Chest pain is a frequently reported symptom that presents in both primary care and emergency department settings. It has a broad differential diagnosis, ranging from benign musculoskeletal pain to life-threatening cardiac events. The presentation of chest pain in the community can be particularly challenging for healthcare providers because the underlying cause is not always immediately apparent. In addition, chest pain is a symptom that can cause significant anxiety for patients and can lead to increased healthcare utilisation and costs.
When evaluating patients with chest pain, it is important to accurately describe the nature of the discomfort to facilitate an appropriate diagnostic work-up. It is worth noting that patients might use a variety of terms to describe their chest discomfort, including pressure, tightness, squeezing, heaviness or burning. As such, using the term ‘chest discomfort’ rather than ‘chest pain’ might be more appropriate to accurately capture the nature of the symptom.
Patients exhibiting clinical signs of acute coronary syndrome (ACS; see Table 1) or other potentially life-threatening causes of acute chest pain in a primary care setting should be immediately transported to the emergency department.
| Table 1. Features of typical and atypical acute cardiac chest pain1–3 |
| Characteristics |
Suggestive of angina |
Less likely suggestive of angina |
| Quality |
Anginal symptoms are typically described as pain, discomfort, heaviness, tightness, pressure, constriction, squeezing in nature |
Sharp chest pain that increases with inspiration and lying supine is unlikely to be related to angina and more likely due to pericarditis |
| Onset and duration |
Anginal symptoms gradually build in intensity over a few minutes |
Chest pain that lasts for only a few seconds is unlikely to be related to ischaemia |
| Location |
Angina pectoris is often perceived as a retrosternal chest discomfort |
Pain localised at the tip of one finger, particularly over the left ventricular apex or a costochondral junction, or pain reproduced with movement or palpation of the chest wall or arms is unlikely to be caused by ischaemia |
| Radiation |
Angina typically radiates to the left arm, neck, or jaw |
Pain that radiates into the lower extremities is unlikely to be related to ischaemia |
| Provoking and reliving factors |
Physical exercise typically exacerbates anginal symptoms and dissipates over a few minutes with rest. Occurrence at rest or with minimal exertion associated with anginal symptoms usually indicates acute coronary syndrome
Relief of pain with nitroglycerin is not necessarily diagnostic of myocardial ischaemia and should not be used as a diagnostic criterion |
The provoking and relieving factors for non-anginal chest pain can vary depending on the underlying cause of the pain. For example, lying down with the head elevated might help relieve chest pain caused by gastroesophageal reflux. Musculoskeletal chest pain can be reproduced with movement or palpation of the chest wall or arms |
| Associated symptoms |
Common symptoms associated with myocardial ischaemia include dyspnoea, palpitations, diaphoresis, light-headedness, syncope or pre-syncope, upper abdominal symptoms or heartburn unrelated to meals and nausea or vomiting |
Tenderness in the epigastrium or in the right hypochondrium might suggest the origin of the pain to be gastrointestinal or hepatobiliary, respectively |
Assessment of chest discomfort
When assessing chest discomfort, it is essential to differentiate between serious and benign causes of discomfort. Although the relief of symptoms with nitroglycerin might suggest myocardial ischaemia, this is not a definitive diagnostic criterion because other conditions, such as oesophageal spasm, might also respond to nitroglycerin. Certain groups, such as women, elderly patients, those with dementia and individuals with diabetes, might not exhibit typical symptoms of ischaemic chest pain.2 In addition, patients experiencing distracting pain, such as from a concurrent hip fracture, might not accurately report or might underestimate their chest pain.4 The severity of chest discomfort symptoms is not always a reliable indicator of the seriousness of an underlying medical condition. Patients with acute chest pain or chest pain equivalent symptoms should seek medical care immediately. A comprehensive diagnostic evaluation is necessary to determine the underlying cause of chest pain, which might involve a combination of clinical evaluation, laboratory testing and imaging studies. For patients with acute or stable chest pain determined to be low risk, urgent diagnostic testing for suspected coronary artery disease is not needed.2
Non-cardiac chest pain is typically diagnosed after ruling out cardiac causes of chest pain through appropriate investigations. Frequently, non-cardiac chest pain originates from gastrointestinal sources, with both erosive and non-erosive gastroesophageal reflux disease being the most common factors. Other gastrointestinal causes include oesophageal motility disorders, oesophageal hypersensitivity, hiatus hernia, gastroduodenal ulcer, pancreatitis, biliary colic pain and cholangitis.5
Certain features in a patient’s medical history can indicate oesophageal causes, such as dysphagia, regurgitation and heartburn. For suspected gastrointestinal-related cases, an empirical trial of a proton pump inhibitor (PPI) might be indicated. If patients do not respond to PPI therapy, further investigation of the upper gastrointestinal tract becomes crucial.5
The aetiologies of pulmonary causes of chest pain include pneumothorax, pneumonia, pulmonary embolism, asthma, chronic obstructive pulmonary disease and malignancy.5
Depending on the underlying aetiologies, patients might have a history of asthma, chronic obstructive pulmonary disease, previous pulmonary embolism (PE), deep venous thrombosis or recent immobilisation, and might present with various symptoms, including dyspnoea, fever, cough, haemoptysis and weight loss.
