The World Health Organization (WHO) defines adolescence as the phase of life between childhood and adulthood, from ages 10 to 19 years.1 During this period, adolescents experience rapid physical, cognitive and psychosocial growth. There is also significant hormonal and somatic development, accompanied by substantial nonlinear changes in brain structural and functional organisation and behaviour.2 These changes contribute to biological alteration in the sleep–wake cycle, often exacerbated by conscious behaviours during a stage of increased autonomy and independence.3 Screen-based activities that often delay bedtime or truncate total sleep time are additional environmental causes that contribute to insufficient sleep for many adolescents.4 Combined, these biological, psychosocial and environmental factors result in few adolescents achieving the recommended 8–10 hours per night for optimal health outcomes.5
Aim
This article aims to provide an overview of the sleep issues that commonly arise during adolescence, based on the experience of Australian paediatric specialists, and discusses the importance of addressing these issues to avoid the associated significant health consequences. Specific differences relating to individual cultural groups within Australia are outside the scope of this article. Instead, an overarching approach to managing adolescent sleep problems encountered in primary care is provided with reference to additional resources.
Adolescent sleep patterns
The Growing Up in Australia Longitudinal Study of Australian Children found that around one-quarter of those aged 12–15 years and half of those aged 16–17 years are not getting enough sleep.6 During adolescence, sleep typically becomes more irregular and timed later in the day. This sleep delay is partially due to a biological delay in the circadian rhythm, or body clock, that typically occurs at the onset of puberty. However, technology use, late-night homework and sleeping in on weekends can all delay sleep timing further.7–9 Over several nights, insufficient sleep might lead to daytime sleepiness, impaired cognition, irritability and low mood, with poorer school performance, increased risk-taking behaviour and elevated anxiety and depression symptoms all reported.10 These associations can substantially reduce quality of life.
Optimising sleep hygiene can stabilise the circadian rhythm and stop sleep timing from drifting too late. Strategies include maintaining similar bed and waking times on weekdays and weekends (<30-minute difference).11 Avoiding sleeping in on weekends and exposure to natural morning sunlight is helpful. Dimming the lights in the evening, avoiding technology use for the hour before bedtime and keeping devices out of bedrooms or on silent mode to avoid checking them during the night can be beneficial.12 Regular mealtimes, particularly eating breakfast on waking, are also important cues and regulators of circadian rhythm. Daily exercise and avoiding stimulant drinks and medications in the late afternoon and evening are other important contributors to a healthy sleep pattern. Studies have shown that adolescents whose parents set a firm bedtime and waking time get more sleep and have improved daytime functioning.13 However, this might be difficult to impose on older, more autonomous adolescents.
Every consultation with an adolescent is an opportunity to actively screen for sleep problems and provide education about healthy sleep. Various paediatric sleep screening tools can be used in the primary care setting, including the BEARS (Bedtime problems; Excessive daytime sleepiness; Awakenings during the night; Regularity and duration of sleep; Sleep disordered breathing) mnemonic (Table 1)14,15 and the ABCs of SLEEPING tool (Age appropriate sleep duration; regular Bedtimes; Consistent sleep/wake routine; Scheduling daytime activities appropriately; Location of the bedroom is cool, dark, quiet and reserved only for sleeping; no Electronics in bed or before bed; Exercise and diet; Positive parenting; Independent sleep onset; biophysical and emotional Needs are met for a Great sleep).11 More detailed adolescent-specific questionnaires might also help assess the effects of poor sleep.16
| Table 1. BEARS screening tool for adolescents |
| Categories |
Example questions |
| Bedtime problems |
Do you have any problems falling asleep at bedtime? |
| Excessive daytime sleepiness |
Do you feel sleepy a lot during the day? At school? While driving? |
| Awakenings during the night |
Do you wake a lot during the night? |
| Regularity and duration of sleep |
What time do you go to bed on a school night? At weekends? How much sleep do you usually get? |
| Sleep disordered breathing |
Ask family members about snoring. |
Adapted from Bruce ES, Lunt L, McDonagh JE. Sleep in adolescents and young adults. Clin Med (Lond) 2017;17(5):424–28, with permission from the Royal College of Physicians.15
BEARS, Bedtime problems, Excessive daytime sleepiness, Awakenings during the night, Regularity and duration of sleep, Sleep disordered breathing. |
Sleep disorders in adolescence
Delayed sleep–wake phase disorder
Delayed sleep–wake phase disorder (DSWPD)17 is a circadian rhythm sleep disorder prevalent in adolescents, affecting an estimated 3% of individuals with little racial differences.18.19 DSWPD occurs when the mismatch between sleep patterns and social obligations is profound and leads to daytime impairment.20 DSWPD is characterised by sleep timing that is typically delayed by two to six hours relative to the patient’s desired sleep timing, resulting in chronic insufficient sleep that is poor in quality. This is often because sleep is attempted when the circadian rhythm promotes wakefulness. DSWPD is treated with appropriately timed bright light and/or exogenous melatonin administration.21 Cognitive behaviour therapy, ideally delivered by a sleep psychologist, might also be beneficial.
