interrogating Medicare items that supported the GPMP and accounted for costs to deliver the model in a GP practice.
- Interviewing experts from Medicare, rural GPs and practice nurses.
Two GP practices in rural South Australia (SA) were involved in designing and piloting this model: Clare Medical Centre in Burra and Waikerie Medical Centre in the Waikerie.
Using the GPMP to develop the business model
In the proposed GPMP, four face-to-face comprehensive cardiovascular assessments are received at the practice at four milestones. The milestones proposed in the model and the activities involved in Phase I/II of CR at each step are summarised in Figure 3 and are as follows:
- Assessment 1: Pre-CR program assessment
- Assessment 2: Post-CR program reassessment
- Assessment 3: Six-month follow-up
- Assessment 4: 12-month follow-up.
The objective in Phase III is to provide continuity of secondary prevention delivered by a patient’s nominated GP and should support ongoing risk management, such as referral to self-management programs and other services that support the heart and general health of the patient. The service model in Figure 3 shows the opportunities for the practice to check up regularly with the patient to provide management and advice regarding their cardiac health and support behavioural changes.
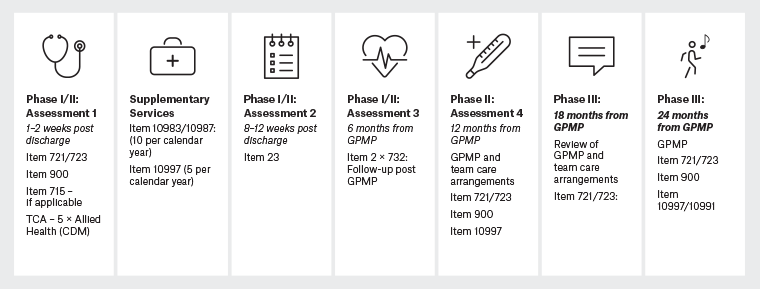
Figure 3. Phase I–III cardiac rehabilitation service delivery model led by the GP. Click here to enlarge
CDM, chronic disease management; CR, cardiac rehabilitation; GP, general practitioner; GPMP, GP management plan; TCA, team care arrangements.
Financial benefit
By implementing the business model, the net benefit to the practice, compared with claiming standard consultation Item 23 as the most likely item to otherwise be claimed, is $505 per patient for Phase I/II CR (Table 1) and $543 per patient for Phase III CR (Appendix 1) or $952 and $892 (Appendices 2,3), respectively, for patients of Aboriginal and Torres Strait Islander descent. This is mainly due to the additional reviews at the practice and increased involvement of the practice nurse in supporting the patient’s CR journey, alongside corresponding revenue for these items against the value of both the GP and practice nurses’ time. Appendices 2 and 3 show the additional items available for Aboriginal and Torres Strait Islander people. All costs are based on July 2021 costing of the respective Medicare Benefit Schedule (MBS) items.
| Table 1. Medicare items to support Phase II cardiac rehabilitation |
| |
Medicare item
description |
Medicare item no. |
RebateA ($) |
PN time (min) |
PN costB ($) |
GP time (min) |
Net value (less PN cost; $) |
Baseline value GP time (standard consult; $) |
| Initial assessment 1 |
| |
Preparation of GPMP |
721 |
152.50 |
45 |
42.19 |
15 |
96.25 |
39.75 |
| Pre-CR assessment |
Cardiac assessment |
|
|
15 |
14.06 |
|
|
|
| Week 1–2 post-discharge assessment |
Coordination team care arrangements |
723 |
120.85 |
|
|
|
120.85 |
|
| GP practice |
Initiate home medication review (billed at a later date) |
|
|
|
|
|
|
|
| Subtotal |
217.10 |
39.75 |
| CR program 6- to 10-week duration – patient choice of CR delivery |
| Reassessment 2 |
| |
Level B GP consultation |
23 |
39.75 |
|
|
15 |
11.63 |
39.75 |
| Post-CR reassessment |
Care plan follow-up: PN (see additional services below) |
10997 |
12.70 |
15 |
14.06 |
|
–15.43 |
|
| Week 8–12 post-discharge assessment |
Cardiac assessment |
|
|
15 |
14.06 |
|
– |
|
| |
Bill for home medication review |
900 |
163.70 |
|
|
15 |
163.70 |
39.75 |
| Subtotal |
159.90 |
79.50 |
| 6-month assessment 3 |
| |
Review of GPMP |
732 |
76.15 |
45 |
42.19 |
15 |
19.90 |
39.75 |
| 6-month review GPMP |
Cardiac assessment |
|
|
15 |
14.06 |
|
|
|
| GP practice |
Review of TCA |
732 |
76.15 |
|
|
|
76.15 |
|
| Subtotal |
96.05 |
39.75 |
| 12-month assessment 4 |
| |
Preparation of GPMP |
721 |
152.50 |
45 |
42.19 |
15 |
96.25 |
39.75 |
| GP practice |
Cardiac assessment |
|
|
15 |
14.06 |
|
|
|
| |
Coordination TCA |
723 |
120.85 |
|
|
|
120.85 |
|
| Subtotal |
217.10 |
39.75 |
| Additional services (if indicated) |
| |
Care plan follow-up: PN, five each calendar year (less one used above) |
10997 |
50.80 |
60 |
56.25 |
|
–5.45 |
|
| GP practice |
Video consult with cardiologist: PN |
10983 |
33.40 |
15 |
14.06 |
|
19.34 |
|
| Subtotal |
13.89 |
– |
| Total |
704.04 |
198.75 |
| Total net value to the practice ($) |
505.29 |
| Bulk-billing incentive items (if applicable; $) |
156.80 |
| Overall total ($) |
662.09 |
AMedicare Benefit Schedule July 2021 (www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Downloads-210701).
