Low back pain (LBP) is the second most common cause for seeking help from general practitioners (GPs).1 With one in six Australians reporting back pain,2 it is the leading cause of disability burden in Australia3 and the main reason for lost work productivity and lost work years due to premature retirement.4,5
People with acute LBP worry that pain means damage, about the effects of their injury on their work and daily life and whether they will recover.6,7 These consultations can be challenging for GPs to manage within tight time frames; however, it is important to effectively assess each patient and address any misconceptions about natural history and approaches to investigations and management from the outset.
Although there is evidence as to how LBP should be managed, naturally GPs vary in their expertise and experience and there is evidence that initial management of LBP could be improved.8–10 There is underuse of low-cost and effective approaches, such as education, advice to remain active and choosing non-drug therapies as first choice, whereas the inappropriate use of imaging and the prescribing of opioids and other medications to manage pain are more common. Research finds that underuse of appropriate care and overuse of low-value care (eg imaging) are actually associated with worse health and return-to-work outcomes for patients with LBP.11–13
Aim
This paper explores the Low Back Pain Clinical Care Standard14 (the Standard) developed by the Australian Commission on Safety and Quality in Health Care in response to the identified gap between best and actual practice. We use a brief case study to illustrate key management steps outlined in the Standard, focusing on areas where the need for quality improvement is greatest.
Figure 1 outlines the extensive process undertaken in the Standard’s development. Eight quality statements are addressed in detail in the Standard and are used to structure this paper. Sections most relevant to GPs have been summarised in a practical guide, with evidence summaries, clinical tips and suggested ways to communicate challenging concepts. Box 1 has links to this GP guide, as well as to many resources for clinicians and patients to assist in shared decision making.
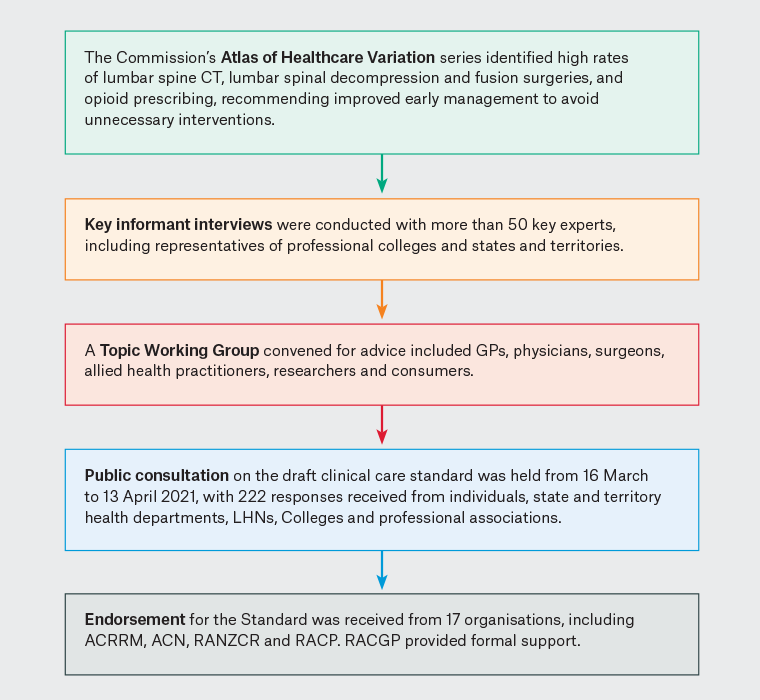
Figure 1. Development process for the Low Back Pain Clinical Care Standard14 by the Australian Commission on Safety and Quality in Health Care (the Commission).
ACN, Australian College of Nursing; ACRRM, Australian College of Rural and Remote Medicine; CT, computed tomography; GPs, general practitioners; LHNs, local health networks; RACGP, The Royal Australian College of General Practitioners; RACP, Royal Australasian College of Physicians; RANZCR, Royal Australian and New Zealand College of Radiologists.
| Box 1. Useful resources |
| For clinicians
For patients
|
The Low Back Pain Clinical Care Standard
We highlight useful evidence, concepts and practical management advice of the Standard, using an abbreviated case study of a patient named John:
John, aged 40 years, is a self-employed plumber who presents with a recurrent episode of LBP that began slowly while digging a trench. He has constant ache over his lower lumbar regions and buttocks, rated at 5/10, becoming sharp and 8/10 with movements such as bending. Hot packs and ibuprofen give partial relief. John mentions that his apprentice hurt his back last year and was never able to return to work. John reports that two similar episodes of LBP in recent years both lasted three days. This episode is worse.