Physical examination might reveal raised jugular venous pressure and other signs of congestive heart failure in PE and, in case of pneumothorax, pneumonia might show signs of reduced air entry, collapse or consolidation respectively. A chest X-ray can help reveal underlying aetiologies.
Care must be taken not to overlook the possibility of dual aetiologies of chest pain, where respiratory, musculoskeletal, gastrointestinal or cardiac causes of chest pain might co-exist simultaneously.
Although there are several life-threatening causes, chest pain usually reflects a more benign condition. Among those presenting to their primary care doctor with chest pain, the final diagnosis was not ischaemic heart disease in 83%.6
The epidemiology of chest pain in primary care and emergency department settings was reported as musculoskeletal, including costochondritis in 36% of cases, gastrointestinal in 19%, cardiac in 16%, stable angina in 10.5%, unstable angina or myocardial infarction (MI) in 1.5%, other cardiac in 3.8%, psychiatric in 8%, pulmonary in 5% and other/unknown in 16%.7
Life-threatening cause of chest pain
Patients presenting with chest pain and suspected serious underlying causes, such as ACS, PE, aortic dissection or pneumothorax, or those with unstable vital signs should be promptly referred to the emergency department for evaluation.
According to a study conducted by Fruergaard et al,8 of a group of 204 consecutive patients admitted to the coronary care unit with chest pain, ACS accounted for 31% of cases, PE was observed in 2% of cases and aortic dissection occurred in 1% of cases.
Most of the following conditions might produce non-specific electrocardiogram (ECG) changes and a positive troponin test, adding diagnostic confusion and uncertainty.
Acute coronary syndrome
The term ‘acute coronary syndrome’ refers to a spectrum of conditions compatible with acute myocardial ischaemia and/or infarction that are usually caused by an abrupt reduction in coronary blood flow. These conditions include unstable angina, ST-elevation MI (STEMI) and non-ST-elevation MI (NSTEMI).
The ECG remains the best initial test for evaluation of chest pain because it is rapid, inexpensive and provides critical diagnostic and prognostic information.3
It is recommended that patients with acute chest discomfort or other symptoms suggestive of MI receive an immediate 12-lead ECG (Figure 1) to rapidly identify those patients with an acute STEMI and consider emergency reperfusion therapy if clinically indicated. Patients with ongoing symptoms suggesting ACS and an unremarkable initial ECG should be sent to the hospital for serial ECGs to monitor for evidence of an evolving infarction.
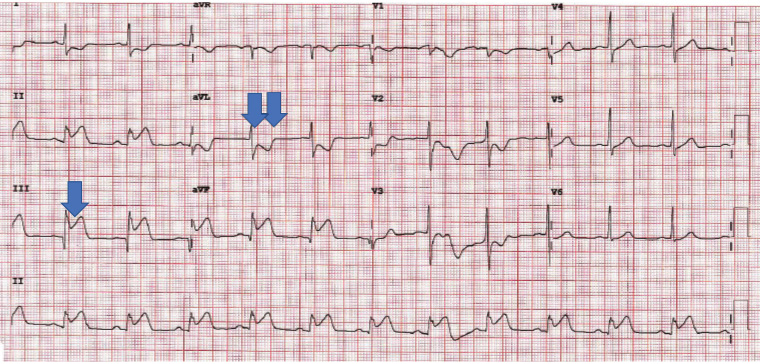
Figure 1. Electrocardiogram showing ST elevation in Leads II, III and aVF (single arrow) with reciprocal ST depression in Lead aVL (double arrow), consistent with acute inferior ST-elevation myocardial infarction.