BAustralian Association of Practice Management National Biennial Practice Management Salary Survey 2019.
CR, cardiac rehabilitation; GP, general practitioner; GPMP, GP management plan; PN, practice nurse; TCA, team care arrangements. |
The business model focused on the net benefit compared with claiming standard consultation Item 23. The costs of room usage, equipment and other infrastructure are fixed costs and were not considered in the model; the only variable cost addressed was the cost of nurse resources. Details of the costing methodology are provided in the full report.23
Discussion
Implementation of the model has been trialled at Waikerie Medical Centre and Clare Medical Centre, SA, over the past three years. Uptake of the model in other centres is underway through the GP hybrid model in partnership with CATCH.
To disseminate this model, we conducted an in-person presentation at the Rural Doctors Association of SA meeting in Adelaide in August 2022. We also conducted an online workshop in October 2022 with the Rural Doctors Workforce Agency of SA. In these presentations with GPs and practice nurses, the primary concern was access to allied health services. Although these items are catered for in the Medicare schedule, there is limited access to allied health professionals across rural and remote Australia. Moreover, the waiting times to access these services are very long, which does not align with the needs of the CR patient.24 The in-built solution in the business model is to schedule remote allied health services through CATCH.
Barrier to successful implementation of the model
Maximising the financial benefit from the model is impacted by several factors, including patient compliance with all assessment milestones and practice nurse follow-up services. System barriers to success that must be considered include poor CR referral systems for patients in the rural areas, intersectional access to healthcare resulting from patient factors (ie patients have poor health literacy and understanding of what services they need or they do not have the time to seek services or access barriers [eg they live too far way to come to the GP]) and the limited availability of allied health professionals in rural areas (although there are provisions to have telehealth appointments in the proposed model, some patients are telehealth averse or lack access to the internet).16
Personal-level barriers to implementation include challenges to sustained long-term behaviour change, such as the patients’ self-efficacy and the lack of social support,25,26 and multimorbidity in this population because over 80% of people with heart, stroke and vascular disease have multiple chronic conditions and GPs might be reluctant to issue a new plan.27 However, if a patient already has a GPMP/team care arrangements (TCA) for another chronic condition in place, admission to hospital for a cardiac event would be a significant change that would qualify as exceptional circumstance under Medicare, enabling the GP to create a new GPMP/TCA.28
It is also important to note that in the Health Budget 2023 the Federal Government indicated its intention to act on the recommendations from the MBS Review Taskforce with respect to the GPMP (721), TCA (723) and associated Review (732) items.29 The key change will be the removal of the TCA Item 723 to reduce the red tape involved. The value of the Review item (732) will be increased to promote more regular review activity. These changes are expected in November 2024. Until the details of these changes are published and the value of rebates for GPMPs and associated reviews are known, we cannot forecast the impact on the business model.
Call to policy action
The most vulnerable populations in the community, including rural and remote patients, have historically been underfunded and this, in addition to other factors, has contributed to their poorer outcomes. The hybrid fee-for-service model in general practice and allied health trumps a proactive prevention model because it is dependent on individuals’ health literacy and affordability.30–32 There is a limited supply of health professionals in rural and remote areas and some of the available services do not bulk bill, which presents an access barrier. To improve access, existing policy must support practitioners in these settings to bulk bill their services and initiate care for individuals with low health literacy. In addition, both short- and long-term policies to address costs to practitioners in rural settings and workforce uptake and retention need to be addressed.
Due to resource constraints, this model was codesigned with only two rural GP practices in SA. This model can be expanded to other chronic diseases, but there is a need for funding to develop bespoke adaptations to this process model with marginalised patients, some remote networks and Aboriginal and Torres Strait Islander community networks.
Conclusion
This proposed model has the potential to make CR more accessible, with the GP as the central point, coordinating patient care and available in a patient’s community without the need to travel to a tertiary hospital or major centre. This value proposition integrates CR and secondary prevention into primary care and provides a business case for implementing CR in the community led by the GP practice. However, interventions to address the personal, policy and intersectional barriers to CR and sustained long-term behaviour change for rural and remote patients need to be addressed.
Key points
- Approximately 70% of Australians do not attend CR after an acute cardiac event.
- Barriers include gender, socioeconomic status and access to programs.
- This is a value proposition to provide CR in the primary healthcare setting.
- The model uses the chronic disease care planning Medicare items.
- This model accrues a net benefit to the general practice of up to $505 and $543 per patient in Phase II and III CR, respectively.