Background
Obstructive sleep apnoea (OSA) and insomnia are the two most common sleep disorders and are frequent reasons for presentation in Australian general practice.
Objective
This article describes the development, content and suggested uses of the online sleep health primary care clinical resource, which provides general practitioners and other primary healthcare professionals with evidence-based information on the aetiology, assessment, management, referral and ongoing care for OSA and chronic insomnia.
Discussion
The Royal Australian College of General Practitioners-accepted clinical resource for the management of OSA and chronic insomnia in primary care was developed by the Australian National Centre for Sleep Health Services Research. The resource is designed to be used during consultations (eg following the steps in assessment and management and the use of online questionnaires for the assessment of OSA [Epworth Sleepiness Scale/OSA50/STOP-Bang] and insomnia [Sleep Condition Indicator/and Insomnia Severity Index]) and as an education/training tool (eg evidence on the role of continuous positive airway pressure/mandibular advancement splints for management of OSA and brief behavioural therapy for insomnia/cognitive behavioural therapy for insomnia for the management of insomnia).
Obstructive sleep apnoea (OSA) and chronic insomnia are the two most prevalent sleep disorders in the adult Australian population.1–3 Both OSA and chronic insomnia are prevalent, debilitating and costly disorders.4,5 They are each associated with increased healthcare utilisation costs and, importantly, impact negatively on people’s mental health, physical health, quality of life and normal daytime function.6 For the past six consecutive years, The Royal Australian College of General Practitioners’ (RACGP) Health of the Nation survey of general practitioners (GPs) has reported that sleep disturbances are among the most common reasons that people present for management in Australian general practice.7 These sleep disorders are a healthcare priority for primary healthcare professionals.8
OSA is often unrecognised and underdiagnosed. It is estimated that 20% of the Australian general population has at least moderate OSA.9,10 With appropriate training and specialist support, patients with uncomplicated OSA can be managed in primary care by GPs and practice or community-based nurses just as well as in specialist sleep centres.11 To assist diagnosis in the community, a rebate will now be provided for Medicare Benefit Schedule (MBS) items when patients are directly referred for a home-based or laboratory-based sleep study by their GP.3 OSA combined with significant respiratory, cardiac or psychiatric comorbidities is not suitable for management in primary care.
Chronic insomnia is a significant public health problem that is undertreated. It affects up to 15% of the adult population and at least one in 10 patients seen in general practice.12,13 Cognitive behavioural therapy for insomnia (CBTi) is the recommended first-line treatment for insomnia.14,15 Behavioural management of insomnia improves insomnia severity and sleep parameters and frequently improves symptoms and management of comorbid conditions such as depression and chronic pain.16,17 Consequently, chronic insomnia should be viewed as comorbid with other health and physical conditions, rather than a secondary symptom.
A search conducted by the authors did not identify any existing guidelines or resources that met the needs of Australian primary care practitioners. Therefore, the online sleep health primary care clinical resource was developed to provide primary care clinicians with a single, trusted resource offering evidence-based and on-demand information on the assessment, management and referral options for OSA and chronic insomnia.
Aim
One of the objectives of the Australian National Centre for Sleep Health Services Research (National Health and Medical Research Council of Australia Centres of Excellence based at Flinders University; www.ncshsr.com) was to develop a sleep health primary care clinical resource. The aim of this article is to provide an overview of the online resource, the development process, website design, intended use by primary care clinicians and future testing and development.
Sleep health clinical resource for primary care
The online resource (Figure 1) aims to provide GPs and other primary healthcare professionals involved in the care of OSA and chronic insomnia with up-to-date evidence-based information on the assessment, diagnosis, treatment and referral of OSA and chronic insomnia. Other primary healthcare professionals involved in treating these conditions include primary healthcare nurses, allied health professionals, pharmacists, psychologists and dentists. The resource is designed to be used online, and there is no hard copy version. The website is hosted and maintained by the Australasian Sleep Association (ASA). The resource has been endorsed by the RACGP and ASA, and has already been incorporated into HealthPathways by the Gold Coast Primary Health Network. Work with other HealthPathways teams and Therapeutic Guidelines is planned.
Figure 1. Homepage of the online sleep health primary care resource (www.sleepprimarycareresources.org.au).
Reproduced with permission from the Australasian Sleep Association.
