The Royal Australian College of General Practitioners (RACGP) and the Royal Australia and New Zealand College of Obstetrics and Gynaecology (RANZCOG) recommend that all people contemplating pregnancy or in early pregnancy should be offered information about reproductive genetic carrier screening (RGCS) for at least the more common genetic conditions that affect children (eg cystic fibrosis [CF], fragile X syndrome [FXS], haemoglobinopathies and spinal muscular atrophy [SMA]) regardless of family history or ethnicity.1,2
In Australia, RGCS is currently offered by several pathology providers, either as a three-condition screen (CF, FXS and SMA) or as expanded carrier screening (ECS) (testing for hundreds of autosomal recessive and X-linked conditions), with a range of out-of-pocket costs.3,4 In November 2023 a new Medicare item number was introduced for RGCS to detect CF, SMA and FXS carrier status.5
The role of general practice in offering RGCS is recognised by stakeholders as crucially important,3 but only a minority of general practitioners (GPs) are offering RGCS in Victoria.6 Although studies have investigated healthcare professionals’ role in ECS in Victoria,7 no study has investigated GPs’ views about screening for the conditions for which the new Medicare item number was introduced.
This study aimed to investigate facilitators and barriers to offering RCGS for CF, SMA and FXS in general practice.
Methods
This study explored the views of GPs who have offered a three-condition screen for CF, SMA and FXS carrier status provided by Victorian Clinical Genetic Services (VCGS), a not-for-profit genetic pathology service that is a wholly owned subsidiary of the Murdoch Children’s Research Institute. This screen is offered through doctors, including GPs and obstetricians. It is the most widely offered RGCS in Victoria.6 Up until November 2023, patients incurred an out-of-pocket cost of $389 for this screen.
Study design
A qualitative approach using semi-structured interviews of a subset of Victorian GPs offering the screening was undertaken. The study used a descriptive phenomenology outlook, which investigates an area of interest from the perspective of those involved,8 and behaviour change theory was used as a methodological framework.9 An interview guide was developed using a behavioural change framework.9,10 At the centre of the framework is a ‘behaviour system’ termed the ‘COM-B system’, which involves three essential conditions: capability, opportunity and motivation. This framework has been used extensively in healthcare research to describe behaviour and to help bring about behaviour change in line with evidence-based practice.10
Researcher characteristics and reflexivity
The interviewer and lead author, RL, is an experienced older Victorian GP who might have had preconceived assumptions about RGCS based on her own experience, attitude and beliefs. Having a GP as an interviewer might have helped with rapport and communication but also might have led to unchallenged, shared assumptions and attitudes, or fellow professionals wanting to present themselves in a certain light to colleagues. Her co-authors, most of whom were not GPs and were experienced in qualitative research, helped by providing guidance regarding qualitative research techniques.
Data collection
A list of GPs who had requested the VCGS three-condition screen was available from the VCGS database. Participant GPs were selected using purposive sampling,11 based on the frequency with which they had requested the screen for their patients between September 2013 and October 2018. Low-frequency requesters (LFR) were categorised as those GPs who had requested this screen once and high-frequency requesters (HFR) were categorised as those GPs who had requested the screen on more than 25 occasions (top fifth percentile of GPs by frequency of request6). Purposive sampling was also used among LFRs to select GPs based on sex and the location of their practice. All HFRs were women and worked in metropolitan areas (Figure 1). Selected GPs were contacted via fax and invited to take part in a telephone interview. Verbal consent was obtained from the participating GP, and the interviews were audio-recorded. Interviewing continued until no new information was emerging from the interviews. Interviewed GPs received a $100 gift voucher. The interviews were undertaken between March 2019 and June 2021. The study duration was longer than expected due to disruptions caused by the SARS-CoV-2 pandemic.
