Case
A family of three individuals returning from Zimbabwe presented urgently to a rural general practice with multiple skin lesions. The man, aged 49 years, had two lesions, on the penis and groin; the woman, aged 48 years, had lesions on her left thigh (Figure 1) and her abdomen; and their daughter, aged 19 years, had one lesion on her right thigh from which she was able to extract a single larva (maggot). The daughter’s lesion improved soon after this. The lesions were all consistent in their appearance: they were red papules with a central smooth nidus and a surrounding patch of erythema (Figure 1). The family brought the extracted larva with them in a small bag (Figure 2). The lesions were worsening, with spreading erythema, pain and pruritus. The family were understandably distressed.
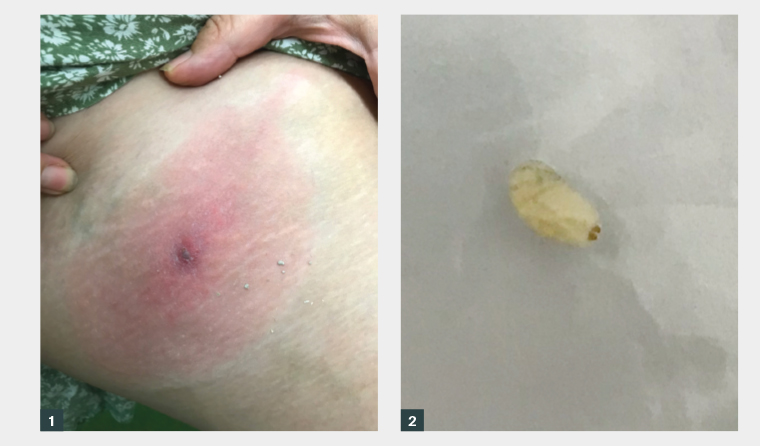
Figure 1. The thigh lesion in the woman aged 48 years.
Figure 2. The larva extracted from one of the lesions.
Question 1
What further history and examination might be important?
Question 2
What are the potential differentials in this case?
Question 3
What would be appropriate provisional treatment for these lesions?
Answer 1
It is important to obtain a thorough exposure and travel history (see Table 1).
| Table 1. Travel history |
| Theme |
Questions |
| History of presenting illness |
- Onset of symptoms
- Chronology of symptoms
- Associated symptoms
|
| Details of travel |
- Departure date
- Countries visited
- Urban/rural areas visited
- Reason for travel: tourism, visiting, humanitarian work
- Accommodation
- Return date
|
| Recreational activities |
- Activities involving fresh water
|
| Exposures |
- Bites: insects and animals
- Food
- Sources of water
- Sexual activity
- Tattoos
- Contaminated soil
|
| Precautions and vaccines |
- Insect repellent use
- Vaccinations received
prior to travel
- Malaria prophylaxis
|
Regarding examination, vital signs should be assessed for potential systemic secondary infections. If there is a systemic febrile illness with potential haemodynamic instability, then hospitalisation should be considered. Dermoscopy and a full skin examination will identify potentially unnoticed lesions in difficult areas and allow the treatment of these lesions.
Answer 2
Common differentials for such a presentation include:
- bacterial furunculosis (a deep bacterial folliculitis also known as a boil)
- insect bite reaction (a severe reaction leading to localised swelling and pruritus)
- cellulitis (a bacterial infection of the dermis and subcutaneous tissue).
When considering the clinical presentation, less common differentials include:
- cutaneous leishmaniasis (a parasitic disease that is spread by sand flies and causes skin sores)1
- tungiasis (a disease caused by female sand fleas that burrow into the skin and lay eggs, leading to abscesses)2
- cutaneous anthrax (a disease caused by contact with Bacillus anthracis spores from infected animals)3
- cutaneous myiasis (a parasitic disease caused by the invasion of fly larvae, such as Cordylobia anthropophaga or Dermatobia hominis, into the tissue of vertebrates).4
Answer 3
One of the main differentials is a bacterial furunculosis, and an antibiotic is therefore a sensible choice for provisional treatment while further information is sought. An antihistamine or topical steroid can also be commenced to assist with pruritus and inflammation.
Case continued
Further history taking reveals that the family were providing humanitarian services in Zimbabwe and were staying in urban houses with friends. They were in the country for four weeks and returned two days ago. They reported no significant exposure to fresh water, contaminated soil, insect bites or animal bites. They did not engage in any risky activities and were fully vaccinated according to the travel guidelines. They had no significant medical history, were taking no regular medications and had no allergies. Their vital signs were within normal limits.
This case was discussed with the infectious diseases team at the Canberra Hospital. The larva was sent off for identification to the local pathology provider by placing it into a specimen jar.
A shared decision was made to commence cefalexin for secondary bacterial cover given the increasing erythema and pain around the nidus of the lesion. A fatty ointment of methylprednisolone was also commenced to treat the pruritus and inflammation.
The pathology provider sent the specimen to a specialist laboratory, which provided the following detailed report:
The sample contains one-third instar (maggot) of tumbu fly, Cordylobia anthropophaga
Family – Calliphoridae, Cordylobia anthropophaga
This species of fly is found throughout Africa. The larvae of this fly burrow into human subcutaneous tissues producing boil-like lesions on almost any body part.
The diagnosis was established as furuncular myiasis secondary to tumbu larva infestation.
Question 4
How is cutaneous myiasis due to the tumbu fly transmitted?
Question 5
How is this condition definitively treated?
Question 6
How can this condition be prevented?
Answer 4
Female tumbu flies lay their eggs in soil contaminated with faeces, urine or garbage. They can also lay eggs on damp clothing that is drying, especially if it comes in contact with the ground.4
The hatched larvae can remain viable in the soil for two weeks. After the larvae penetrate the skin of a host, they develop through three larval stages. They then leave the host and bury into the ground to pupate into an adult fly, and the cycle renews.5
Transmission through the clothing seems to be the most likely method of transmission in this case given the lack of exposure to soil reported by the family. The larvae hatch when the clothes are worn and can penetrate the intact skin.4
Answer 5
The larvae mature in 8–12 weeks and then leave the tissue on their own.4 This is a suboptimal option given the risk of secondary bacterial infection and a significant granulomatous skin reaction.
Removal of the larvae would provide definitive treatment, and there are various options available, including applying lateral pressure,6 surgical removal with excision,7 more novel methods such as using a venom extractor8 or the application of a fatty ointment (eg white soft paraffin) that suffocates the larvae and forces them to exit.9 The methylprednisolone ointment in this case provided this benefit, in addition to its anti-inflammatory properties.
Answer 6
General prevention methods for cutaneous myiasis include covering the skin to limit bites and using insect repellent and mosquito nets. In this case, the most likely route of transmission was through drying clothing. To prevent this, the laundry could be protected by ironing afterwards, drying in full sunlight off the ground, drying under a mosquito net or drying in an electric dryer.4
Case continued
All the lesions were treated by the application of the fatty ointment, which suffocated the larvae, forcing them to partially exit. The larvae were then definitively removed with lateral pressure. The skin of all family members has since settled, without any ongoing issues.
Key points
- Furuncular myiasis is a condition caused by the infestation of skin by fly larvae (tumbu fly in this case) leading to boil-like lesions.
- If furuncular myiasis is suspected, the definitive treatment is removal of the larvae.
- Precautions should be taken by patients travelling to sub-Saharan Africa when drying damp clothes.