Exercise has become a central part of medicine owing to its impact on good health and the prevention and management of chronic diseases. It is therefore essential for general practitioners (GPs) to develop and maintain an understanding of how they can incorporate basic exercise prescription into their skill set and as part of their management plan. When emphasising the role of exercise in the lives of children and adolescents, it is important to first understand that children are not just ‘mini adults’, and there are unique considerations that must be applied.
This article discusses how GPs can optimise physical activity and exercise recommendations to young people, accounting for developmental, cultural and individual diversity. Although the focus of this article is on school-aged children, there is evidence to support the adoption of physical activity behaviours at younger ages. Increased levels of physical activity starting from infancy are associated with improvements in motor skill development and adiposity,1 promoting positive activity habits to continue into later childhood and adolescence.2 The current Australian recommendations, which are adapted from the Canadian Society for Exercise Physiology’s 24-Hour movement guidelines,3 for infants (birth to 12 months), toddlers (one to two years) and preschoolers (three to five years) are presented in Table 1.
| Table 1. Physical activity recommendations during infancy and early childhood from the Department of Health and Aged Care4 |
| Age group |
Recommendations |
| Infants |
- Prior to gaining mobility:
- Encourage supervised, interactive playtime on the floor
- Aim for a minimum of 30 min of active tummy time throughout the day, including movement of their limbs
- Assist them in reaching and clutching objects
- Upon achieving mobility:
- Facilitate crawling – set up simple obstacles for them to navigate
- Support them in standing up and moving around while using objects for balance
- In certain instances, they might also begin walking
|
| Toddlers |
- Aim for a minimum of 3 h of assorted physical activities daily including more vigorous types of activity. These activities can include:
- running – playing tips, ball games or races at the park
- spinning and jumping – at the park or by creating fun obstacle courses at home
- dancing
- throwing
- These activities should be spread out throughout the day, rather than done in one burst
- Remember, physical activities for toddlers should be enjoyable and stimulate curiosity and learning
|
| Preschoolers |
- The more active play preschoolers take part in, the better
- Preschoolers should be active for at least 3 h each day; this should include 1 h of energetic play, like:
- running – playing tips, ball games or races at the park
- kicking, throwing and jumping – at the park or by creating fun obstacle courses at home
- dancing
- skipping
- These activities should be spread out throughout the day, rather than done in one burst
- Remember, physical activities for preschoolers should be enjoyable and stimulate curiosity and learning
|
For children aged five years and older, the Australian exercise guidelines include at least 60 minutes of moderate to vigorous physical activity each day that can be divided into several shorter bouts throughout the day. It is recommended that on at least three days of the week, children incorporate more vigorous activities, as well as activities that contain bone- and muscle-strengthening elements. It is important that children also aim to reduce sedentary behaviours (which often includes screen time) to maintain an active and healthy lifestyle. Table 2 summarises the guidelines for children with example activities.
| Table 2. Activity recommendations for children aged 5–18 years from the Department of Health and Aged Care4 |
| Type of activity |
How much and how often? |
Examples |
| Light physical activity |
Every day for several hours |
- Walking to school
- Walking the dog
- Going to the park with friends
- Helping around the house
- Playing handball
|
| Moderate to vigorous physical activity |
Moderate activity every day for at least 60 min with 3 days incorporating vigorous activity |
- Football
- Basketball
- Netball
- Bike riding
- Scooter riding
- Swimming
- Dancing
|
| Muscle-strengthening activity |
3 days/week as part of the 60 min of daily activity |
- Running
- Climbing
- Swinging on monkey bars
- Push-ups
- Sit-ups
- Lifting weights
- Yoga
|
How much exercise are Australian children currently performing?