Content development process
The resource received input from a multidisciplinary expert group, including practising and academic GPs, sleep physicians, psychologists, sleep researchers, the ASA, the RACGP, local practice-based research networks and HealthPathways, during several iterative stages of content development and ease-of-use website testing (Table 1).
| Table 1. Content development process of the sleep health primary care clinical resource |
| September 2019 |
- The NCSHSR members at Bond University developed an outline of the scope of the resource, including a list of headings and subheadings for input from the NCSHSR sleep health expert group
|
| December 2019 |
- An initial draft of the resource drew on publications identified in a literature search and discussion with key clinician and academic informants
- The level of evidence for treatment options for OSA was based on the GRADE systemA
|
| May 2020 |
- The initial draft was refined following review from the NCSHSR expert group
|
| June 2020 |
- The content of the resource was further informed by qualitative interviews with Australian GPs about experiences in the assessment and management of insomnia (n=8) and OSA (n=17) as part of the NCSHSR program
|
| September 2020 |
- A second round of review was provided by GPs and clinical editors of HealthPathways and local practice-based research networks in Queensland and South Australia
|
| November 2020 |
- Several GPs of GoldNet Research, a local practice-based research network in south-east Queensland, were consulted to provide further feedback on their written suggestions
|
| 2021 |
- The website was designed and tested
|
| April 2021 |
- A final draft was reviewed and approved by the ASA Education Committee and endorsed by the Board
|
| August 2022 |
- The final version of the resource obtained RACGP Accepted Clinical Resource status
|
| November 2022 |
- The resource was formally launched at GP22 in Melbourne, Victoria
|
| 2023 |
- The ASA supported ongoing maintenance, testing and further development of the resource
|
AThe Grading of Recommendations Assessment, Development and Evaluation (GRADE) evidence ratings are based on the recommendations of the Dutch Medical Specialists Federation (Federatie Medisch Specialisten; www.kennisinstituut.nl) published in Obstructief slaapapneu (OSA) bij volwassenen18 and the American Academy of Sleep Medicine’s most recent meta-analysis and GRADE assessment on the effectiveness of continuous positive airway pressure.19 The GRADE system provides a transparent approach to grading quality (or certainty) of evidence and strength of recommendations, and is now considered the standard in guideline development.
ASA, Australasian Sleep Association; GP, general practitioner; NCSHSR, National Centre for Sleep Health Services Research; OSA, obstructive sleep apnoea; RACGP, The Royal Australian College of General Practitioners. |
Website design and content
The freely accessible website (www.sleepprimarycareresources.org.au) was designed with easy and intuitive wayfinding in mind, and includes the following features:
- designed for computers, mobile devices, and tablets
- designed for real-time use in clinical consultations
- directs clinicians to as-needed information through search functions and hyperlinks
- has two sections following the same structure: one for OSA and one for chronic insomnia
- headers and footers, a comprehensive search function, explanation of abbreviations, quick links and hyperlinks within the text to facilitate ease of navigation
- background information on key topics to facilitate further education and exploration of OSA and chronic insomnia
- designed as a ‘living resource’ to be kept up to date based on new developments published in the peer-reviewed literature, without the need for extensive technical expertise.
The website is being assessed in a qualitative study with GPs, which will provide further feedback on its ease of use.
The website is designed to be used in a range of settings and the content has several layers with increasingly detailed information:
- The steps in assessment and management page for each condition (Figure 2) is a guide for use by GPs and other primary healthcare professionals during patient consultations. These steps are helpful during presenting and follow-up consultations.
- A key feature of the resource is the automated calculation of questionnaire scores for the assessment of OSA and insomnia (Figure 3). The OSA questionnaires are important in deciding whether a patient meets the MBS criteria for a home-based or laboratory-based sleep study. The advantages of a sleep study at home include increased patient comfort, shorter waiting time, a more accurate reflection of their sleep position and avoiding the use of hospital beds. In-laboratory assessment is relevant for patients with unstable cardiovascular status (eg nocturnal angina or recurring cardiogenic pulmonary oedema), hypercapnic respiratory failure, a high pretest probability of OSA and about to undergo major surgery and those with a history of significant drowsiness while driving. In addition, a level 1 sleep study has the benefits of video monitoring, which might be helpful in assessing for seizure activity or any complex movements during sleep. The questionnaires can be completed online during a consultation and the results can be printed or saved as a PDF file. The questionnaires related to OSA include the Epworth Sleepiness Scale, the OSA50 and STOP-Bang questionnaires. The questionnaires related to chronic insomnia include the Sleep Condition Indicator and the Insomnia Severity Index.