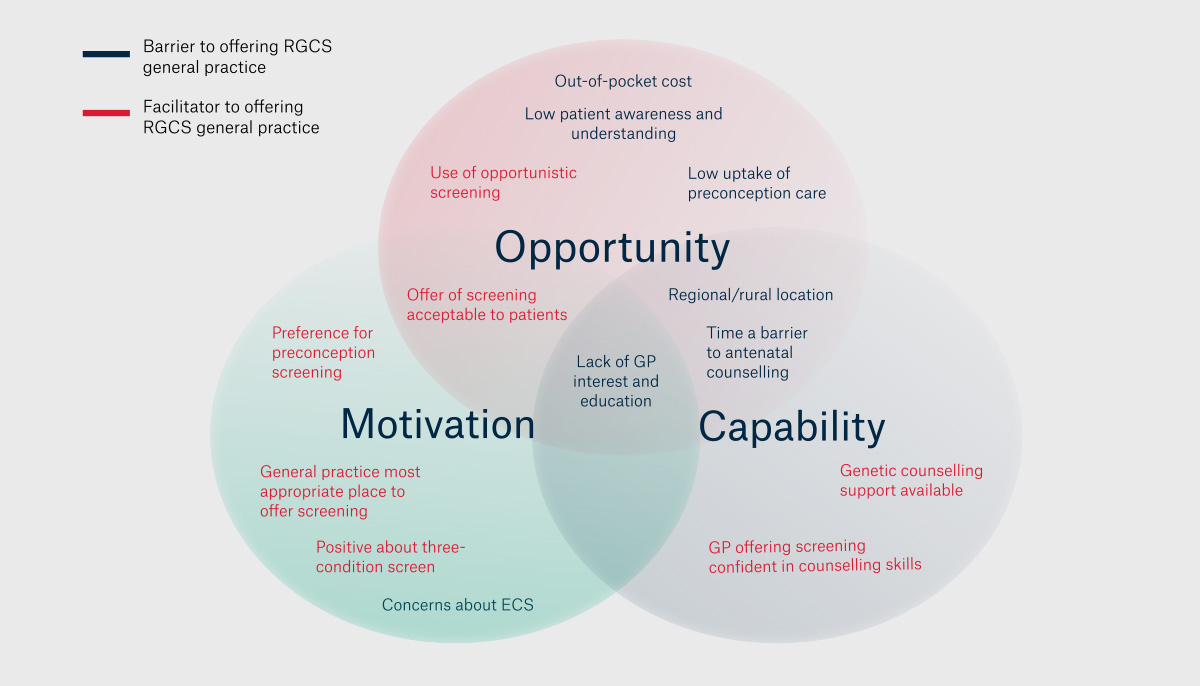
Figure 1. Facilitators and barriers to offering RGCS in general practice mapped onto the COM-B system.9
ECS, expanded carrier screening; GP, general practitioner; RGCS, reproductive generic carrier screening.
Data processing and analysis
Interviews were transcribed verbatim and subsequently de-identified. Data and coding were managed using NVivo (version 12, Lumivero, 2018). The initial transcripts were coded by one researcher (RL) and then co-coded by two other researchers (AA and SL). Coding differences were discussed and a common coding scheme was created. The subsequent coding was completed by RL, with ongoing discussion among coders. Related codes were organised into themes and then reorganised as an iterative process after discussion among the three coders.12 Emerging themes were then mapped onto the behavioural framework using the COM-B system.9
Results
Selection and characteristics of participants
Of the 860 Victorian GPs who requested the VGCS three-condition screen between September 2013 and October 2018, 587 (68%) were eligible for this study; that is, they were either HFRs or LFRs (Table 1). A total of 24 HFRs (49% of all HFR) and 26 LFRs (5% of all LFRs) were invited for interview. Nine HFRs and six LFRs agreed to participate in an interview. Interviews lasted between 14 and 26 minutes, with a median length of 21 minutes. All HFRs were women, worked in the metropolitan area and provided antenatal shared care. Half the LFRs were men. Two lived in rural locations, one provided shared care and one was a GP obstetrician.
Many of the HFRs described offering the three-condition screen to all women attending for preconception care and all pregnant women. In contrast, the LFRs had not incorporated this screening into their regular care. Among the six LFRs, two described how they were increasingly offering RGCS as they became more familiar with it, two commented that they only offer it to women before pregnancy but do not see many women in this category, and two GPs had only requested the test when requested by a patient.
