Case
A man, aged 60 years, presented with a sudden onset of erythema, oedema and significant inflammation with non-scaly and relatively well-demarcated erythematous plaques, pustules and large nodules on his cheeks, with small abscess formation and significant pus discharge more prominent on the right medial cheek (Figure 1). There was no preceding factor to account for the presentation. The man was otherwise well, with no systemic symptoms such as fever, sweating, weight loss or being unwell. He denied any history of trauma or injury to his skin.
He had a history of acne as a teenager and his past medical history otherwise included hypercholesterolaemia managed with diet and lifestyle.
On examination, he had moderate-to- severely inflamed and oedematous skin on bilateral cheeks and chin, and moderate rhinophyma.

Figure 1. Sudden onset of papules, nodules and pustules on the central face of a man aged 60 years.
Question 1
What are the differential diagnoses and what initial investigations should be performed?
Answer 1
The acute onset of the facial eruptions can represent an infection (bacterial, fungal or viral), an inflammatory process (eg acne, rosacea, dermatitis, cutaneous lupus) or skin malignancies.
Initial investigations include microscopy and culture examination of the swab taken from the discharge, systemic inflammation response check and a skin biopsy for histopathological assessment.
Case continued
The skin swab for microscopic examination and culture did not reveal any microorganism. Biochemistry was unremarkable, with no leucocytosis or elevations in C-reactive protein or the erythrocyte sedimentation rate. Histopathology of the facial lesion reported mild spongiosis but an otherwise normal epidermis. There were telangiectatic vessels in the upper dermis with perivascular lymphoplasmacytic inflammation. The overall features on histology were suggestive of rosacea (Figure 2).
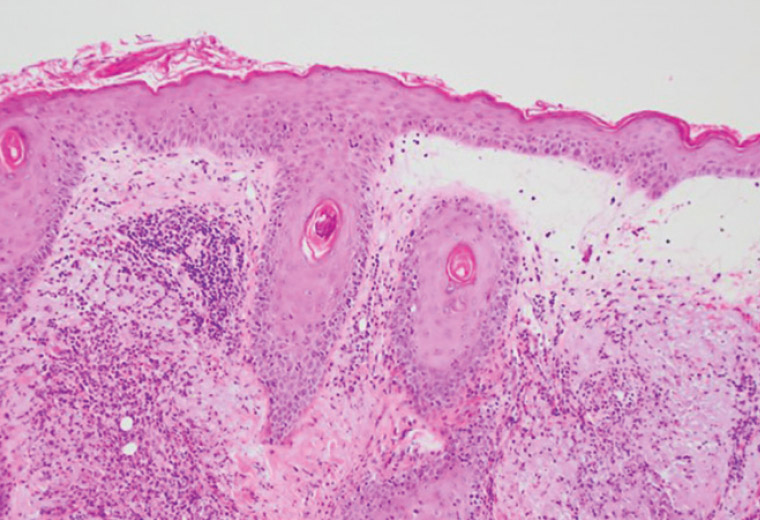
Figure 2. Histological examination of a skin biopsy of papules that appeared acutely on the central face of a man aged 60 years showing telangiectatic vessels and perivascular inflammation, diagnostic for rosacea (haematoxylin and eosin stain; original magnification ×100).
Question 2
What was the final diagnosis?
Answer 2
The patient was clinically diagnosed with rosacea fulminans (pyoderma faciale), an acute form of rosacea. Although he had a history of acne as a teenager, it is not common for acne vulgaris to represent with significant papule, nodules and cysts over a short period of time after being inactive for years.
Although pyoderma faciale can represent as acne and rosacea, it was believed to be a form of acne conglobata1 when described by O’Leary and Kierland in 1940. It was first described as a severe and extreme version of rosacea in 1992.2
The aetiology of the condition is not fully understood. It seems to be different from acne with the absence of comedones and the disease onset being after adolescence.
Question 3
How is rosacea fulminans diagnosed?
Question 4
Who gets rosacea fulminans?
Question 5
What are the possible associations with other medical conditions?
Question 6
What are the treatment options?
Answer 3
The diagnosis of rosacea fulminans is often made clinically. Bacterial culture from the purulent lesions is typically negative. A microbiological swab is often considered following a poor response to an initial course of antibiotics to exclude atypical infections or antibiotic resistance. Histological examination can sometimes help with the diagnosis by revealing periadnexal and perivascular neutrophilic, lymphocytic and histiocytic infiltrates. Rosacea fulminans does not present with any systemic symptoms.3
Skin biopsy is often considered to identify the nature of the inflammatory response, including polymorphic light eruptions, drug-related rash, granulomatous conditions, cutaneous lupus and skin malignancies like mycosis fungicides.
Answer 4
This form of rosacea more commonly affects women. The predominance of the condition in women and reports of disease onset in pregnancy4 suggest a possible role of hormones as a contributing factor.
Although the common presentation of the condition is severe inflammatory papules, pustules, necrotic cysts and nodules on the face of middle-aged women, it has also been reported to have some extrafacial presentations and can be seen in other age groups.5,6
Answer 5
The disease has been reported in association with inflammatory bowel disease,7 thyroid disease,8 psychological and emotional stress9 and some medications, such as high doses vitamins B6 and B12, PEGylated interferon and ribavirin.10–12
Answer 6
Numerous treatments have been suggested for pyoderma faciale, including oral antibiotics, corticosteroids and isotretinoin.13
Further treatments of rosacea with oral isotretinoin, vascular laser for telangiectatic components and ablative laser for rhinophyma can be considered.
Case continued
Before being referred to the dermatology clinic, the patient had a course of cephalexin 500 mg four times daily for 10 days. Following the review in the dermatology clinic, in consultation with the dermatologist, he was started on doxycycline 100 mg daily and prednisolone 25 mg daily. After a week, his doxycycline was changed to isotretinoin 20 mg on alternate days for two weeks followed by 20 mg daily afterward, and prednisolone was also continued with 25 mg daily for another two weeks before it was reduced to 12.5 mg daily for a week and then 12.5 mg on alternate days for a week before medication was stopped.
Question 7
What was the outlook of the treatment?
Answer 7
Two months into the treatment with isotretinoin 20 mg/day, the patient presented with a significant improvement in skin inflammation and erythema on his cheeks. He was able to reduce the dose of isotretinoin to 20 mg on alternate days for a further five months.
He tolerated the treatment well and the periodic blood test did not reveal any metabolic complication of the therapy. The treatment resulted in an almost complete recovery of the skin with no scars (Figure 3).

Figure 3. Almost complete clearance of rosacea fulminans 6 months into the treatment with oral isotretinoin.
Key points
- Acute onset of facial eruption could be caused by infectious or non-infectious aetiologies.
- The acute form of rosacea, so-called rosacea fulminans, can represent with papules, pustules and nodules with significant inflammatory components.
- Oral isotretinoin is the first-line treatment, which warrants early referral to a dermatologist to prevent scarring.