John is worried about his ability to continue working and, among other things, asks if it is time to do a scan.
Conduct an initial clinical assessment
Patients need to be assessed early in each new presentation of LBP, with targeted history and examination to exclude serious pathology and differential diagnoses. A focused neurological examination is necessary when the back pain is accompanied by leg pain and/or neurological symptoms.
After a targeted history and examination, you decide John is experiencing another episode of non-specific LBP with no suspicious features.
Here is a communication tip from the Standard to inform John:
We’ve done a good assessment here today and there is no indication that your back pain is associated with a serious underlying condition. While the pain can be severe, the good news is that most acute episodes of LBP settle within a couple of weeks. In the meantime, there are a lot of things you can do to help reduce and manage your LBP.14
Psychosocial assessment
John still looks worried. He is concerned any activity that hurts him now is further damaging his back.
Some psychosocial factors and emotional responses to pain are linked to delayed recovery from back pain. Identifying these risk factors is often overlooked in practice. GPs can use a biopsychosocial approach in the history and/or brief online risk assessment tools to find patients at such risk. Actively listen to the patient and identify harmful misconceptions, including fear avoidance (Box 2).
| Box 2. Useful questions to identify psychosocial issues |
|
Do you think your pain will improve or become worse?
- What to listen for: a belief that the back pain is damaging or potentially severely disabling
Do you think you would benefit from activity, movement or exercise?
- What to listen for: fear and avoidance of activity or movement-related pain
How are you coping emotionally with your back pain?
- What to listen for: signs of low mood, distress or withdrawal from social interaction
What treatments or activities do you think will help you recover?
- What to listen for: expectations of passive treatment, rather than expectations that active participation will help
Are you worried that something has been missed?
- What to listen for: concerns that there is serious pathology that has been missed.
|
| Adapted from Health Quality Ontario. Quality standards. Low back pain. Care for adults with acute low back pain. Health Quality Ontario, 2019, with permission from Health Quality Ontario.16 |
You enquire further about his concerns and John confides that he is ‘worried sick’ about his business, his poor sleep and his relationship with his wife. Acknowledging his fears and that his pain is real, you provide reassurance about the nature of his pain.
Communication tip:
Back pain does not usually mean your back is badly damaged. The brain acts as an amplifier: the more you worry and think about your pain, the worse it can get.14
Given the psychosocial factors John has described, you suggest further follow up.
Reserve imaging for suspected serious pathology
John again requests at least an X-ray if not magnetic resonance imaging ‘just in case’.
Investigations are rarely indicated for non-specific LBP. Inappropriate imaging can create unnecessary concerns, and incidental findings with no clinical significance can lead to further unnecessary tests (Table 1). Radicular leg pain alone is not considered a serious pathology in the absence of severe or progressive neurological deficits.18 Although imaging can sometimes identify the cause of neuropathic pain, it should only be done if it will change management.19
| Table 1. Age-specific prevalence estimates (%) of degenerative spine imaging findings in patients asymptomatic for low back pain |
| Imaging finding |
Age group (years) |
| 20 |
30 |
40 |
50 |
60 |
70 |
80 |
| Disc degeneration |
37 |
52 |
68 |
80 |
88 |
93 |
96 |
| Disc signal loss |
17 |
33 |
54 |
73 |
86 |
94 |
97 |
| Disc height loss |
24 |
34 |
45 |
56 |
67 |
76 |
84 |
| Disc bulge |
30 |
40 |
50 |
60 |
69 |
77 |
84 |
| Disc protrusion |
29 |
31 |
33 |
36 |
38 |
40 |
43 |
| Annular fissure |
19 |
20 |
22 |
23 |
25 |
27 |
29 |
| Facet degeneration |
4 |
9 |
18 |
32 |
50 |
69 |
83 |
| Spondylolisthesis |
3 |
5 |
8 |
14 |
23 |
35 |
50 |
Prevalence rates are estimated with a generalised linear mixed-effects model for the age-specific prevalence estimate (binomial outcome) clustering on study and adjusting for the midpoint of each reported age interval of the study.
