Case
A man, aged 39 years, presented to a rural hospital with frequent watery bowel motions. The patient described a two-day history of 15–20 bowel actions daily with overnight faecal incontinence. He had arrived two days ago from interstate for a new job and was staying at a hotel close to the hospital. Other symptoms were fatigue, nausea, abdominal discomfort, reduced urination and perianal irritation. He had not travelled outside Australia in the preceding year. He was tolerating water and black tea. He had taken eight 2 mg loperamide tablets the day prior to presentation, with no change in symptoms. On examination, he was afebrile, with a pulse of 95 and blood pressure of 120/70 mmHg supine and 105/70 mmHg standing. Abdominal examination was notable for several laparoscopy scars. The patient reported that these were from colectomy surgery for ulcerative colitis (UC) five years previously.
Question 1
Why has this man had a colectomy?
Question 2
What are the implications of his surgery on this presentation?
Answer 1
Ulcerative colitis (UC) might be severe despite treatment, with persistent bleeding, toxic megacolon or perforation requiring surgery. One in 10 patients with UC will require surgery 10 years after diagnosis.1 The most common procedure is proctocolectomy with ileal pouch anal anastomosis (Figure 1).2 UC incidence in Australia rose through the 20th century and is now stable. Its prevalence is rising due to near normal life expectancy of patients with UC.3
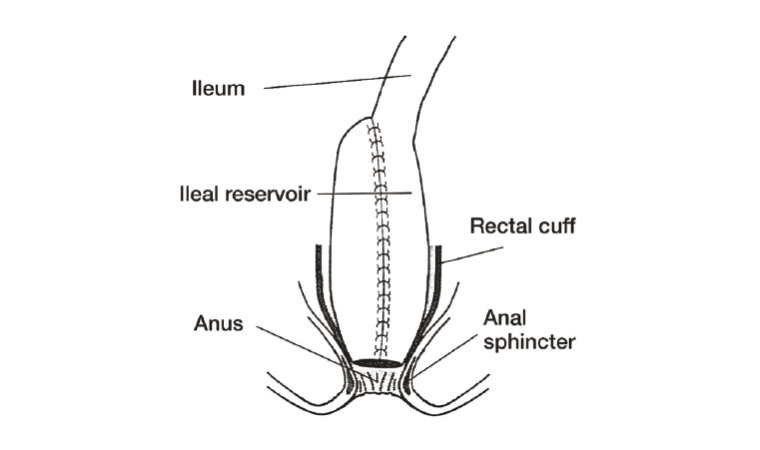
Figure 1. Anatomy after proctocolectomy and ileal J-pouch anal anastomosis.
Reproduced with permission from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health (www.niddk.nih.gov/news/media-library/17891).
Other reasons for total colectomy are familial adenomatous polyposis and Hirschsprung’s disease.
Answer 2
In the intact state, the colon reabsorbs 400 to 1000 mL of water per day, with capacity to absorb much more.4,5 People with a total colectomy have increased stool volume, with an average of six bowel actions in 24 hours, including one overnight.6 Patients who have had a total colectomy have a reduced capacity to cope with increased ileal flow, and they are prone to dehydration and electrolyte loss.
Case continued
The patient was advised to temporarily take loperamide at an increased dose of 6 mg four times a day and commence oral rehydration solution rather than water.7 He was reviewed after four hours. He had two bowel actions in four hours and was feeling better and passing urine. He had discovered that his toddler niece, who he had seen the day of his departure, had come down with viral gastroenteritis. Samples were arranged for stool culture and he was discharged. He was seen later in the week; stool cultures and polymerase chain reaction results were negative for known pathogens. At this stage, he had eight bowel actions per day and could return to work.
Question 3
What are the other potential causes of diarrhoea in this case?
Question 4
What are the other complications of total colectomy?
Answer 3
Pouchitis is an inflammatory or infective condition of the ileal pouch. It is a common complication of colectomy surgery. Antibiotics might be required, and it should be treated in conjunction with a gastroenterologist or colorectal surgeon. Patients with a pouch might manage their bowel actions with a particular diet, and the patient in this case study might have had difficulty with this while travelling, further contributing to his condition.
Answer 4
Seepage of bowel contents, abdominal pain, perianal pain and irritation, and bowel obstruction are other common gut side effects of total colectomy surgery. Despite these complications, most patients report improved quality of life postsurgery, and almost 90% of patients would recommend the surgery to another individual in a similar situation.8
Case continued
The patient is staying in the town for work and continues to see his general practitioner (GP). Shared care has been established with his original surgeon and gastroenterologist.
Question 5
What other issues should the doctor address with the patient?
Answer 5
Other issues experienced by patients with ileal pouches include sleep disturbance and low energy due to nocturnal bowel actions, incontinence and ‘toilet awareness’, altered sexual and reproductive function, and body image concerns. Patients have reported feeling ‘forgotten after being cured’.8 Validating patients’ concerns and connecting them with appropriate allied health practitioners and support groups is useful.9
Key points
- Proctocolectomy with ileoanal anastomosis is required for severe UC refractory to treatment. As patients with UC have near normal life expectancy, the prevalence of this condition will likely rise.
- Familiarity with expected complications and understanding what is normal for individual patients is essential for the treating GP. Relationships with treating specialists in gastroenterology and colorectal surgery are essential to manage complications.
- Ileoanal anastomosis surgery affects all aspects of the patient’s life. Treating practitioners should actively enquire about complications. Support through organisations such as Crohn’s & Colitis Australia is useful.