Burnout is common in general practitioners (GPs) worldwide1 to the point of being normalised as it reaches crisis point.2 Burnout is an ‘occupational phenomenon’, caused by persistent and unrelenting workplace demands and unattainable goals.3 Burnout is generally described as comprising overwhelming feelings of exhaustion, disengagement and poor performance efficacy3 that occurs in GPs when one’s ‘wellbeing reservoir’ is depleted.4
Prior to COVID-19, burnout had already reached ‘global epidemic levels’,5 with up to one in every three doctors at high risk of, or already experiencing, burnout.6,7 The risk of burnout has been further exacerbated by the recent pandemic and unprecedented natural disasters, especially for frontline service workers.8,9 Most recently, The Royal Australian College of General Practitioners' (RACGP) 2023 Health of the Nation report, which surveyed over 2000 practising GPs in Australia, found that 71% reported having experienced burnout in the past 12 months in their role as a GP.10
Although it is not a clinical disorder per se, burnout in health practitioners is associated with poor mental health,11 including higher rates of suicide ideation8 and poor physical health,12 as well as low job satisfaction and high intentions to leave.11 Moreover, alongside significant personal and professional consequences, burnout has been linked to reduced quality of patient care.11,13
To date, initiatives to reduce burnout tend to focus on fostering resilience in individuals, such as practising self-care, but with limited effect. For example, a recent randomised controlled trial in over 2000 National Health Service staff in the UK found a significant improvement, albeit with small effects, of the Headspace self-care digital phone app on stress (95% confidence interval [CI]: –0.47 to –0.14) depression (95% CI: –0.40 to –0.08) and anxiety (95% CI: –0.32 to –0.06), but not burnout, compared with an active control (Moodzone).14 Other research has argued that mindfulness interventions designed to tackle burnout and other work-related stressors must be contextualised within a supportive organisational environment to achieve benefits.15
This is aligned with recent calls for systems and government responses to address the workplace and workforce shortage problems associated with burnout.16 Only 13% of medical graduates are choosing to specialise in general practice, representing a 30% reduction in the past five years, heralding a significant workforce shortfall by 2030.17 Moreover, burnout has been linked to accelerating workforce attrition in general practice, which threatens the sustainability of primary healthcare in Australia.10,18
Retention losses also include general practice supervisors, with up to one-third of the supervision workforce intending to leave supervision within the next few years.19 General practice supervisors are the cornerstone of GP vocational training, overseeing the training of several thousand GP registrars annually, hosted in general practices across the country.20 Losses in those willing to supervise raise questions about the future sustainability of GP training in Australia. Research is needed to explore the prevalence of burnout in general practice supervisors, their engagement in self-care practices and risk factors associated with general practice supervisor attrition.
The aim of this exploratory study was to advance understanding of burnout and self-care practices in general practice supervisors in Australia and their intentions to remain in general practice supervision.
Methods
This was a cross-sectional study. Invitations to participate in General Practice Supervision Australia’s (GPSA) online anonymous annual national supervision survey were emailed to GPSA members and advertised in social media and GPSA’s E-News in March–April 2022.
Burnout was indexed using the 16-item Oldenburg Burnout Inventory (OBI),21 to which respondents indicate their agreement with items using a scale from 1 (strongly disagree) to 4 (strongly agree). The OBI comprises two burnout dimensions: Disengagement, referring to negative attitudes towards one’s work; and Exhaustion, arising from prolonged exposure to physical, affective and cognitive strain.21 Following reverse scoring of eight negatively phrased items, items were summed to generate mean ‘Disengagement’ and ‘Exhaustion’ scores, as well as a ‘Total Burnout’ score, ranging from 1 to 4, with higher scores indicating higher levels of burnout. Suggested cut-off scores established in Swiss healthcare workers were applied here, namely >2.1 for Disengagement and >2.25 for Exhaustion.22 The OBI has good psychometric properties.23
Self-care was measured using the Self-care Assessment for Psychologists (SCAP),24 which has relevance to other health professions. The SCAP comprises five self-care dimensions: Professional Support (eg avoiding workplace isolation); Professional Development (eg maximising time in enjoyable professional activities); Life Balance (eg spending time with family or friends); Cognitive Awareness (eg being mindful of triggers that increase professional stress); and Daily Balance (eg taking some time for relaxation each day). Higher scores in each self-care domain indicate higher levels of engagement in self-care. The SCAP has good psychometric properties.24
The Primary Healthcare Practitioner self-care survey25 was used to address respondents’ workplace self-care, such as the amount of annual/personal/sick/mental health leave taken in the past 12 months.