- Both OSA and chronic insomnia resources have a Summary page that condenses the key information relevant to the management of OSA and chronic insomnia in primary healthcare.
- Most of the remaining pages of the online resource contain a more in-depth overview of the literature to date (Table 2). These pages are developed as a training tool and contain the most detailed information, including Grading of Recommendations Assessment, Development and Evaluation (GRADE) levels based on the peer-reviewed literature of the efficacy of management of OSA. This includes the use of continuous positive airway pressure and mandibular advancement splints, as well as positional therapy for the management of positional OSA.
- The Resources section of the website contains links to other websites, as well as downloadable PDF files from sources including the ASA and Sleep Health Foundation.
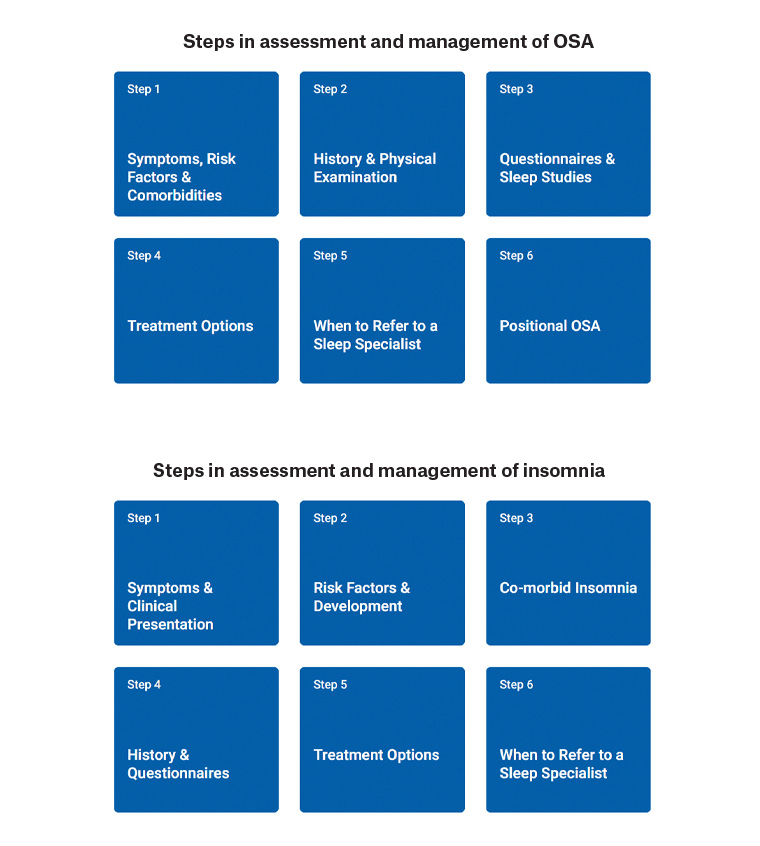
Figure 2. Steps in the assessment and management of OSA (left; www.sleepprimarycareresources.org.au/osa/steps-in-assessment-and-management) and insomnia (right; www.sleepprimarycareresources.org.au/insomnia/steps-in-assessment-and-management).
OSA, obstructive sleep apnoea.
Reproduced from Australasian Sleep Association. Obstructive sleep apnoea: Steps in assessment & management. Australasian Sleep Association, 2024. Available at www.sleepprimarycareresources.org.au/osa/steps-in-assessment-and-management [Accessed 7 May 2024]20 and Australasian Sleep Association. Chronic insomnia/insomnia disorder: Steps in assessment & management. Australasian Sleep Association, 2024. Available at www.sleepprimarycareresources.org.au/insomnia/steps-in-assessment-and-management [Accessed 7 May 2024],21 with permission from the Australasian Sleep Association.
