Chemical eye injuries are potentially sight threatening. They are uncommon in general practice and present more frequently in rural and regional emergency and urgent care clinic settings.1 They represent 10–22% of all ocular trauma presentations.2 Chemical eye injuries represent three in 100 eye injury encounters in general practice.3 Understandably, primary care practitioners might feel less well prepared to deal with ophthalmic emergencies, particularly chemical eye injuries in rural settings.
A study of 1480 patients who called the Victorian Poisons Information Centre between January 2009 and January 2010 found that among the caustic substances individuals were exposed to, cleaning agents were the most common cause of eye injuries (comprising 32.6% of exposures), followed by personal products (haircare/shampoo; 25.4%), industrial agents (11.8%), pesticides and herbicides (5.7%) and petroleum-based products (4.2%).4 Men sustained industrial agent injuries more commonly than women: 74.8% versus 25.2%.
Primary healthcare providers might not be confident in the assessment and management of ocular injuries due to the infrequent presentation of injuries and lack of training. However, understanding the pathophysiology of the injury and steps for prompt management of a chemical eye injury can prevent the patient from losing vision. The aim of this article is to present a clinically useful guide for general practitioners and urgent care physicians so they feel better equipped in the primary management of chemical-related eye injuries, particularly in rural and regional areas.
Chemical eye irritants
Ocular chemical burns can be categorised as acidic or alkali. Alkali substances tend to have more propensity for injury, as they promote cell membrane lysis and penetrate the cornea deeper, causing denaturation of proteins, fat saponification and liquefactive necrosis, with stromal fibroblast necrosis limiting the repair of denatured stromal collage.5 Alkali substances also penetrate other tissues deeper than acidic substances, including the conjunctiva and skin. Common alkali substances, such as ammonia, can be found in cleaning solutions and nitrogen-based fertilisers; drain cleaners contain sodium hydroxide; and calcium hydroxide is present in plaster and cement (Table 1).
For acidic substances, coagulation necrosis occurs where the burned and denatured proteins form an eschar, and consequently, a natural barrier is created from advancement of the offending substance. This is why an eye injury from acidic substances is likely to be superficial compared to an injury from alkali substances, which can penetrate much deeper. Common acidic substances can be found in car batteries, swimming pool disinfectants, dyes and vinegars.6
| Table 1. Common chemical eye irritants |
| Acids |
| Acid |
Example |
pH |
|
|
|
0.01 |
|
|
|
1 |
|
|
|
2 |
|
|
|
2.6–2.7 |
|
|
|
2.8–7.5 |
|
|
- Rust removers and metal cleaners
|
3 |
|
|
|
3 |
|
|
|
5–7 |
| Alkalis |
| Base |
Example |
pH |
|
|
|
11–12.5 |
|
|
- Chlorine bleach, pool disinfectant
|
11–13 |
|
|
- Nitrogen-based fertilisers
|
11–13 |
|
|
- Caustic soda oven cleaner and
drain cleaner and lye
|
14 |
Initial assessment
Ingestion or inhalation of the caustic substance might trigger prompt resuscitation of the patient, as the airway might be threatened from laryngeal oedema. Ensure prompt treatment for any patient with compromised vital signs. Transferring the patient to a general hospital should be considered if multiple body systems are affected (eg skin and respiratory systems).
Irrigation and pH testing
Once a chemical eye injury has been established, irrigation of the eye should commence immediately. You can never irrigate the eye too much. If a chemical injury is suspected, the clinician should commence irrigation simultaneously with history-taking if necessary. Ideally, pH testing should be performed in both eyes prior to irrigation. If only one eye is affected, the other eye can serve as a reference point when testing for a normal pH level. To test the ocular pH, apply a pH indicator strip to the conjunctival fornix (Figure 1).
If a universal pH indicator strip is not available, a urinalysis strip can be used. The strip will need to be cut down so the pH reading area can be applied directly to the conjunctival fornix (Figure 1). Note that the pH value from the urinalysis strip ranges from 5 to 9 rather than 1 to 10 for the conventional pH strips.
After the materials are gathered (Figure 2), instil a drop of topical anaesthetic into the eye in the form of tetracaine or oxybuprocaine. Irrigate the eye until one litre of a fluid bag has been emptied. Wait for five minutes after cessation of irrigation and check the pH level of the eye again. If a physiologic pH of 7.0 to 7.4 has not been reached, further irrigation with another litre of fluid should occur. For strong acidic or basic substances, irrigation for up to two hours might be necessary. Irrigation should commence with what is currently at the clinician’s disposal. If only tap water is currently available, irrigation under a sink would suffice until the proper materials are sourced. Allow for the water to run from the bridge of the nose towards the ear to ensure that the caustic substance does not affect the other eye.