NSTEMI lacks persistent ST elevation or new left bundle branch block. ECG changes might include transient ST-segment elevation (<20 minutes), ST-segment depression or T wave changes (Figure 2), or the ECG might be normal in approximately one-third of cases.4
The assessment of cardiac troponin is a highly sensitive means of detecting myocardial injury, used in both the diagnosis of acute MI and the assessment of risk in patients experiencing acute coronary symptoms. The fourth universal definition of MI emphasised the critical role of biomarker elevations in the diagnosis of acute MI.9 Unfortunately, troponin levels are also elevated in many conditions, including PE and acute aortic dissections.9,10
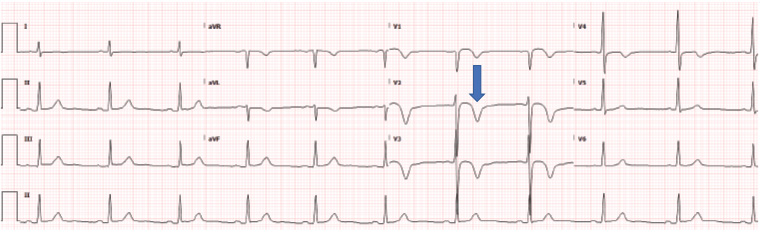
Figure 2. Electrocardiogram trace from a man aged 68 years with non-ST segment elevation myocardial infarction showing T wave inversion (arrow) in aVL and V1–V4. Coronary angiogram showing critical proximal left anterior descending artery stenosis.
Troponin testing might have a limited role in the primary care setting, except when working in an emergency department in the regional areas.
Patients who present with a history of a possible ACS but have been symptom free for at least 24 hours and who have no high-risk features of ongoing chest pain, syncope, heart failure and abnormal ECG could be assessed with a single serum troponin test. If patients have had ongoing symptoms within the preceding 24 hours or the troponin result becomes positive, they should be referred immediately to an emergency department for assessment.11
In a stable patient, when ACS and other serious causes of chest pain have been excluded, the investigations presented in Table 2 might be helpful in the community to investigate whether they might have coronary artery disease.
| Table 2. Investigating suspected coronary artery disease in stable patients9 |
| Test |
Indications |
Advantages |
Disadvantages |
| Exercise stress test |
Assessment of chest pain in patients with intermediate probability for CAD |
- Simple, widely available and low-cost technique
- Relatively high specificity
- Functional test
|
- Low sensitivity
- No or limited diagnostic value in the presence of LBBB, paced rhythm, WPW syndrome, LVH and use of digitalis
|
| Stress echocardiography |
Preferred non-invasive imaging technique for assessment of stable CAD |
- Low cost, wide availability and lack of radiation exposure
- Compared with nuclear imaging, stress echocardiography has similar accuracy and markedly higher specificity
|
- Interpretation dependant on operator experiences
|
| Myocardial perfusion scintigraphy using SPECT |
Indicated for assessing chest pain in patients who are unable to exercise adequately or have abnormal baseline ECG (eg LBBB) |
- Provides a more sensitive prediction of the presence of CAD than the exercise stress test
|
- Adenosine might produce bronchospasm in susceptible individuals
- Risk of radiation
|
| CAC scoring |
Indicated for quantitation of coronary artery calcification, a marker of atherosclerotic plaque burden |
- Useful in intermediate-risk patients, who are asymptomatic, to reclassify them into lower- or higher-risk groups
- An independent predictor of future MI and mortality
|
- Not useful in high-risk patients, patients with documented CAD and in symptomatic patients
|
| CCTA |
Useful in low- to intermediate-risk patients when initial exercise test is inconclusive |
- Provides additional information about the vessel condition, remodelling and plaque surrounding the lumen
|
- Difficult to interpret in the presence of coronary calcification, obesity, atrial fibrillation and heart rate >65 bpm.
- There has been a significant decrease in radiation dose from CCTA over time
|
| CAC, coronary artery calcium; CAD, coronary artery disease; CCTA, coronary computed tomography angiography; ECG, electrocardiogram; LBBB, left bundle branch block; LVH, left ventricular hypertrophy; MI, myocardial infarction; SPECT, single photon emission computed tomography; WPW, Wolff–Parkinson–White. |
Aortic dissection
Aortic dissection is a rare condition that can be difficult to diagnose and needs to have a high index of suspicion.