Data were exported from SurveyMonkey and imported into IBM SPSS Statistics V.28. In all, 290 general practice supervisors commenced the survey. Little’s Missing Completely at Random test confirmed that missing OBI and SCAP data were missing completely at random (χ2383=427.25, P=0.059). Expectation maximisation, which provides an unbiased algorithm for predicting missing values, was used to input missing data for participants with <20% missing SCAP data (n=7) and <20% missing OBI data (n=5). Respondents with 100% missing OBI and SCAP data were removed (n=23; <10% of the sample), with the final sample comprising 267 respondents. Two outliers (defined as scores ±3.29 standard deviations [SD]) were identified (OBI: Disengagement and SCAP: Professional Support) across two separate respondents. Inspection of the boxplots identified these as mild outliers and, given that they were within ±3.5 SD, they were not transformed. Hierarchical multiple linear regression (HMLR) analyses were used to explore predictors of Disengagement and Exhaustion; all assumptions were met. Logistic regression analyses were used to explore predictors of general practice supervision attrition. The assumptions of minimum frequencies (>five cases per level of each variable) and goodness of fit (Hosmer and Lemeshow, P>0.05) were met. The standardised residuals of five cases exceeded ±2, but the total number are <5% of total cases. The assumption of logit linearity was violated for one continuous predictor (SCAP: Professional Support), which was removed from the model.
Ethics approval to conduct the study was granted in February 2022 by the Monash University Human Research Ethics Committee (#19442).
Results
Of the 4464 supervisors invited to participate via email, 267 completed the surveys. Sociodemographic and professional factors are presented in Table 1.
Primary health self-care
Of the respondents, 21% (n=56) do not have their own GP and 41.6% (n=111) had worked in the past 12 months while physically or mentally unwell. Most respondents had taken annual leave in the past 12 months (n=247; 92.5%), and almost half had taken personal/sick leave (n=128; 46.1%). Over 10% of respondents had taken leave in the past 12 months for mental illness/stress or burnout (n=33; 12.5%) and almost 60% felt that their self-care/wellbeing could be supported better in their workplace (n=138; 58%).
Self-care
Internal consistency across the five SCAP dimensions was good to excellent (Cronbach’s α=0.79–0.84). In general, average self-care subscale scores suggest relatively high levels of self-care (mean >4.00), except for Daily Balance self-care, which was low (mean [±SD] 3.79±1.56). Up to 12% of the sample (n=33) had low self-care scores on one or more self-care dimensions, relative to mean self-care subscale scores (low score ≤1.5 SD from the mean).
Burnout
Internal consistency across the Burnout dimensions was good to excellent (Cronbach’s α=0.77–0.89). The majority of the sample had high levels of Disengagement (score ≥2.1; n=189; 71%) and Exhaustion (score ≥2.25; n=212; 79.4%), with mean scores exceeding published cut-off points.22 The mean score for Exhaustion was significantly higher than that for Disengagement (2.59±0.55 versus 2.29±0.48, respectively; t266=–12.26, P<0.001). There were no differences in burnout scores according to gender or practice location (metropolitan versus regional, rural and remote).