Any form of intravenous fluid can be used for irrigation (eg Hartmann’s and normal saline), but a warmed solution as opposed to that at room temperature is more tolerable for patients.7
A Morgan lens is ideal for continuous ocular irrigation as it is well tolerated by patients (Figure 2). The Morgan lens is placed directly onto the eyes with fluids connected to its port. A Y-connector should be in place with the line primed for another infusion bag to ensure that the irrigation does not stop.
Nasal prongs can be used if a Morgan lens is not available.8 By positioning the nasal prongs over the bridge of the nose, the irrigation will run down into the eyes. Nasal prongs can be connected to an intravenous fluid bag via a plastic sump connector (Figure 3).
To provide time-sensitive irrigation, especially in the setting of an urgent care clinic, it might be necessary to pre-organise a ‘chemical eye injury pack’ that incorporates all necessary materials for a presentation (Figure 2). It might also be prudent to have an ‘eye assessment pack’ ready for post-irrigation management. The items necessary in such a pack would include topical anaesthetic, fluorescein strips, eye pads, a binocular magnifier, a Wood’s lamp, a pinhole occluder and micropore tape.
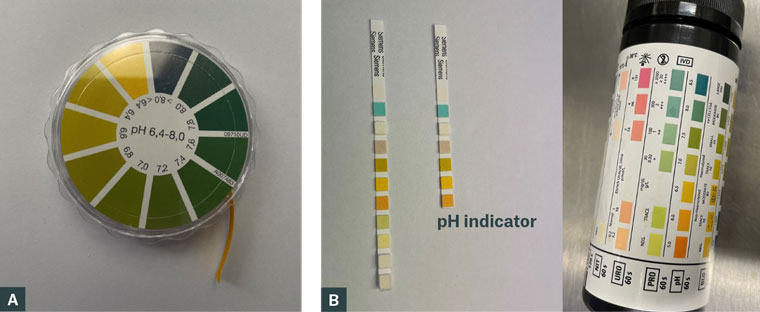
Figure 1. (A) Universal pH indicator strips. Colour change after strip applied to fornix compared to references provided. (B) Urinalysis test strips can be cut down to the pH indicator square to apply the conjunctival fornix and compare against reference values.
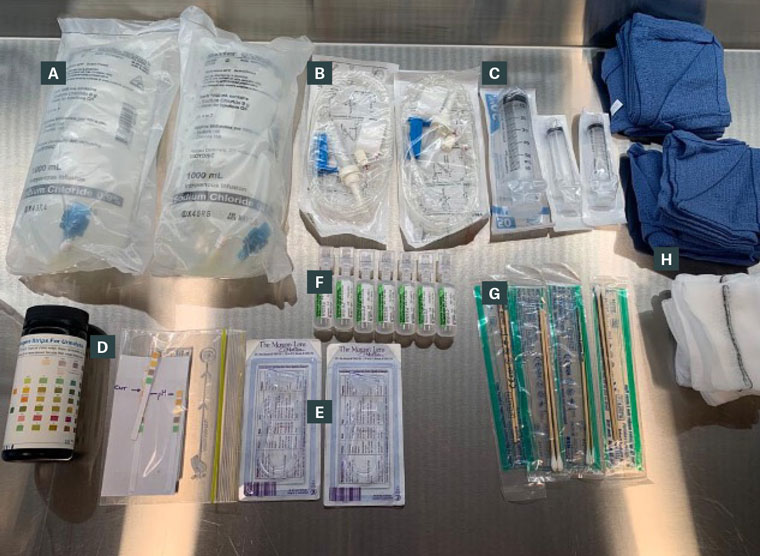
Figure 2. Chemical eye injury emergency box equipment, including (A) 2 1-L bags of normal saline; (B) 2 giving sets; (C) varying sized syringes (D) pH testing strips; (E) 2 Morgan lenses; (F) 10-mL saline ampoules; (G) cotton buds; and (H) gauze and towels.