|
Table 1. Selection and characteristics of participants
|
| |
Total number of general practitioners
|
Invited for an interview
|
Interviewed
|
|
High-frequency requesters
(ie >25 requests)
|
49
(all female)
|
24
(all female)
|
9
Sex: all female
Location: all metropolitan
Maternity qualifications: all shared care
|
|
Low-frequency requesters
(ie 1 request)
|
538
(349 female, 189 male)
|
26
(9 female, 17 male)
|
6
Sex: 3 male, 3 female
Location: 2 regional, 4 metropolitan
Maternity qualifications: 1 shared care,
1 general practitioner obstetrician
|
Mapping themes onto the COM-B system
Themes that predominantly map onto the ‘motivation’ domain
Positive attitude to the concept of offering the three-condition RGCS and viewing general practice as the most appropriate place for RGCS to be offered
Both HFRs and LFRs expressed broadly positive attitudes to the concept of offering the three-condition screen and agreed that general practice is the most appropriate place for this screen to be offered (Figure 1). Reasons given were that GPs know their patients best, they see women/couples prior to pregnancy, they are the first healthcare professional to see pregnant women and they are often the only healthcare professional women see in the first trimester of their pregnancy:
We (GPs) are the ones who see the people in the beginning of their pregnancy and also pre-pregnancy … I can’t imagine where else they are going to find out about it. (Helen, HFR)
Concerns about ECS
In contrast to their attitude to the three-condition screen, many of the GPs expressed concern about counselling for ECS (with hundreds of autosomal recessive and X-linked conditions screened for from one sample). They acknowledged their lack of knowledge about many of the conditions included in the ECS and questioned whether screening for so many conditions is beneficial to the patient:
I really have no sense of the broader panels of testing … And what sort of can of worms that opens up. (Vera, HFR)
I’m quite comfortable about the short panel, but when they start talking about the extended ones … what does it actually mean? (Bob, LFR)
Preference for preconception screening over antenatal screening
GPs were all in agreement that offering screening before pregnancy is preferable to offering screening during pregnancy. Patient anxiety and time constraints for GPs are seen as more problematic when offering screening during pregnancy compared to before pregnancy:
In those first few visits (in pregnancy), you’re pretty time poor and the rush to get through as much as possible in that visit. (Simon, LFR)
Early pregnancy (screening) is OK, but it leads to the issue, as has happened to me once before, where a test comes back positive and mum is already 9–10 weeks pregnant and dad is frantically having his test done, and everyone is a bit on edge waiting to see what happens. (Susan, HFR)
The offer of RGCS is acceptable to patients even if they decide against screening
GPs reported that women are broadly positive about being offered screening and that those women who choose not to take up screening do not express concerns about being offered screening. They stated that a common response among women choosing not to take up screening is that a positive result would not affect their future behaviour:
I’ve not had anyone be hostile, but they (say) ‘I’m just not interested in doing it’ or ‘I wouldn’t act on it if I had a child that was affected by disease, so that’s not for me’. (Anne, HFR)
Themes that predominantly map onto the ‘capacity’ domain
Confident in ability to undertake pre-test counselling for the three-condition screen
Despite differences in frequency of screening, all the GPs felt confident in their ability to undertake appropriate pre-test counselling for the three-condition screen. LFR GPs felt that even if they are not across all the details of the screening offered, they are able to explain basic concepts and direct the patient to the relevant written information for more details. A parallel between the skills required for offering non-invasive prenatal testing (NIPT) and those required for offering RGCS was postulated by some interviewees:
Yeah, I feel skilled enough to talk about what’s on offer. Probably not so much about the actual details, you know the sensitivity and specificity of the test, but enough to explain what’s on offer, what we’re looking for in terms of CF and FXS. (Simon, LFR)
Yes, I think so. I have a good understanding of the genetics of cystic fibrosis, not so much the fragile X and the spinal muscular atrophy … I don’t think I need to know more about the details of those for my role in offering the test. (Helen, HFR)
In many ways, I’m always talking about something similar when I’m talking about the NIPT as well. (Bob, LFR)
GPs all described using written information (ie brochures/information sheets and/or directing patients to online websites) as part of the counselling process. Involving the patient’s partner in decision-making was acknowledged as important. The GPs offering screening described how the process became easier with time.
Presenting information about RGCS but not influencing the patient and allowing them to decide was seen as very important:
I don’t suggest that they do or don’t; I just give them the information so that they can decide for themselves … And really whether they decide to or not is not really my business. (Anne, HFR)
Level of GP knowledge and interest in reproductive medicine is a major factor in frequency of offering screening
Lack of awareness and education around RGCS were mentioned as common reasons why many GPs are not offering screening. Personal preferences of GPs for particular areas of medical practice were seen to play a role in differences in frequency of offering RGCS:
It’s another thing GPs should do, and for some GPs, it’s not that important to them. Maybe it’s not going to be high on their list of priorities. (Sally, LFR)
There’s a lot of GPs whose focus is on skin or diabetes or heart disease, who really don’t have the knowledge that would be required to do it properly. (Anne, HFR)
Level of genetic counselling support offered by pathology affects GP confidence in offering screening.
The importance of support from the pathology provider for follow-up genetic counselling services was expressed by many GPs and guided their choice of pathology provider.
