This article is part of a longitudinal series on ear, nose and throat conditions.
Allergic rhinitis (AR) is a Type 1 IgE-mediated hypersensitivity reaction to airborne allergens, most commonly dust mites, tree, weed or grass pollens, in addition to animal dander and mould.
The pathophysiology is well understood, with allergen exposure triggering an immediate early phase response with mast cell degranulation and a histamine response in the nasal mucosa1 causing rhinorrhoea, postnasal drip, sneeze, itch and nasal congestion.2 Eosinophils and other inflammatory cells then contribute to late phase symptoms of chronic nasal obstruction, hyposmia and nasal mucosal hyper-reactivity.
AR is a prevalent condition affecting people of all ages, with the prevalence in Australia during 2017–18 being almost one in five.3 Worldwide, the prevalence of AR ranges from 5% to 50%;4 however, it is often underdiagnosed and inadequately managed.5 AR can have a significant effect on quality of life and affect school/work, productivity, sleep quality, mood and concentration in both adults and the paediatric age group.4,6,7
Although AR peaks in the 25–44 years age range,3 it is important not to miss this diagnosis in children presenting with sleep disordered breathing, obstructive sleep apnoea, snoring, behavioural issues and frequent upper respiratory tract infections. Children are underdiagnosed because they are unable to describe their symptoms. AR accounts for 0.6% of general practitioner (GP) presentations,3 likely an under-representation due to self-medicating from pharmacies. AR should be considered in all of those with asthma because the concurrence is 60–80%.
The risk factors for developing AR include genetic factors, atopy during childhood, eczema and higher socioeconomic status.4 Interestingly, some factors previously thought to contribute to the risk of AR, such as tobacco smoking, pollution, and early exposure to dust mites, pollen, animal dander and fungal allergens, all have inconclusive evidence.4 The prevalence of AR in large polluted Asian cities is on the rise compared with the rural areas of the same countries.8 Although the connection between poor air quality and AR is not understood, it is clear that more people are developing AR in those cities with poorer air quality.8
There are certain factors that have been demonstrated to be protective against developing allergic rhinitis. This includes Level 2 evidence for breastfeeding, and some evidence for microbial diversity.4,9
In recent years, there have been several developments in the investigation of AR, including component resolved diagnostics,10 e-diaries11 and aeroallergen monitoring applications.12 Management has broadened also, including the recent introduction of combination intranasal corticosteroid and antihistamine sprays, as well as the availability of self-administered sublingual immunotherapy wafers and dissolvable tablets that can target grass pollen and house dust mites.13 Antigen-specific immunotherapy is effective, available and the only form of disease-modifying therapy available currently.4
For comprehensive information on this topic, the authors highly recommend accessing the Australasian Society of Clinical Immunology and Allergy (ASCIA) Allergic rhinitis clinical update, published in 2022 and available online.14 Alternatively the updated International consensus statement on allergy and rhinology is an extensive document that has pooled evidence-based reviews and recommendations for the investigation and management of allergic rhinitis.4
The objective of this article is to provide a contemporary and accessible framework for the clinical assessment, investigation and management of AR in the primary care setting and to establish appropriate referral criteria for ear, nose and throat and/or allergist/immunologist referral.
Assessment
The aim of assessment is to determine whether the condition is indeed AR, to gauge the severity and effect of disease and to exclude other differential diagnoses, including common conditions (ie non-allergic rhinitis, chronic rhinosinusitis), and to exclude red flag conditions, including malignancies and benign neoplasms. A detailed and targeted history is the first (key) element of the clinical assessment for AR. This includes establishing the hallmark symptoms of rhinorrhoea, sneeze, itch, nasal obstruction and concurrent allergic conjunctivitis, as well as associated symptoms such as postnasal drip and nocturnal cough. Establishing seasonal patterns and/or environmental triggers, including pets in the house and soft toys, is of value and can help guide subsequent specific allergen testing. A family or personal history of atopy might be corroborative. An early referral to otolaryngology should be considered if unilateral nasal obstruction, progressive blood-stained, malodorous nasal discharge or unilateral nasal polyps are present.