Predicting burnout
Exhaustion
An HMLR analysis found that 42% of the variance in exhaustion was explained by several sociodemographic, workplace and self-care factors (F12,219=14.31, P<0.001). As indicated in Table 2, general practice supervisors who were younger, those who had worked while physically/mentally unwell in the past 12 months, who held the belief that their self-care could be supported better in the workplace, and those who had lower engagement in daily balance self-care, had significantly higher levels of exhaustion.
Disengagement
A second HMLR analysis found that 30% of the variance in disengagement was explained by sociodemographic, workplace and self-care factors (F12,219=8.80, P<0.001). As indicated in Table 2, general practice supervisors who were younger, had worked while physically/mentally unwell in the past 12 months, and those who had lower engagement in professional development self-care, had significantly higher levels of disengagement.
Predicting general practice supervisor retention
A logistic regression model found that 36% of the variance in retention was explained by sociodemographic factors and burnout (χ2 [13, n=215]=67.53, P<0.001). Older general practice supervisors (odds ratio [OR] 0.276; 95% CI: 0.181–0.422), those who had taken leave for mental illness, stress or burnout in the past 12 months (OR 0.345; 95% CI: 0.125–0.952) and those who had higher levels of disengagement (OR 0.235; 95% CI: 0.085–0.650) were less likely to continue supervising (Table 3).
Self-care was independently and atemporally associated with retention, after accounting for exhaustion, age and working when unwell (b=–0.379; 95% CI: –0.777 to –0.050; Figure 1). These results implicate self-care in shared relationships between exhaustion and retention. There was no significant mediation model for disengagement.
| Table 1. Characteristics of study participants |
| Factor |
Category |
n |
% |
| Age (years) |
<45 |
36 |
13.5 |
| 45–54 |
75 |
28.1 |
| 55–64 |
104 |
39.0 |
| ≥65 |
51 |
19.1 |
| Prefer not to say |
1 |
0.4 |
| Gender identity |
Women |
122 |
46.2 |
| Men |
142 |
53.8 |
| Diversity |
Aboriginal/Torres Strait Islander |
2 |
0.7 |
| LGBTQIA+ community |
9 |
3.4 |
| Live with a disability |
9 |
3.4 |
| Culturally and linguistically diverse |
56 |
21.0 |
| State/territory location of main training practice |
NSW and ACT |
83 |
31.1 |
| Victoria |
67 |
25.1 |
| Queensland |
55 |
20.6 |
| SA |
20 |
7.5 |
| WA |
19 |
7.1 |
| Tasmania |
17 |
6.4 |
| NT |
6 |
2.2 |
| Region |
Metropolitan |
119 |
44.7 |
| Non-metropolitan |
147 |
55.3 |
| Description of main training practice |
Community general practice |
235 |
88.3 |
| State-funded health service |