Insomnia
Insomnia refers to decreased sleep due to difficulty falling asleep, difficulty staying asleep or awakening too early.21 Insomnia in adolescence is common. The term ‘insomnia disorder’ is sometimes used to refer to chronic perceived dissatisfaction with sleep that is over and above the typical changes in sleep in adolescents.22 It is estimated that almost one-quarter of adolescents experience insomnia.23 Insomnia is more common in females and older adolescents, with a prevalence comparable to other major psychiatric disorders (eg depressive disorders).22 Diagnosing insomnia in adolescence is particularly challenging because diagnosis requires an ‘adequate opportunity to sleep’,22 which, in many adolescents, does not occur due to external factors already described. Psychophysiological insomnia is characterised by the inability to fall asleep or stay asleep due to the intrusion of anxious or stressful thoughts in bed.17 In adults, this is most effectively treated with cognitive behavioural therapy for insomnia (CBTi). More rigorous research is needed to support the use of CBTi specifically in adolescents with insomnia,21 although there are evolving resources in this area. A good example is the Sleep Ninja app recently launched by the Black Dog Institute.24
Factors contributing to insufficient adolescent sleep
Twenty-four-hour connectivity
Most adolescents rely on the internet as their primary method of communication and view this as a fundamental aspect of their daily life.25 Excessive digital technology use with ‘24-hour connectivity’ significantly contributes to adolescent sleep restriction. Electronic media use at bedtime might affect sleep through several mechanisms: the direct reduction of time available to sleep, awakenings caused by incoming messages/calls overnight, the melatonin suppression effect of screen light and the presleep psychophysiological arousal secondary to engagement and content of the viewed media, which prevents the psychophysiological withdrawal necessary to fall asleep.4,22 This latter effect perpetuates the development of chronic insomnia.22
Recent studies have attempted to determine the factors that influence the continued use of devices at bedtime in adolescents and have identified ‘missing out’ and ‘norms and expectations’ as two important drivers of this behaviour.26,27 Adolescents in these studies described concerns around the risk of offline peer exclusion from missing out on online interactions and the fear of social disapproval from violating norms around online availability and prompt responses.26 Such insights are crucial for clinicians and help provide context to the importance of connectivity for adolescent patients who have grown up surrounded by digital information and entertainment on screens.28 For these young individuals, screens (screen time) are a significant part of contemporary life, and the increased social connectedness and belonging they gain through online peer interactions is perceived to outweigh the detrimental effects of sleep deprivation.26,28 A key focus for improving adolescent sleep health needs to include the development of interventions that consider the cognitive drivers that underpin day-to-day decisions that result in poor sleep.27
Another consideration is the association between cyberbullying, poor mental health and sleep quality.29 Cyberbullying is common, with studies from several countries reporting that the average adolescent victimisation prevalence rate is approximately 15%.30 Adolescents report higher rumination and inadequate sleep, which persists for as long as two years after being victimised online. Therefore, enquiring about cyberbullying is an important component of consultations with adolescents, who might require specific support to address this issue.25
Chronic health conditions
Sleep loss might exacerbate a chronic condition, and disease-related symptoms might disturb sleep. Significant evidence now links several chronic diseases in children with worse sleep. This includes allergic rhinitis, asthma, cancer, cystic fibrosis, epilepsy and type 1 diabetes.31 Children with chronic pain or rheumatological conditions are also significantly at risk, with shorter sleep duration, poorer sleep quality and more night wakings all reported compared with healthy peers.31,32 Acknowledging the bidirectional relationship between sleep quality and chronic disease and pain highlights the importance of optimising sleep problems and pain, which are often modifiable.