The 2020–21 National health survey found that only 8.9% of young people aged 15–17 years met the physical activity guidelines in Australia,5 and this was similar to the 10% reported in 2017–18,6 suggesting that COVID-19 was not a significant determinant. The most recent data in younger children are from the National nutrition and physical activity survey 2011–12, detailing that just under one-quarter (23%) of children aged 5–14 years performed the recommended 60 minutes of physical activity per day.7 Males continue to dominate participation rates in organised sport across all ages,
but a five-year study investigating community-level sport participation rates identified that this gap is gradually closing in line with strategies and investments into sport and wider cultural developments in society.8
Cohorts at increased risk of not meeting the recommended guidelines include teenage girls,9 Aboriginal and Torres Strait Islander peoples,10 people from low socioeconomic backgrounds11 and those with or at high risk of a chronic condition.12 Some of the most frequently cited obstacles to sport participation include the child’s or parents’ schedules, costs and limited access.13 Broader issues, such as the amount of physical activity children are performing while at school,14 and the impact of increased levels of screen time (both at home and at school) on numerous health indicators further influence sedentary behaviour among Australian children.15
Why is exercise important for children?
The benefits of exercise in improving physical and psychological health, and in the prevention and management of chronic diseases, are well documented. Activity levels during younger ages are associated with significant improvements in motor performance and cognitive development,16 and are highly predictive of adult activity levels.2
Aerobic exercise has been shown to considerably improve body composition outcomes in school-aged children with overweight and obesity, including significant changes in measures of body mass index, total fat and abdominal fat.17 Cardiovascular risk factors, including levels of high-density lipoprotein cholesterol and triglycerides, improve with aerobic exercise, with unfit boys and girls 1.9- to 3.7-fold more likely to have hypercholesterolaemia than their physically active counterparts.17 Metabolic syndrome and hypertension also benefit from exercise intervention. Strength training, once thought to stunt childhood growth and provide undue risk of injury, is now known to be effective at improving strength (even in prepubertal children) and bone health, likely leading to increased athletic performance and reduced injury risk during sport.18
The role of sport and exercise in improving many psychological and social health outcomes has also been investigated. There is strong evidence that participation in team sport in particular is associated with improvements beyond leisure time physical activity or individual sports.19 Engagement in regular physical activity during childhood and adolescence positively influences cognitive function, including attention, learning and memory.20
Table 3 summarises the effects of exercise on a number of physical, psychological and cognitive variables.
| Table 3. Health measures that strongly benefit from exercise |
| Health measure |
SampleA |
Minimum amount of physical activity for health benefit |
| Adiposity |
Overweight or obese |
F: 3–5 days/week
I: Moderate to vigorous
D: 30–40 min/day
T: Variety of aerobic activities |
| Cardiovascular health |
| Metabolic syndrome |
Overweight or obese |
Likely similar to adiposity |
| Lipids/lipoproteins |
|
|
| HDL-C |
|
Likely similar to adiposity |
| Triglycerides |
|
Likely similar to adiposity |
| Blood pressure |
Hypertensive |
F: 3 days/week
I: Vigorous
D: 30 min/session
T: Aerobic |
| Mental health |
| Anxiety symptoms |
|
Varies with mode of activity |
| Depression symptoms |
|
Varies with mode of activity |
| Academic performance |
| Grades, standardised tests |
|
Unclear |
| Indicators (eg memory) |
|
Unclear |
| Bone strength |
Prepubertal and pubertal |
F: 2–3+ times/week
I: Moderate–high strain
D: 10–60 min
T: 10 min impact-loading exercise (eg skipping, running or jumping), 45–60 min general weight bearing |
Adapted from Janssen and LeBlanc (2010).17
AUnless indicated otherwise, all samples are from the general child and youth population.
D, duration; F, frequency; HDL-C, high-density lipoprotein cholesterol; I, intensity; T, type of activity. |
Assessing activity levels
The Royal Australian College of General Practitioners (RACGP) recommends that physical activity is assessed opportunistically in children and adolescents.21 Australian GPs, often heavily limited by time, report challenges following this recommendation and are therefore more likely to enquire when physical activity is ‘immediately relevant’ to a patient’s presentation.22 Assessing whether a child or adolescent is achieving the desired level of exercise can be difficult and should ideally factor in sports participation, both organised and unorganised, recreational activities, incidental physical activity and sedentary behaviours. A full assessment incorporating the principles of frequency, intensity, type and duration of activity is beneficial, but GPs report lack of time as the greatest barrier to achieving this appraisal.22 Investigations of the utility of a brief, two-question physical activity assessment compared with objective assessment using accelerometry and more detailed self-report measures have shown good validity and reliability in adults.23 Although this has not yet been assessed in children, adapting the questions to adhere to child and adolescent guidelines might assist with a clearer determination of activity levels; for example:
- On average, how many days per week does the child engage in at least 60 minutes of vigorous physical activity (eg playing sport, heavy lifting or fast bicycling)?