Themes that predominantly map onto the ‘opportunity’ domain
Socioeconomic and educational status of patient affects access
There was universal agreement among the GPs that the out-of-pocket cost of RCGS is a major barrier to uptake of screening, and some felt uncomfortable offering an expensive test to women who might not be able to afford it. Several GPs mentioned the desirability of screening being government funded. Counselling women was noted to be easier and quicker when patients are from a well-educated demographic:
It’s a fairly knowledgeable patient base that I see anyway. You’re probably starting already from the half-way point. (Susan, HFR)
… to explain something like genetic testing to someone whose English is a second language or who hasn’t gone to school, … in particular locations of general practice and in particular demographics; this kind of stuff is boutique medicine, really. I can understand why a GP just wouldn’t even have a conversation about a $400 test for a patient that, you know, is just living from week to week. (Anne, HFR)
Rural/regional location could make follow-up more difficult and increase costs
Concerns about potential delays in follow-up and incremental costs were aired as potential problems for rural and regional patients:
I do worry, once we get a result, that that person is adequately counselled around the result and that we’ve got access to genetic counsellors quickly. In the past, it’s been difficult because access is usually going to Melbourne, and it’s a struggle for some families, just the escalation in cost. So, I certainly think these things might be a bit of a barrier to me opening up a Pandora’s box. (Bob, LFR)
Variation in time taken for pre-test counselling
There were a variety of opinions about the time required to provide adequate pre-test counselling. The importance of taking time to counsel the patient thoroughly was raised by some. Others felt that a long discussion is unnecessary and undertake only brief counselling with their patients:
Well, it’s obviously quite complicated, and so I want to make sure they understand it all beforehand, so it’s not particularly quick. (Jenny, LFR)
I give them brief counselling because there is never time for too much (laugh) … general practice is not the place to go into detail. (Helen, HFR)
Time constraints and competing priorities emerged as a larger barrier to offering screening in early pregnancy compared with preconception counselling.
Level of awareness and understanding of RGCS among patients
GPs reported that women responded less positively to the offer of RGCS compared to screening for chromosomal conditions and ascribed this to lack of familiarity. Additionally, the conceptual understanding required to assess risk and then understand the options available in the event of a positive result was reported as challenging and off-putting for some patients. Some patients erroneously assumed that that screening is not appropriate where there is no family history of the conditions:
They’ll say, ‘I’ve always known about having the test for Down syndrome, didn’t know about this test’, ‘my friends didn’t have it’ or ‘I didn’t have it in my last pregnancy so I don’t think I’ll bother this time’. (Linda, HFR)
I often have people say to me, ‘Oh, I have none of these conditions in my family, so I don’t think I will’ … so I explain that most people (who) are found to be carriers don’t have family members … That is a common misunderstanding. (Helen, HFR)
Variation in uptake of preconception care related to socioeconomic demographic of patients.
A high uptake of preconception care was notable among HFR GPs. In contrast, LFR GPs expressed frustration at the poor uptake of preconception care. HFR GPs ascribed their high uptake of preconception care to the high socioeconomic demographic of their patients. They also described use of opportunistic preconception counselling during other consultations, particularly women’s health-related consultations. This approach was seen to work best when there is continuity of care:
I often laugh because I get so excited when someone comes in to prepare for pregnancy; it’s such a rarity. I usually get, ‘Oh my god, I’m pregnant! I need to find a doctor’. (Simon, LFR)
I work in the CBD of Melbourne, so I’m fortunate to work with very motivated, intelligent patients who usually, not always, have a consult before they even try and get pregnant. (Alice, HFR)
Often, I have prompted them to have made that (preconception) visit. So, if they indicate that they are contemplating family planning over the next 12–18 months, then I usually say, ‘Please come and see me three months before you are planning to actively try’. (Vera, HFR)
Low level of community education about preconception care
There was recognition that public awareness around the benefits of pregnancy planning is low. Various ways of promoting preconception care were suggested, including use of posters, social media and education in high school:
I don’t think there is general public awareness about pre-pregnancy check-up. We promote contraception, but we don’t promote pregnancy planning as well. (Carol, HFR)
Summary of findings
Many of the barriers to screening mapped onto the ‘opportunity’ domain, which includes social influences and environmental context and resources (Figure 1).10 Using the behaviour change framework wheel at the policy level,9 changes in fiscal measures (eg government funding), service provision (eg in rural and regional areas) and communication/marketing (eg related to delivery and uptake of preconception counselling) might be measures that lead to a reduction in opportunity barriers. The main barrier in the motivation/capability domain is lack of interest and/or lack of education of GPs in RGCS.