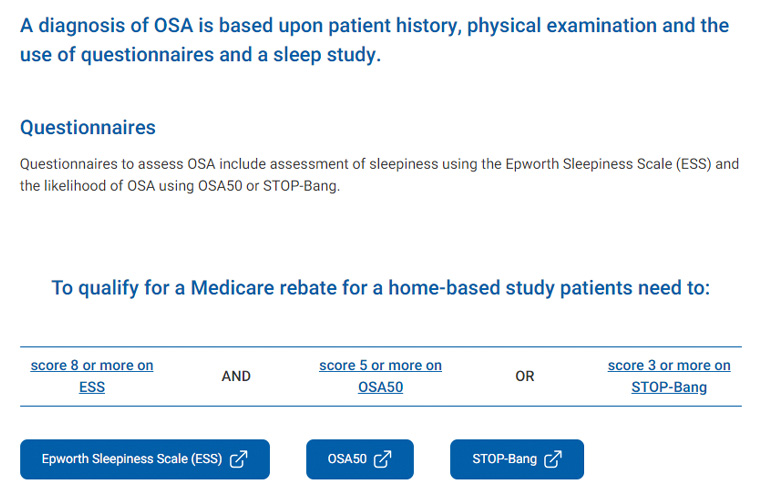
Figure 3. Steps in assessment and management: Step 3 page, questionnaires and sleep studies, of the obstructive sleep apnoea (OSA) resource (www.sleepprimarycareresources.org.au/osa/steps-in-assessment-and-management/questionnaires-and-sleep-studies).
Reproduced from Australasian Sleep Association. Obstructive sleep apnoea: Questionnaires & sleep studies. Australasian Sleep Association, 2024. Available at www.sleepprimarycareresources.org.au/osa/steps-in-assessment-and-management/questionnaires-and-sleep-studies [Accessed 7 May 2024], with permission from the Australasian Sleep Association.22
| Table 2. In-depth information about obstructive sleep apnoea and insomnia, available via the collapsible tabs found in the top banner of the resource |
| OSA resources |
Insomnia resources |
| Steps in assessment and management |
Steps in assessment and management |
| Summary and recommendations |
Summary |
| Introduction |
Acute insomnia |
| Definition |
Introduction |
| Prevalence |
Definition |
| Pathophysiology |
Prevalence |
| Comorbidities and complications |
Pathogenesis risk factors and development |
| Presentation and risk factors |
Comorbid insomnia |
| Screening |
Clinical presentation |
| Assessment – history |
Clinical presentation |
| Assessment – questionnaires |
Assessment – sleep history |
| Assessment – fitness to drive |
Assessment – questionnaires |
| Physical examination |
Management |
| Management of risk factors |
Basic sleep and sleep hygiene education |
| Sleep studies and referral |
BBTi |
| Treatment options – weight reduction |
Bedtime restriction therapy |
| Treatment options – CPAP |
Stimulus control therapy |
| Treatment options – MAS |
Relaxation techniques |
| Treatment options – positional therapy |
CBTi |
| Treatment options – surgery |
CBTi – cognitive restructuring |
| Treatment options – pharmacologic |
Referral to digital CBTi |
| Comorbid insomnia and OSA |
Referral to psychologist |
| Review CPAP adherence and follow-up |
Bright light therapy |
| |
Pharmacological therapy |
| BBTi, brief behavioural therapy for insomnia; CBTi, cognitive behavioural therapy for insomnia; CPAP, continuous positive airway pressure; MAS, mandibular advancement splint; OSA, obstructive sleep apnoea. |
Intended use by primary care clinicians
Recommendations to clinicians on how to use the website include:
- become familiar with the layout and content of the resource, including the steps in assessment and management, different sections with further information on assessment, treatment and referral recommendations, interactive questionnaires and links to other resources
- during consultations, use the resource’s interactive questionnaires to determine eligibility for a sleep study referral (eg high-risk OSA and sleepiness) or the presence of insomnia symptoms (eg Sleep Condition Indicator)
- during consultations, use the search tool to quickly find information on symptoms, treatment and resources
- outside consultations, use the resource as an education/training tool (Figure 4).