The typical presentation of aortic dissections involves an abrupt and intense tearing pain that spreads through the back.4,12
Hypertension is a common finding among patients with aortic dissections, and approximately 20% of cases might present with neurological deficits. Suspicions of aortic dissection might increase when there is a difference in blood pressure >20 mmHg between the two arms.
Pulmonary embolism
Symptoms of PE might include pleuritic chest pain (66%), dyspnoea (73%), cough (37%) and haemoptysis (13%).13
Risk factors associated with PE include recent surgery, trauma or travel with a history of immobilisation, malignancy, history of deep vein thrombosis (DVT) or PE, and hypercoagulable states. Most patients with PE present with a sudden onset of pleuritic chest pain or shortness of breath, whereas other presentations include syncope and haemoptysis.4
Physical examination findings for PE are typically non-specific, but an unexplained tachycardia, signs of DVT or congestive heart failure might indicate its presence. Tachypnoea might also be observed.4
ECGs are often abnormal but non-specific. The most common finding is sinus tachycardia, but other ECG findings suggestive for PE include right bundle branch block, T wave inversion in V1–3 and an S1Q3T3 pattern.4
D-Dimer tests are useful for ruling out PE in low- or intermediate-risk patients because they have a high sensitivity with a low false-negative rate. However, they also have low specificity with a high false-positive rate.4
A normal chest X-ray with hypoxia might suggest PE. Computed tomography pulmonary angiography and ventilation/perfusion scanning are recommended for low- or intermediate-risk patients with positive D-dimer tests or high-risk patients.4
Echocardiography is useful for suspected PE cases and might reveal right heart dilatation, increased right ventricular systolic pressure and dysfunction and sometimes the presence of a large pulmonary artery or a clot.4
Tension pneumothorax
In the case of tension pneumothorax, chest pain symptoms typically appear abruptly, localised to the side of the pneumothorax, and a pleuritic quality. In addition, dyspnoea is frequently experienced.
The classic examination findings are reduced, or absent, breath sounds on the affected side and hyper-resonance on percussion.
In a patient with suspected pneumothorax, chest X-ray is the investigation of choice.9
Ruptured oesophagus
The classic presentation of spontaneous oesophageal rupture is severe vomiting or retching followed by acute, severe chest or epigastric pain.4
Conclusion
In conclusion, chest pain is a common symptom that can range from benign to life-threatening causes, making it a challenging presentation for healthcare providers. Patients might use various terms to describe their discomfort, which underscores the importance of obtaining an accurate description and thorough examination, including vital signs, to facilitate appropriate diagnostic work-up.
When evaluating patients with chest pain, it is essential to differentiate between serious and benign causes of discomfort, and it is crucial to identify potentially life-threatening causes and evaluate the need for emergency care before considering other common causes of chest pain.
For patients with acute or stable chest pain determined to be at low risk of cardiac cause, urgent diagnostic testing for suspected coronary artery disease is not needed. A comprehensive diagnostic evaluation is necessary to determine the underlying cause of chest pain, which might involve a combination of clinical evaluation, laboratory testing and imaging studies. It is crucial to note that the severity of chest discomfort symptoms is not always a reliable indicator of the seriousness of an underlying medical condition. Finally, patients with acute chest pain or chest pain equivalent symptoms, with a potential serious cause, should be sent to emergency care immediately.
Key points
- Chest discomfort in the community is a frequently reported symptom. It has a broad differential diagnosis, ranging from benign musculoskeletal pain to life-threatening cardiac events.
- In cases where coronary artery disease is not suspected, it is preferred to use the term ‘non-cardiac’ rather than ‘atypical’. To provide a more accurate and informative description of the potential underlying cause of chest pain, it is recommended to use terms such as ‘cardiac’, ‘possibly cardiac’ or ‘non-cardiac.’
- Careful evaluation of patients with chest pain should include a detailed history, physical examination and appropriate investigations to determine the cause and management of the patient’s symptoms.
- The ECG remains the best initial test for chest pain evaluation because it is rapid, inexpensive and provides critical diagnostic and prognostic information.
- High-sensitivity troponin has a limited role in the community setting but remains an important biomarker in assessing and risk stratifying chest discomfort symptoms. It also enables the safe exclusion or ‘rule out’ of MI within one to two hours for most patients, thereby reducing unnecessary hospitalisation and promoting efficient resource use.