- On average, how many days per week doesthe child engage in at least 60 minutes of moderate physical activity (eg walking while carrying a backpack, bicycling at a regular pace or playing more leisurely games)?
Children and adolescents may also use activity-monitoring devices, such as smart watches or mobile apps, that provide additional data, such as step counts and heart rate, and can be a useful adjunct to further elucidate their levels of activity.
An exercise assessment is a reliable way to gauge cardiorespiratory fitness, physical conditioning and functional status. Time and equipment constraints make formal cardiopulmonary exercise testing unfeasible in most general practice settings; therefore, referral to specialised services might be indicated if such testing is required. Routine monitoring of other related health markers, such as body mass index and waist circumference, should also be used to complement activity level assessment.
Prescribing exercise
It is important to highlight that any physical activity is better than none. Patients not exercising regularly should be encouraged to start smaller bouts of exercise, with the aim of gradually building by 5–10% each week towards the recommended amount.21 Children are generally encouraged to sample a range of different sports and activities, while specialisation should be delayed until late adolescence (age 13–15 years) to optimise success while minimising injury, psychological stress and burnout.24 Regarding weight training, in general, children and adolescents should use submaximal loads and be of sufficient age and maturity to follow instructions correctly.18 Special mention should also be made with regard to children exercising in hot environments. Due to a higher ratio between surface area and body mass leading to a more rapid increase in body temperature alongside an underdeveloped sweating mechanism impacting body cooling, children and adolescents have increased vulnerability to thermal injury.25 It is therefore recommended that stricter control of fluid intake and monitoring of temperature and weather conditions be given extra attention.25
Cultural considerations that affect how children and adolescents meet sport and exercise guidelines are another important factor. Examples include:
- family support and engagement
- religious beliefs and practices (eg sporting attire, fasting periods)
- gender norms and expectations, including cultural sensitivities to mixed gender participation
- language and communication.
These should be discussed prior to the delivery of an exercise program to promote an inclusive and culturally sensitive environment. Figure 1 is an example of a form that can be used to quickly assess sedentary behaviour and activity levels, as well as providing goals and an exercise prescription.
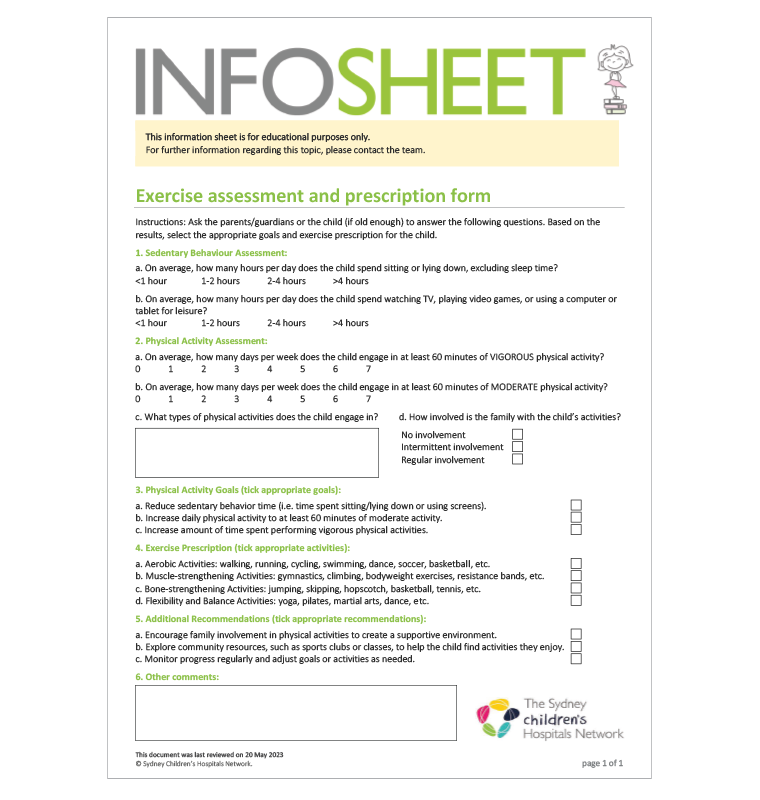
Figure 1. An example of a paediatric exercise assessment and prescription form (Sydney Children’s Hospitals Network; SCHN).26
Reproduced with permission from the Children’s Hospital Institute of Sports Medicine.
