Case
A previously well male surveyor, aged 53 years, presented for dermatologist review for an eight-week history of a widespread pruritic eruption. The itch initially affected his wrists, palms and ankles and became more widespread after four weeks, involving all areas of his body from the neck down, affecting his sleep and ability to function. There were no recent changes to his regular medications, which included longstanding rosuvastatin and escitalopram.
Complete skin examination demonstrated erythematous and excoriated papules over his trunk and the webbing of his fingers and feet. Firm pruritic genital nodules were present. Serpiginous epidermal burrows were visible on dermoscopy on his wrist (Figure 1).
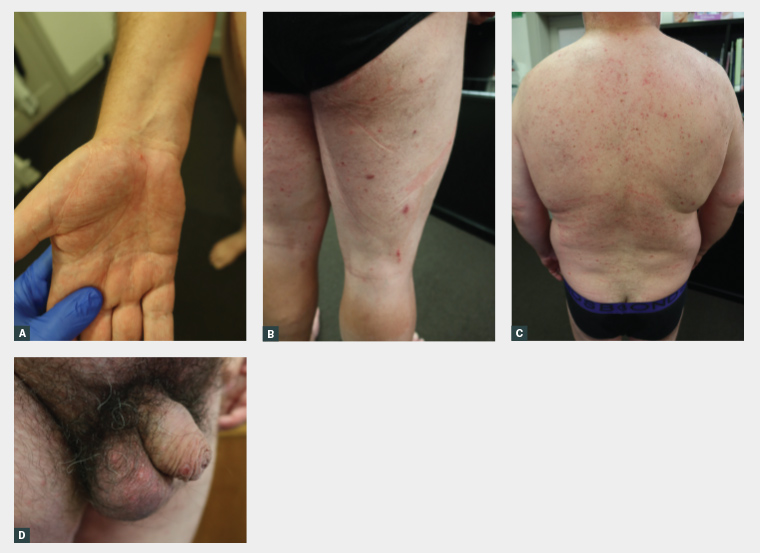
Figure 1. Representative clinical photographs demonstrating scattered erythematous papules, nodules and burrows of (A) the right volar wrist, (B) lower limbs, (C) back and (D) genitals.
Question 1
What is the most likely diagnosis?
Question 2
What are the potential differential diagnoses for this condition?
Question 3
How is scabies treated?
Question 4
What are some general management considerations?
Answer 1
Scabies is a cutaneous infectious dermatosis caused by the obligate human parasite Sarcoptes scabiei var. hominis. Adult female mites dig tunnel-like burrows within the epidermis and lay two to three eggs daily.1 An infected adult can be infested with up to 15 mites. Each mite can produce up to 40 ova, and larvae hatch after two to four days.2 Infestation triggers symptoms of generalised itching within three to six weeks, with a characteristic nocturnal predominance, the clinical hallmark of scabies.3
Scabies is an under-appreciated global health concern, affecting 300 million individuals annually.2 It is highly contagious. In Australia, scabies clusters in overcrowded environments that facilitate its spread. It can be found in remote Aboriginal and Torres Strait Islander communities and institutions such as prisons or aged-care facilities, although numerous sporadic cases are identified in the mainstream community.
Immunocompromised patients are at risk of crusted scabies, which occurs as a result of hyperinfestation with millions of mites, permitting rapid transmission between individuals.3 Crusted scabies is associated with a five-year mortality of 50% due to secondary sepsis and/or the underlying predisposing condition.4
Infestation with scabies can trigger a hypersensitivity response to burrowing mites and their faeces and result in secondary eczema, which contributes to the symptoms of intractable itch.5
Scabietic lesions can become coinfected with skin commensals such as Streptococcus pyogenes and Staphylococcus aureus due to excoriation or skin breaches by burrows leading to superinfection. Aside from local skin infections such as impetigo, these infections can lead to significant morbidity due to their associated postinfectious sequelae, including acute rheumatic fever and post-streptococcal glomerulonephritis.6
Answer 2
The differential diagnosis of scabies can include insect bites, atopic dermatitis, papular urticaria, folliculitis, prurigo and bullous skin diseases such as dermatitis herpetiformis. Crusted scabies may mimic seborrhoeic dermatitis or chronic plaque psoriasis.
Scabies is generally a clinical diagnosis. Patients tend to report a history of intractable itch that is worse at night and associated history of itch in close contacts. It has a predilection for intertriginous spaces, particularly the dorsal interdigital web spaces of the hands, axillae, buttocks, genitalia and under the breasts in women, although the limbs and trunk can be involved. It can present as erythematous papules on palms or soles, or as firm pruritic nodules in the genitalia that can be pathognomonic of scabies.
The use of dermoscopy can reveal serpiginous burrows with the triangular or ‘delta’ sign indicative of the mite’s head (Figure 2).7 Translucent ovoid eggs evidenced by ‘mini triangular signs’ may be visualised under dermoscopy.7 Direct visualisation of a fresh skin scraping with 10% potassium hydroxide under light microscopy demonstrating a live mite or ova can corroborate the diagnosis, although this can be impractical in resource-poor settings.

Figure 2. Dermoscopy of the volar wrist burrow demonstrating a serpiginous burrow with the ‘delta sign’ (arrow).
Answer 3
First-line treatment is 5% topical permethrin covering all areas of the body, including skin creases, from the jawline to toes, left on overnight for a minimum period of eight hours. Asymptomatic close contacts, including family members, should be treated simultaneously to avoid reinfestation. Repeat application is essential after seven days to eradicate newly hatched mites.
Oral ivermectin is a highly effective option in cases where treatment with topical permethrin has failed or when there is an inability to comply with topical therapy. Oral ivermectin is used at a dose of 200 mcg/kg and prescribed as a single dose that is repeated between seven and 14 days. Ivermectin is the treatment of choice to eradicate crusted scabies or mass outbreaks, but it is not recommended for use in pregnant or breastfeeding women or in children aged less than five years or weighing less than 15 kg.6
Other less effective treatments include benzyl benzoate, which has reduced tolerability and efficacy compared with permethrin.6
Answer 4
General measures to assist with itch control include avoiding irritants, the use of soap alternatives, emollients and antihistamines and the application of a medium-potency topical steroid until the itch subsides, because post-scabetic itch due to secondary eczema may persist for weeks after the treatment is completed.
Mellanby demonstrated that scabies is likely spread through direct person-to-person or sexual contact as opposed to fomites.8 However, guidelines continue to recommend environmental control measures because live mites have been identified in the surroundings of patients with crusted scabies in particular.9 Recommendations include hot laundering of linen and bagging non-cleanable items such as pillows for 72 hours, the expected lifetime of a scabies mite without a host for survival.10
Key points
- Scabies is caused by the obligate human parasite Sarcoptes scabiei var. hominis and is transmitted via person-to-person contact.
- Scabies outbreaks tend to occur in communities where there is overcrowding; however, scabies needs to be considered in the differential of any pruritic cutaneous dermatoses.
- First-line treatment for scabies is topical permethrin 5%, and close contacts should be treated simultaneously. Oral ivermectin is effective in those who have not responded to topical treatment.