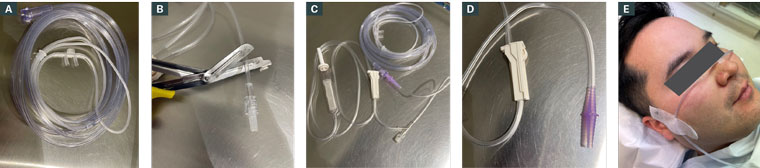
Figure 3. (A–D) The nasal prong connection is removed and replaced with a plastic sump connector. The other end of the connector is attached to an infusion line connected to an irrigation bag. (E) The nasal prongs are placed over the bridge of the nose and the tubing is taped to the side of the face.
Post-irrigation management
After irrigation is complete and pH has normalised, a thorough ocular assessment should be performed. Visual acuity should be assessed using a Snellen visual acuity chart to assess the degree of impairment. There would be an expected degree of decrease in acuity given the microtrauma caused by irrigation. However, a patient with a visual acuity of counting figures would warrant further concern compared to a patient who can read small letters. The eyelid and eyelash margins should be examined. The eyelids should be everted to ensure there is no trapped particulate material in the superior and inferior fornices.
The cornea and conjunctival surface should be examined with fluorescein staining. The deeper layer of the cornea includes the stroma, and the degree of cornea haze should be noted as this predicts visual prognosis.
Damage to the limbus is crucial to note as this can provide information on visual recovery. As the limbal region houses the epithelial stem cells, any form of ischaemia will affect corneal regeneration following damage. The appearance of a pale and blanched limbus (the interface of the cornea and conjunctiva) represents limbal ischaemia.
The Roper-Hall classification can be used to classify chemical eye injuries (Table 2).9 It grades chemical injuries based on the clarity of the cornea and degree of limbal ischemia. Since 2020, the newer Dua classification has been used to grade chemical injuries based on limbal and conjunctival involvement (Table 3).10
After completion of irrigation, further pharmacological therapies can be considered. For all grades of injury, regular oral analgesia should be prescribed. For grade I and II injuries according to Roper-Hall classification, chloramphenicol qid can be used as well as a topical steroid to reduce inflammation (eg fluorometholone or Prednefrin Forte qid).
For more severe injuries, an ophthalmologist should be consulted. Topical chloramphenicol qid and fluorometholone/Prednefrin Forte qh can be considered. In cases of pain due to ciliary spasm and photophobia, topical cyclopentolate 1% or atropine 1% tds can be used. Topical ascorbic acid 10% can be used every 1–2 hours to replenish lost collagen. Systemic ascorbic acid (vitamin C) 500 mg qid can be used to promote collagen synthesis and for pain relief.
| Table 2. Roper-Hall classification for ocular surface burns9 |
| Grade |
Prognosis |
Cornea |
Limbus |
| I |
Good |
Corneal epithelial damage |
No limbal ischaemia |
| II |
Good |
Corneal haze, iris details visible |
<1/3 limbal ischaemia |
| III |
Guarded |
Stromal haze, iris details obscured |
1/3 to 1/2 limbal ischaemia |
| IV |
Poor |
Cornea opaque, iris and pupil obscured |
>1/2 limbal ischaemia |
| Table 3. Dua classification for ocular surface burns10 |
| Grade |
Prognosis |
Limbal involvement (clock hours) |
Conjunctival involvement (%) |
Analogue
scaleA (%) |
| I |
Very good |
0 |
0 |
0 |
| II |
Good |
<3 |
<30 |
0.1–3/1–30 |
| III |
Good |
>3–6 |
>30–50 |
3/1–6/30.1–50 |
| IV |
Good to guarded |
>6–9 |
>50–75 |
6.1–9/51–75 |
| V |
Guarded to poor |
>9–<12 |
>75–<100 |
9.1–11/75.1–99.9 |
| VI |
Very poor |
12 (total limbus) |
100 (total conjunctiva) |
12/100 |
| AThe analogue scale records the amount of limbal involvement in clock hours of affected limbus/percentage of conjunctival involvement. The conjunctival involvement should be calculated only for the bulbar conjunctiva, up to and including the conjunctival fornices. |
Conclusion
Primary care practitioners should feel supported to confidently conduct an initial assessment and instigate immediate management of chemical eye injuries. If additional advice is required, further help can be obtained from locally based optometrists or ophthalmologists. Additional advice can be obtained by calling the Poisons Information Centre if unsure about the pH level of a substance. Ideally, chemical eye injuries associated with an epithelial defect or decreased vision should be reviewed by an ophthalmologist within 24 hours of the initial injury.