8 |
3.0 |
| ACCHO |
14 |
5.3 |
| N/A |
2 |
0.8 |
| Other |
7 |
2.6 |
| Role (as many as apply) |
General practice supervisor |
267 |
100.0 |
| Medical educator |
55 |
20.6 |
| GP (principal, partner or practice owner) |
135 |
50.6 |
| GP as employee |
54 |
20.2 |
| Practice manager |
8 |
3.0 |
| GP (sole trader/non-employee) |
47 |
17.6 |
| Other |
10 |
3.7 |
College membership
(as many as apply) |
RACGP |
244 |
91.4 |
| ACRRM |
48 |
18.0 |
| N/A |
5 |
1.9 |
| Other |
6 |
2.2 |
| No. GPs in main training practice |
1–5 |
90 |
33.8 |
| 6–10 |
104 |
39.1 |
| ≥11 |
72 |
27.1 |
| General practice supervision experience (years) |
<2 |
22 |
8.2 |
| 2–5 |
58 |
21.7 |
| 6–10 |
62 |
23.2 |
| 11–20 |
62 |
23.2 |
| ≥21 |
63 |
23.6 |
| General practice supervision – intention to continue |
For the next 5 years |
143 |
53.6 |
| Will stop within the next 5 years |
83 |
31.1 |
| Not supervising in the future |
12 |
4.5 |
| Unsure |
29 |
10.9 |
| ACCHO, Aboriginal Community Controlled Health Organisation; ACRRM, Australian College of Rural and Remote Medicine; ACT, Australian Capital Territory; GP, general practitioner; LGBTQIA+, lesbian, gay, bisexual, transgender, intersex, queer/questioning, asexual; N/A, not applicable; NSW, New South Wales; NT, Northern Territory; RACGP, The Royal Australian College of General Practitioners; SA, South Australia; WA, Western Australia. |
| Table 2. Hierarchical linear multiple regression predicting exhaustion and disengagement |
| Outcome |
Predictor |
b |
SE |
β |
P value |
95% CI |
| Exhaustion |
Age |
–0.064 |
.030 |
–0.111 |
0.036 |
–0.124, –0.004 |
| Working while unwell |
0.295 |
0.062 |
0.267 |
<0.001 |
0.172, 0.418 |
| Self-care workplace support |
0.131 |
0.060 |
0.119 |
0.030 |
0.013, 0.250 |
| Daily balance |
–0.062 |
0.023 |
–0.176 |
0.009 |
–0.108, –0.016 |
| Disengagement |
Age |
–0.073 |
0.029 |
–0.144 |
0.013 |
–0.131, –0.015 |
| Working while unwell |
0.179 |
0.060 |
0.185 |
0.003 |
0.061, 0.298 |
| Professional development |
–0.116 |
0.043 |
–0.264 |
0.007 |
–0.201, –0.032 |
| CI, confidence interval; SE, standard error. |
| Table 3. Logistic regression model predicting general practice supervisor retention |
| Variable |
B |
SE |
Wald |
P value |
Exp(B) |
95% CI |
| Age |
–1.286 |
0.215 |
35.655 |
<0.001 |
0.276 |
0.181–0.422 |
| Mental illness leave |
–1.066 |
0.519 |
4.220 |
0.040 |
0.345 |
0.125–0.952 |
| Disengagement |
–1.448 |
0.519 |
7.771 |
0.005 |
0.235 |
0.085–0.650 |
| CI, confidence interval; SE, standard error. |
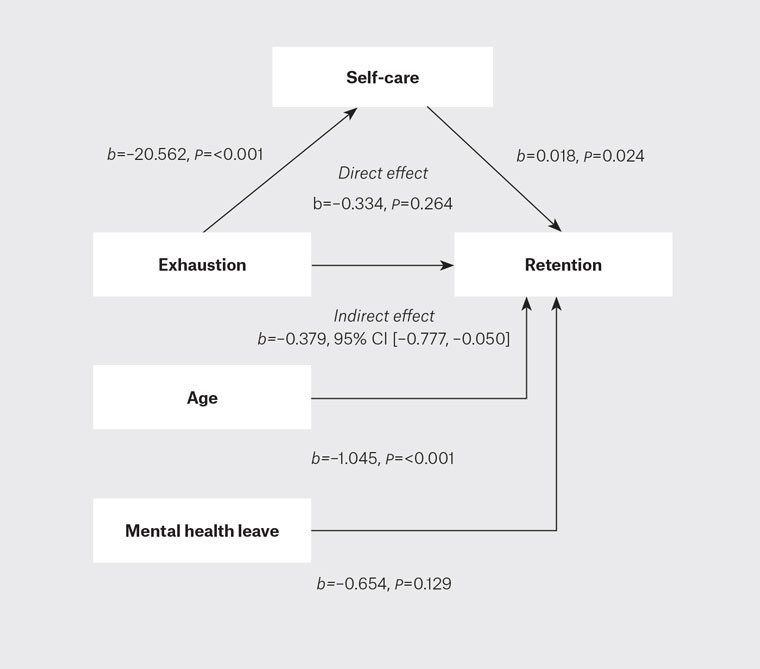
Figure 1. Binary logistic mediation model of burnout as a predictor of retention, mediated by self-care, adjusted for covariates.