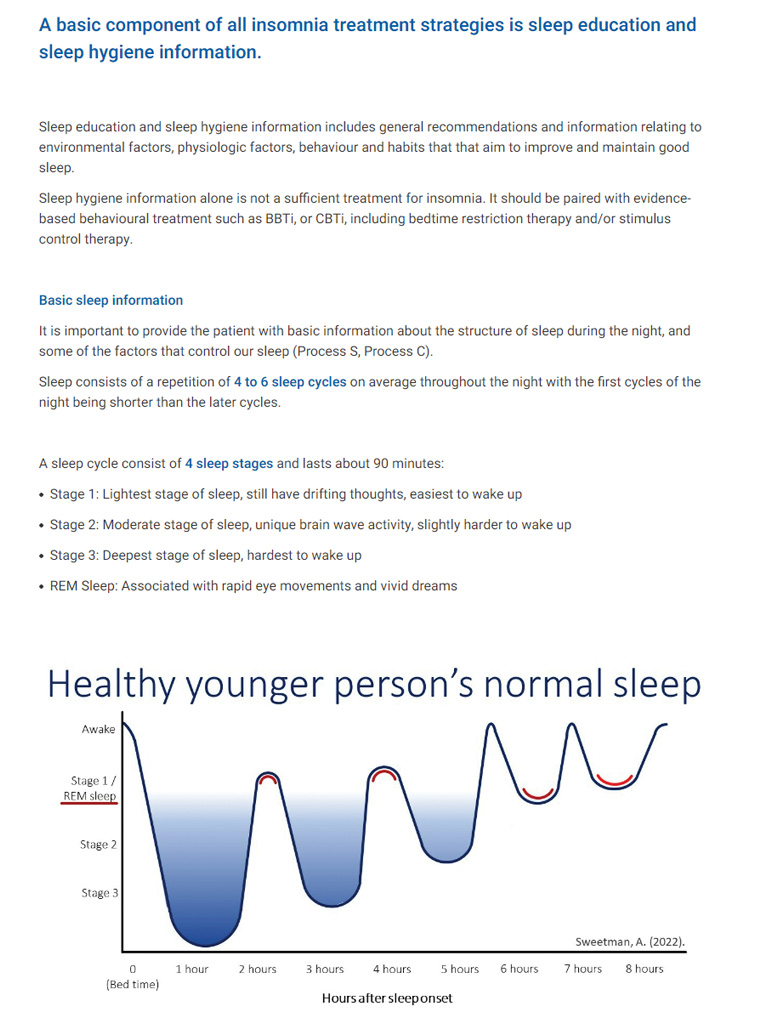
Figure 4. Screenshot of the basic sleep and sleep hygiene education section of the insomnia resource (www.sleepprimarycareresources.org.au/insomnia/basic-sleep-and-sleep-hygiene-education).
Reproduced from Australasian Sleep Association. Chronic insomnia/insomnia disorder: Basic sleep & sleep hygeine education. Australasian Sleep Association, 2024. Available at www.sleepprimarycareresources.org.au/insomnia/basic-sleep-and-sleep-hygiene-education [Accessed 7 May 2024], with permission from the Australasian Sleep Association.23
Future testing and development
The website is a living resource that will be maintained and updated as new evidence-based information, referral/treatment options and funding/reimbursement pathways for sleep disorder management become available. The ASA is refining and promoting the resource in general practice through a Health Peak and Advisory Bodies Program grant from the Commonwealth Government. The ASA is conducting a qualitative study with practising GPs to understand the scope of information in the resource and the acceptability and use of the resource as a decision support tool during consultations, as well as to generate feedback from GPs for future development. GPs and other primary care clinicians are invited to contact Alexander Sweetman (alexander.sweetman@sleep.org.au) with any feedback about the resource.
Conclusion
The National Centre for Sleep Health Services Research developed an online sleep health primary care clinical resource with up-to-date evidence-based information for the management of OSA and insomnia in primary care. The website will be kept up to date both in terms of content and ease of use by the ASA.
Key points
- The website is an RACGP-accepted clinical resource for OSA and chronic insomnia and received input from a multidisciplinary sleep expert group and practising GPs.
- The steps in assessment and management page is a guide for use during patient consultations and as a decision support tool.
- Questionnaires for the assessment of OSA (Epworth Sleepiness Scale, OSA50, STOP-Bang) and insomnia (Sleep Condition Indicator and Insomnia Severity Index) can be completed during a consultation, used to guide management, including referral, and the results can be printed or saved as a PDF file.
- A summary and a more in-depth overview of the literature provide evidence on the role of continuous positive airway pressure and mandibular advancement splints for the management of OSA, as well as brief behavioural therapy for insomnia and CBTi for the management of insomnia.