Validated survey instruments can be used to screen for AR and might offer a more structured and standardised means of obtaining the clinical history, including the effect on quality of life; in addition, they can more objectively assess treatment response. For primary care, the Control of Allergic Rhinitis and Asthma Test (CARAT-10) is a good option, being relatively short and accessible.15 These questionnaires can be used in children and adults and concurrently assess for conjunctivitis and asthma.
Physical examination with anterior rhinoscopy might show an increased volume of clear, sticky mucus and pale oedematous swelling of the inferior turbinates. Other causes of nasal obstruction, such as a significant septal deviation, polyps or a sinonasal mass, should be excluded. Fibreoptic nasendoscopy undertaken by an otorhinolaryngologist or an allergist can assess for allergic/oedematous changes of the middle turbinate, exclude a large adenoid in older children who can tolerate this examination and exclude alternative pathologies. Nasoendoscopy is not essential to the diagnosis of AR, but direct anterior rhinoscopy, with an effective light source, is highly informative and should be performed in all patients with nasal symptoms.
If the history and examination is suggestive of AR, the diagnosis can be further supported by either referring the patient to an allergist for skin prick testing (generally accepted as the gold standard) or requesting a specific panel of blood tests available from any pathology provider. The latter is more accessible to most GPs and might include a full blood count and as well as serum allergen-specific IgE levels (previously known as the radioallergosorbent test or RAST) to specific allergens that are suggestive from the history. Medicare will rebate four single allergens, two mixed allergen panels or two single and one mixed allergen panel per testing episode, with additional panels available usually at a minor cost to the patient. These tests should be targeted to the patient’s specific environmental triggers: Dust and Mite Mix, Grass Mix, Pollen Mix and Animal Danders should be considered because they are common. Animal Danders should be specific if the patient has exposure to a certain animal because mixes are not specific. Other available tests include Weed Mix, Tree Mix, Mould Mix and Occupational Mixes (only to be requested if a person has a specific occupational exposure; eg bakers).16
For accurate skin prick testing, it is important to ensure that patients have withheld oral H1 receptor antihistamines for at least two to seven days prior and topical antihistamines for at least two days. Tricyclic antidepressants might affect results; this will be taken into consideration by the allergist if skin prick testing is inconclusive. Systemic corticosteroids and topical corticosteroids (provided not used at the testing site) can be continued. Of note, an elevated serum IgE or an eosinophilia is non-specific, unless in eosinophilic airways disease,17 and false positives are common. A positive test without corroborative clinical symptoms is not relevant and should not be acted on.
Radiological imaging is not indicated in the work-up for AR. Imaging should only be considered to rule out other causes of nasal obstruction/rhinorrhoea if the history and examination is unconvincing.18 It is important to note that nasal obstruction might be a combination of allergy and anatomical obstruction from large adenoids and/or septal deviation.19
Management
The four main aspects to the management of AR are allergen avoidance, pharmacotherapy, immunotherapy and, occasionally, surgery.
Allergen avoidance
Avoidance measures are considered a low-risk option and can be effective. They do frequently entail significant inconvenience, cost, lifestyle modification and even disruption to one’s occupation. Adherence can be challenging, even for the most diligent of patients. Allergen avoidance has been found to be specifically effective for the following allergens: house dust mites, cockroaches, pets, rodents and pollen.4 Portable home air filter units have increasing evidence of their effectiveness against some aeroallergens, especially pollen.20 House dust mite avoidance is nearly impossible in areas of high prevalence, such as temperate and humid coastal regions of Australia. Reduction measures might be helpful, but certain measures, such as sheet/pillow protectors, might be expensive.
Pharmacotherapy
Pharmacotherapy can be separated into first-line agents, second-line agents and other options.