Drugs and alcohol
Australian data show that the prevalence of nicotine, alcohol or cannabis use among young people, either experimentally or recreationally, is relatively high.33 This might contribute to sleep pattern changes and subsequent chronic sleep loss. Sleep deprivation among adolescents can also increase risk-taking behaviours, including substance use.34
Nicotine: Tobacco and e-cigarettes
Although the prevalence of tobacco smoking in young people is decreasing, there has been a steep increase in the use of e-cigarettes (vaping).33,35 Nicotine is the primary psychoactive component found in tobacco cigarettes and most e-cigarettes and is thought to be a mechanism linking smoking and vaping with sleep disturbances.36 Respiratory problems might also mediate this association.37 Nicotine-dependent adolescents report poor sleep quality and increased use of sleep medication.38 There is evidence from a large number of studies in adolescents using tobacco cigarettes that the frequency of recent smoking (eg in the past 30 days) is associated with greater sleep problems, such as difficulty initiating sleep,39 shorter sleep duration and later sleep onset and offset.40–42 Recent studies evaluating sleep in adolescents using e-cigarettes have also found a tendency for shorter total sleep time and difficulty initiating asleep.40,43,44 Nicotine cessation is associated with sleep disturbance in addition to other withdrawal symptoms.45,46 It is important to provide anticipatory advice about sleep when counselling adolescents to quit.
Marijuana
Marijuana (or cannabis) is Australia’s most widely used illicit drug. Several studies have assessed the relationship between marijuana use and adolescent sleep disturbances.40–42,47,48 A variety of problems are described, including difficulty initiating and maintaining sleep, waking up feeling tired and sleeping more on weekends.
Alcohol
Alcohol consumption initially causes sleep-inducing effects; however, during sleep, alcohol has a stimulating effect, which disturbs normal sleep stages. This results in sleep fragmentation and early morning awakening.49 In adolescents, alcohol use, particularly binge drinking, is significantly associated with sleep disturbances such as difficulty initiating sleep, difficulty maintaining sleep, shorter sleep duration and snoring.50–52 There is a growing understanding that adolescents who report sleep problems, such as disturbances in circadian rhythm, might also be more likely to use alcohol to initiate sleep and are at higher risk for escalation of alcohol problems.47,53
Caffeine
Caffeine is the most widely used psychoactive drug worldwide and is primarily ingested via dietary sources such as coffee, tea and energy drinks. According to evidence from a 2018 national survey of Australian adolescents, 8% of those aged 12–17 years regularly consume energy drinks.54 Energy drinks might also contain other stimulant compounds. Caffeine has alerting properties, with acute administration close to normal bedtime resulting in increased sleep latency and decreased total sleep time, including decreased slow-wave sleep.55 Somewhat ironically, adolescents report consuming caffeinated drinks to counteract the effects of insufficient sleep.56.57 Adolescents with attention deficit hyperactivity disorder (ADHD) represent a particularly high-risk group because they are more likely to consume high levels of caffeine and experience sleep disturbance with consumption.58,59
Prescribed medications
Both over-the-counter and prescription medications can affect sleep.31,60 Antihistamines taken by some adolescents to induce sleep might result in excessive daytime sleepiness and can worsen restless legs syndrome. Other hypnotic medications should not be prescribed routinely in the paediatric age group, and consideration should be given to their side effect profile and risk of daytime sleepiness. Benzodiazepines, for example, might cause worsening of sleep disordered breathing (SDB), alterations in sleep architecture and rebound insomnia on withdrawal.58 Opioid medications used for pain management can (also) reduce respiratory drive and worsen SDB and should be used with caution in those with underlying respiratory conditions. If any hypnotic medications are prescribed, they should be used in conjunction with behavioural sleep strategies for optimising sleep and circadian health. Once behavioural and cognitive strategies have improved sleep, medication requirements should be re-evaluated to consider ongoing need and ensure safe discontinuation of these treatments. Commonly prescribed medications might also result in delayed sleep onset (eg stimulant medication for ADHD, oral steroids), disrupted sleep (eg some antidepressants and anticonvulsants) and consequent daytime sleepiness in adolescents.61
Melatonin
Melatonin is an endogenous hormone produced by the pineal gland responsible for regulating the sleep–wake cycle. Misalignment of the endogenous melatonin rhythm with the desired sleep–wake timing results in difficulty falling asleep and waking in the morning.62 Exogenous melatonin administration has a primary chronobiotic effect, shifting the circadian phase by advancing or delaying it within the day–night cycle, depending on when it is administered relative to circadian timing.