Reproduced from Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol 2015;36(4):811–16. doi: 10.3174%2Fajnr.A4173, with permission from the American Society of Neuroradiology.17 |
Communication tip:
Imaging is used mainly to rule out anything serious, but otherwise it is not very good for identifying the cause of your pain. I’m not concerned that you have a serious cause of LBP, so there is no need for any scans at this stage. In fact, imaging shows up changes that occur normally with age, even in people without back pain, so the findings are often not very helpful.14
Education and advice
The key issues are to reassure patients about the benign nature of LBP, the low risk of serious underlying disease and the likelihood of recurrence.20 Many educational materials are available to reinforce key messages (Box 1).18,19,21 It is important to address any unhelpful beliefs and thoughts identified in the psychosocial assessment that might affect how the patient manages their symptoms, including anxiety or fear about their condition.16,18,19 Explain the evidence for treatment options so the patient can understand why some strategies are, or are not, being recommended.19
Communication tip:
Most back pain is caused by a simple strain of the back, and for most people it does not indicate serious disease or long-term disability. Most people with acute LBP will feel much better or will have recovered within two weeks, if they follow some simple advice.14
Encourage self-management and physical activity
John explains that he is scared to keep working but cannot afford to rest his back as friends are advising him to do.
It is important to actively involve patients in the management of their pain and encourage self-confidence to stay active, avoid bed rest and continue or quickly return to usual activities, including work.9
Communication tip:
Pain does not mean serious damage. Remember that your back is strong. Movements might be painful at first, like an ankle sprain, but they will get better as you gradually get active again. It is likely that you will experience some pain with activity, but that does not mean that your back is getting worse or that your spine is damaged.14,18
Offer physical and/or psychological interventions
Offer the patient physical and/or psychological interventions, using their clinical and psychosocial assessment findings to determine the complexity and intensity of support the patient might need. These therapies, such as cognitive behavioural therapy, aim to help address psychosocial factors that contribute to pain; prevent chronic pain and restore and maintain physical activity and function; and reduce the need for medicines or surgery.
You talk with John about possible interventions for his psychosocial and physical concerns, their costs and his preferences. He agrees to see a physiotherapist to address his work activities and strengthen his back. You also suggest he explore free websites such as MyBackPain or PainHEALTH to receive tailored information to support his self-management and inform discussion at a subsequent consultation.
Judicious use of pain medicines
Although the non-steroidal anti-inflammatory drugs give John some relief, he wonders whether it is time for something stronger.
The goal of pain medicines is to reduce pain to support continuation of usual activities, rather than to eliminate pain completely. Pain medicines should be combined with physical activity and self-management strategies to help improve function and mobility. Patients should be prescribed the lowest effective dose for the shortest possible time, in line with current Therapeutic Guidelines,18,19 with clear stopping goals.
Communication tip:
For most of the medicines used for managing LBP (including drugs for nerve pain and opioid analgesics), there is not strong evidence that they are effective. All of these medicines have potential significant side effects, so it would be best not to use them routinely. If we need to use them, we must do so very carefully and on a short-term trial basis only. If the pain becomes unbearable, we can discuss other options.14
Review and referral
A patient with persisting or worsening symptoms, signs or function is reassessed at an early stage to determine the barriers to improvement. Referral for a multidisciplinary approach is considered. If the patient’s pain is persisting or worsening on review, assess whether the lack of improvement relates to progression of their condition or to physical, functional or psychosocial factors.18 Psychosocial factors should be reassessed and addressed at each review.
Given John is at risk of poorer outcomes based on your psychosocial assessment, you ask him to return for follow up after two weeks, when he will have seen a physiotherapist for further advice and explored the online pain self-management program.
Conclusion
The Low Back Pain Clinical Care Standard provides support for GPs to better manage LBP through a focus on self-management, appropriate messaging and avoidance of unnecessary interventions. The Standard should assist GPs to better manage these often challenging clinical presentations.
Key points
- Principles of management include tailoring a plan to the individual, encouraging self-management and physical activity and identifying barriers to improvement.
- A targeted history and examination should be performed to exclude serious pathology.
- Some psychosocial factors and emotional responses play a major role in the experience of LBP and are linked to delayed recovery from back pain.
- Primary care clinicians should not request imaging if there are no indicators of a serious cause for LBP.
- The goal of pain medicines is to reduce pain to support the continuation of usual activities, including physical activity and work, rather than to eliminate pain completely.