Discussion
This study of GPs’ views of RGCS found that major facilitators to GP screening were a positive attitude towards the three-condition RGCS and confidence in counselling skills. Major barriers were cost, low awareness and knowledge about RGCS among many GPs and patients and low provision of preconception care in many GP settings. Many of these findings are similar to those of a study of healthcare professionals offering ECS.7 Most barriers mapped to the ‘opportunity’ domain using the behaviour change framework.
The introduction of government funding for CF, FXS and SMA carrier screening has now removed the out-of-pocket cost for this form of RGCS, thus removing one of the major ‘opportunity’ barriers to offering screening. This will, no doubt, lead to an upsurge of interest by GPs and patients in the three-condition screen. Improving GP awareness and education about RGCS, so that general practice is equipped for this change, is vitally important.
However, some barriers in the ‘opportunity’ domain of the behaviour change framework will remain, such as the provision and cost of some follow-up tests (currently prenatal testing is available free of charge in the public system, but preimplantation genetic testing is not and is associated with significant out-of-pocket expenses). For couples living in rural or regional areas, access to follow-up for genetic counselling, prenatal testing or in vitro fertilisation with preimplantation genetic testing is a significant barrier to RGCS. Similar barriers to access to screening programs and preconception care have been found in other studies.13 Additionally, the educational level and cultural and ethnic backgrounds of patients are likely to remain a source of inequity.14
The GPs’ preference for preconception RGCS over antenatal RGCS is in accordance with the expressed preference for preconception screening among other health professionals and stakeholders.15 Time constraints in antenatal consultation already crowded with healthcare issues and concern about causing increased anxiety to women at a vulnerable time in their lives are issues highlighted in this study and also described in the literature.16 Additionally, it is well recognised that preconception screening increases the reproductive choices for women found to be at increased risk by screening.3 Despite this strong preference for offering screening before pregnancy, studies have shown that most RGCS requested by GPs are in early pregnancy.6 The frustration expressed in this study at the poor uptake of preconception care in general practice mirrors findings from other studies.13,17 Offering RGCS as part of a holistic GP preconception care consultation provides a model by which GPs could incorporate RGCS into their practice.3 There is strong evidence for the benefits of preconception care in general practice for improving pregnancy outcomes.18,19 The RACGP’s ‘Guidelines for preventive activities in general practice’ (Red Book) outline evidence-based recommendations covering such items as immunisation status, previous adverse pregnancy outcomes and patient lifestyle.20 A new updated version is planned that will include recommendations for RGCS that are consistent with those of RANZCOG.
The lack of public health education about planning for pregnancy compared with other areas of health promotion, noted by the GPs in this study, is in line with many studies that have shown that women of reproductive age demonstrate low levels of knowledge and behaviour related to preconception care.21,22 Raising awareness of the importance of preconception care in the community should be a priority. There are multiple Medicare Benefits Schedule (MBS) item numbers used in general practice to promote public health and preventative health measures. In view of the strong evidence for the benefits of preconception care in general practice for improving pregnancy outcomes18,19 and the advantages of offering RGCS before pregnancy, the introduction of the MBS item number for RGCS might prompt consideration of the public health benefits of introducing an item number for preconception care.
GPs in this study placed emphasis on being non-directive when offering screening, seeing their role as giving patients information and allowing the patient to come to their own decision about proceeding with screening. This approach aligns with the concept of reproductive autonomy for the patient.3 As RGCS becomes more common, it is important that GPs continue to respect reproductive autonomy and are vigilant to avoid ‘routinisation’ when offering RGCS.23
The misgivings expressed in this study about ECS burdening patients with information about their status as carriers of multiple rare genetic conditions might be unfounded if couples-based screening (where only couples who both carry a mutation for the same condition are notified) is used.24 Outcomes from the prospective study Mackenzie’s Mission,25 which offered couples-based screening, will help further clarify the acceptability of ECS with couples-based screening.
Limitations
Focusing only on GPs who have had experience of offering RGCS limits this study’s generalisability, as GPs who offer RGCS are still a minority in the state of Victoria.6 ‘Early adopters’ might have a more favourable attitude to RGCS than GPs not presently engaging in RGCS. Additionally, views of GPs might have changed since the completion of these interviews. Both the availability of the interviewer and recruitment of GPs was affected by the change in priorities in general practice over the SARS-CoV-2 pandemic.
Conclusion
In conclusion, undertaking changes that address the ‘opportunity’ domain of the behaviour change framework, particularly reducing out-of-pocket costs, delivering preconception care and improving GP education around RGCS, will provide more people with the opportunity to make informed choices about participation in RGCS.