A recent meta-analysis including seven randomised controlled trials concluded that melatonin was an effective and tolerable drug in the short-term treatment of insomnia in children and adolescents.63 However, the authors also highlighted that more, higher-quality studies were required, especially in adolescents, to investigate the efficacy and safety of melatonin.63 Regardless, because of its benign safety profile, exogenous melatonin has increasingly been used off-label to treat paediatric insomnia globally, despite being approved only in specific indications and populations and not in all countries.64 In the USA, melatonin is not approved by the US Food and Drug Administration (FDA) and is instead sold over the counter as a dietary supplement.65 Another recent study showed that most melatonin gummy products in the USA were inaccurately labelled, with most products exceeding the declared amount of melatonin and containing concerning levels of cannabidiol (CBD).65 In Australia, melatonin is approved for use and must be prescribed. Specialists should warn against purchasing melatonin products from overseas. Specialists generally consider melatonin to assist adolescent patients with insomnia when first-line therapy with sleep hygiene measures and behavioural and cognitive treatment approaches have failed and other underlying sleep disorders have been ruled out. In addition, melatonin administration alongside light therapy and cognitive behavioural techniques is often used for those adolescents who meet the criteria for DSWPD.
Obesity
Australian data from 2017 to 2018 demonstrate that approximately one-quarter of Australian children aged 5–17 years are overweight (17%) or obese (8%).66 This is consistent with the significant increase in the prevalence of obesity, which has been seen worldwide, leading to the declaration of a global epidemic by the WHO.67
Sleep behaviours observed in adolescents might be associated with the increasing prevalence of obesity in this age group.68 Less sleep is consistently linked with unhealthy dietary habits, including larger portion sizes, increased perceived hunger, higher calorie food choices and increased food and sugar-sweetened beverage intake.69,70 This is thought to be mediated, at least in part, by changes in metabolic hormones, such as leptin and ghrelin.68 Poor sleep quality and altered patterns of sleep duration (eg later bedtimes on weekends than weekdays, termed ‘bedtime shift’ and ‘social jet lag’, referring to sleep deficits that accumulate during the week and result in oversleeping during the weekend) might also be risk factors for obesity, leading to dysregulation of circadian rhythms and subsequent altered metabolism.68 Some of the proposed mechanisms for poor sleep and obesity and possible obesogenic behaviours seen in those with poor sleep are summarised in Table 2.68
| Table 2. Proposed mechanisms and possible obesogenic behaviours in poor sleep and obesity |
| Proposed mechanisms |
Obesogenic behaviours |
Evening chronotype:
- With early wake time
- Social jetlag
|
Unhealthy food choice:
- Sugar-sweetened beverages
- Fast food
- High-calorie snacks
- Excessive portion size
|
| Bedtime shift |
Increased food consumption |
| Hormonal alterations:
|
Increased perceived hunger
Food preoccupation |
| Adapted from Gohil A, Hannon TS. Poor sleep and obesity: Concurrent epidemics in adolescent youth. Front Endocrinol (Lausanne) 2018;9:364, with permission from Frontiers Media.68 |
Prevalence rates of obstructive sleep apnoea (OSA) in children and adolescents with obesity range between 13% and 59%.71,72 The precise aetiology for OSA in this population is uncertain but is proposed to result from multiple interacting factors that increase the risk in this cohort. This might include adenotonsillar hypertrophy, altered neuromuscular tone with increased upper airway collapsibility during sleep and central adiposity, causing an excess mechanical load on the chest wall, which results in decreased chest wall and diaphragmatic excursion, leading to reduced functional residual capacity and tidal volumes.72 OSA might further perpetuate the weight gain cycle by causing greater sleep disruption and shorter overall sleep duration, both of which are linked to obesity risk.73,74