Discussion
This study advances understanding of the prevalence of burnout and self-care practices in general practice supervisors in Australia and explores factors linked to intentions to remain in general practice supervision, during a period of extraordinary circumstance and stress in Australia and internationally. Our survey was conducted in March/April 2022, more than two years after the commencement of the COVID-19 pandemic and with COVID-19 cases and restrictions continuing, along with the identification of long COVID.26 The finding that over 70% of general practice supervisors had experienced burnout in the past 12 months (specifically disengagement and/or exhaustion) is consistent with the rates reported in the RACGP’s 2023 Health of the Nation report (survey conducted April/May 2023).10 The rates reported here are within the upper range of prevalence estimates reported in large-scale meta-analyses involving physicians.6 Nonetheless, our findings confirm previous reports of high rates of burnout in general practice10 and extend these specifically to general practice supervisors who had worked through two years of the COVID-19 pandemic at the time of the survey.
Findings from this study also identified risk factors for burnout, showing that younger general practice supervisors and those who worked when they deemed themselves tohave been physically or mentally unwell were more likely to have higher levels of disengagement and/or exhaustion. The belief that one’s self-care is not sufficiently supported in the workplace, as well as poor engagement in daily balance (eg taking breaks throughout the workday) and professional development (eg maximising time in enjoyable professional activities) self-care activities also predicted higher levels of burnout. Given the clear workplace context of these predictors, organisational strategies that empower and support general practice supervisors to set healthy workplace boundaries may go some way towards addressing these issues.
There are several tools and guidelines available to support mental health and wellbeing in the workplace, with recent evidence-informed guidelines recommended to support GP registrars involved in Australian general practice training.27 For example, in Australia, Heads Up and Beyond Blue have partnered to develop a ‘how-to guide for health services’ to ‘[develop] a workplace mental health strategy’.28 Systems and policy-based strategies that foster ‘value fulfilment’29 and workplace resilience through ‘compassion-centred leadership’ may offer a proactive, authentic means by which to build a supportive organisational culture and prevent future burnout.14
Although our cross-sectional study design precludes causal inferences, mediation modelling supports atemporal associations between exhaustion, self-care and general practice supervisor retention. Future longitudinal research that unravels the causal effects of self-care on burnout, or vice versa, and general practice supervisor retention appears warranted. In addition, further research is needed to monitor the mental health and wellbeing of general practice supervisors, given the easing of COVID-19 restrictions, to determine whether measures of disengagement and exhaustion remain high, perhaps due to continuing cumulative impacts of the pandemic.
Limitations
Participation rates in this cross-sectional study were lower than expected (<10% of the general practice supervision workforce), consistent with falling rates of GP research participation reported elsewhere.30 The possibility that the results represent a selection bias preferencing those more affected by burnout seems unlikely, given that the findings reported here are consistent with those of past research,10 suggesting that they are likely to be broadly generalisable to GPs practising in Australia.
Conclusion
Findings from this study confirm that the high levels of burnout seen in primary care doctors around the world extend to those involved in GP training, with younger general practice supervisors at higher risk. Most general practice supervisors felt that their wellbeing and self-care could be supported better in their workplace. Workplace initiatives that support healthy self-care practices, such as setting boundaries and engaging in meaningful professional development activities, may help address the wellbeing crisis in general practice. Given that general practice supervisors experiencing disengagement were more likely to intend to leave supervision, urgent government investment that simultaneously addresses workforce shortages and minimises the burdens on training practices to encourage greater organisational focus on workforce wellbeing and satisfaction is needed to attract and retain Australian general practice supervisors.