Exercise in special populations
Although the Australian physical activity guidelines outline an ideal framework for children to follow, many patients will face additional challenges that might require a nuanced approach to exercise and activity prescription. The Australian Government does not provide specific guidelines for children with disabilities and chronic conditions due to the individual nature of these issues.4
Children and adolescents with chronic conditions and disabilities have distinct requirements, sometimes precluding generalised activity guidance. These might include:
- mobility limitations
- sensory impairments
- cognitive and learning disability
- chronic health conditions (eg obesity, asthma)
- mental health challenges.
In many situations where one or more of these issues are present, a more tailored approach might be required in order to ensure the exercise performed is not counter to medical recommendations, is inclusive and takes into consideration additional needs, such as assistive devices/equipment. A collaborative approach with appropriate medical specialities and allied health professionals, such as an exercise physiologist, is therefore essential to develop an optimal exercise management plan individualised to the child’s or adolescent’s needs and goals. Exercise and Sport Science Australia (ESSA) has developed Exercise for disabilities,27 an e-book that outlines the fundamentals for exercise prescription in many conditions, including cerebral palsy, autism and sensory impairments.
Exercise dosage suggestions for paediatric chronic diseases, including cystic fibrosis, asthma, congenital heart disease, obesity, type 2 diabetes, juvenile idiopathic arthritis (JIA) and cancer, have been published previously.12 Specific conditions might carry inherent risks that curtail the prescription of unrestricted activity, and it is therefore important to be aware of some of the necessary limitations. It is recommended that children and adolescents with cardiomyopathy, isolated pulmonary hypertension and Marfan syndrome with aortic dilation avoid strength training, and that those with seizure disorders first demonstrate good seizure control before participation.18 Other recommendations and contraindications for JIA, osteogenesis imperfecta, achondroplasia, haemophilia, cerebral palsy, spina bifida, cystic fibrosis and childhood cancer are also available.28
Once these aspects have been appropriately factored in and there is an indication to promote additional exercise, the RACGP suggests the following interventions:
- at least two sessions of face-to-face provision of brief advice or counselling on exercise with supporting written materials
- written prescription for exercise and/or supplementary advice or counselling by telephone
- consideration of referral to structured physical activity programs such as the Better Health Program (Western Australia) or Go 4 Fun (New South Wales [NSW]), which provide 10-week programs for children aged 7–13 years who are above a healthy weight.21
When to refer for specialist evaluation
Referral to hospital or paediatric services might be considered for children and adolescents if they are aged 2–18 years and have a body mass index well above the 95th percentile on the US Centers for Disease Control and Prevention (CDC) growth charts or the 97th percentile on World Health Organization growth charts, or if they have serious related comorbidities that require weight management (eg sleep apnoea, orthopaedic problems, risk factors for cardiovascular disease or type 2 diabetes, psychological distress).21 Paediatric sport and exercise medicine services such as the Children’s Hospital Institute of Sports Medicine (Westmead, NSW) might also be considered for more objective exercise assessment and specialised exercise prescription. Numerous organisations are available to assist with meeting the distinct needs of children and adolescents, including those with chronic diseases and disabilities (Table 4).
Conclusion
The prescription of exercise for children and adolescents serves as a powerful tool for GPs to promote overall health and wellbeing. By integrating physical activity into the lives of children and adolescents, GPs can assist the growth and development of young people and reduce the risk of chronic disease while improving social skills, cognitive development and mental wellbeing. It is vital for GPs to remain current with the latest recommendations and resources to ensure they provide optimal care for their young patients.