Treatment of OSA in adolescents with obesity should be prioritised because the effect of comorbid OSA is significant. OSA is a risk factor for cardiovascular, metabolic and neurocognitive complications and negatively affects quality of life.72 However, it is well recognised that children with obesity benefit less from first-line treatment with adenotonsillectomy compared with children of normal weight,75,76 with some studies reporting residual OSA rates of almost 50% postoperatively.72 Other evidence-based treatment options considered for OSA in children and adolescents with obesity include weight loss and treatment with continuous positive airway pressure or bilevel positive airway pressure.72 Adherence to positive airway pressure therapy is often significantly challenging in this group, who do not always perceive a benefit. However, improved attention and academic function have been demonstrated in adolescents who adhere to therapy relative to those who do not.77 In Australia, bariatric surgery to treat obesity is rarely available for adolescents but might be a consideration if non-surgical measures have been tried without success.72 Other promising treatments are the incretin medications (eg semaglutide), used to treat obesity in adults. Trials show that these medications in addition to lifestyle interventions result in greater weight loss than lifestyle changes alone.78
Negative consequences of poor sleep in adolescents
Many somatic effects of poor sleep during adolescence have already been discussed, including the effect on obesity risk and the associated increased prevalence of OSA alongside metabolic and cardiovascular dysfunction. Cognitive function is also affected, with poorer attention, learning and memory.21 The relationship between sleep and common adolescent psychiatric disorders is complex. Mood and risk of depression are correlated with sleep duration, with self-reports of poor mood, emotional dysregulation and self-harm all higher in those with sleep restriction.21 However, because poor mood and anxiety can also worsen insomnia, this association is likely bidirectional. As such, it is important to evaluate sleep problems in individuals who present with a suspected mood disorder because sleep problems are potentially treatable and might be exacerbating the mood disturbance. Similarly, it is essential to recognise that poor sleep might be a symptom of anxiety or depression. In the adolescent patient, this should not be ignored and might represent a warning sign for increased risk-taking behaviours.16
Sleep and motor vehicle accidents
Multiple studies have now reported that young drivers (aged <25 years) are at the highest risk for sleep-related motor vehicle crashes, with a large Australian study demonstrating that sleeping six or fewer hours per night is associated with an increased risk of motor vehicle crashes among young drivers.79 Young drivers have frequently reported driving while tired, with 51% of young American drivers reporting driving while drowsy and 9% reporting nodding off while driving in the past year.79 This international data highlights the importance of discussing and addressing sleep problems with adolescent patients. Educating adolescents on the increased risk of fatal accidents when driving while tired is important. Certain sleep disorders might additionally increase the risk of motor vehicle accidents, such as untreated OSA80 and narcolepsy.81 Narcolepsy is important to consider in adolescent patients because the onset of symptoms occurs during childhood and adolescence in 50% of cases,82 and diagnosis has specific implications for driving. Referral to a sleep specialist should be considered once other causes of excessive daytime sleepiness have been excluded.
Managing sleep problems in adolescents
Sleep education is often the first step in managing adolescent sleep issues. A review of studies examining the effectiveness of sleep education in behaviour change found that it was important to educate parents and the young person, given that environmental and cultural factors influence sleep in the home.83 Furthermore, it is important to identify specific issues for the individual, explore their understanding of sleep and tailor sleep education rather than simply providing generic advice about sleep hygiene. An approach to assessing and managing sleep problems in adolescents is provided in Figure 1; some examples of additional online resources that provide specific sleep hygiene advice relevant to adolescents are listed in Appendix 1. For more complex sleep difficulties, where mood disturbances or an additional underlying diagnosis is suspected, referral to a sleep physician or other relevant specialist (eg a psychiatrist or psychologist) is recommended. Similarly, persistent symptoms of OSA should prompt specialist referral.
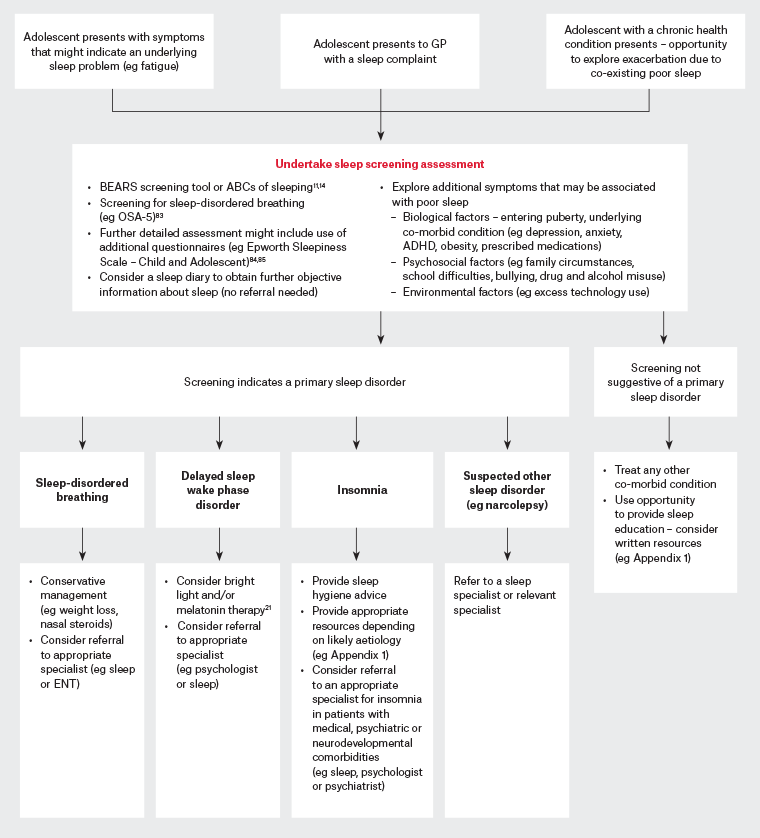
Figure 1. An approach to assessing and managing sleep problems in adolescents. Click here to enlarge
ABCs of SLEEPING, Age-appropriate sleep duration, regular Bedtimes, Consistent sleep–wake routine, Scheduling daytime activities appropriately, Location of the bedroom is cool, dark, quiet and reserved only for sleeping, no Electronics in bed or before bed, Exercise and diet, Positive parenting, Independent sleep onset, biophysical and emotional Needs are met for a Great sleep; ADHD, attention deficit hyperactivity disorder; BEARS, Bedtime problems, Excessive daytime sleepiness, Awakenings during the night, Regularity and duration of sleep, Sleep disordered breathing; ENT, ear, nose and throat; GP, general practitioner; OSA, obstructive sleep apnoea.
Conclusion
Adolescence is a life phase in which the opportunities for health are considerable and future patterns of adult health are established. The physiological and psychosocial changes during this critical transition period make this population vulnerable to sleep disorders and their associated negative consequences. In addition, sleep problems might be the presenting feature of an underlying psychiatric disorder that emerges during this period. Proactively assessing sleep is essential for any clinician who encounters young people regularly. Identifying and managing sleep problems in adolescents is important to optimise wellbeing and avoid longer-term health consequences. Sleep and psychosocial screening tools and online education resources can be helpful in the primary care setting.
Key points
- Healthy sleep is essential (to maintain physical health, emotional wellbeing and school performance), although many adolescents do not get the recommended 8–10 hours.
- Understanding the potential short-term and long-term consequences of sleep restriction and irregularity, as well as the factors contributing to sleep loss in adolescents, is key in counselling patients and families in the general practice clinical setting.
- Every consultation with an adolescent is an opportunity to actively screen for sleep problems, provide advice for healthy sleep and support parents to help their teenager get adequate, good-quality sleep.