First-line agents are all available over the counter and include the following:
- Intranasal saline sprays or rinses: these can be used to clear mucous and reduce local allergen load. These are a cost-effective management option with no side effects and can help alleviate symptoms.21
- Intranasal corticosteroids (eg mometasone, budesonide, fluticasone): used regularly for a minimum of four weeks these are highly effective and have a preventative role.22 Correct administration technique is important.23 Poor technique might increase the risk of bleeding from Little’s area and can be combated by both improved technique as well as the use of emollients or combination antibiotic, antifungal and corticosteroid ointments.
- Intranasal antihistamines (eg azelastine, levocabastine): these have minimal side effects and can reduce symptom burden acutely, with a reduction in itch, sneeze, rhinorrhoea and eye symptoms soon after they are used.24
- Combinations of intranasal corticosteroid and antihistamine sprays (eg azelastine/fluticasone, olopatadine/mometasone): these are now increasingly recognised as an excellent first-line option. In Australia, azelastine/fluticasone has recently been scheduled S2 and is available over the counter, whereas olopatadine/mometasone is prescription only. These combinations have the benefit of the preventative action of the steroid and the symptomatic relief of the antihistamine when used for a minimum of one month. They have only been available in recent years and have been strongly recommended for the management of AR.4 The senior author of this paper feels a strong argument can be made to use one of these combination sprays as the first-line treatment, particularly as more rapid results might improve compliance.
- Oral H1 receptor antihistamines (eg cetirizine, loratadine, fexofenadine): these are less effective, have a slower onset and have more side effects than topical antihistamines. However, they have a role to play in those unwilling to comply with topical delivery.24
- One of the few second-line agents is intranasal sodium cromoglycate, which can be a useful prophylactic treatment and has minimal adverse effects.25,26
Other pharmacotherapy options that should only be considered if first- and second-line agents are insufficient include the following:
- A ‘pulse’ or brief course of oral corticosteroids (eg prednisolone) if not contraindicated: this can be prescribed with the aim of improving congestion to allow the penetration of first-line topical sprays. Oral corticosteroids should not be prescribed routinely or frequently due to systemic adverse effects.4
- Leukotriene receptor antagonists (eg montelukast): these can alleviate symptoms.27 Despite having a rare side effect of behavioural disturbance, leukotriene receptor antagonists are particularly useful in young children and those with asthma who cannot tolerate nasal sprays.28
- Oral and intranasal decongestants (eg phenylephrine, diphenhydramine, pseudoephedrine): these are effective in the short term at improving nasal patency and provide rapid temporary benefit. However, they cause significant rebound congestion with extended use and patients can very easily become dependent on these medications (rhinitis medicamentosa); therefore, their use should be short-lived only.29
Immunotherapy
Immunotherapy can be considered if the above pharmacotherapy agents do not sufficiently treat the symptoms or the patient is seeking an alternative to medical management. Immunotherapy involves the controlled exposure of allergens to a patient in order to reduce the hypersensitivity response. It can be delivered using several methods:
- subcutaneous immunotherapy (SCIT) with serial injections is one of the most common delivery methods and has the strongest evidence of efficacy, but also the highest risk of systemic adverse events4
- sublingual immunotherapy (SLIT) also has evidence of efficacy and the added benefit of a less-invasive self-administration route and less risk of adverse side effects compared with SCIT.4 The duration of protection from immunotherapy is 10–20 years. This might be much more acceptable for the paediatric population, who might wish to avoid injections.4,30,31
GPs might be asked to assist with the maintenance injections for aeroallergen immunotherapy prescribed by allergists, using a shared care model. GPs need to be aware of the risks of this therapy, including possible anaphylaxis, and have necessary resuscitation equipment and have completed ASCIA anaphylaxis training. GPs should also have clear guidelines from the prescriber about dose adjustment if injection intervals vary or side effects occur.32
The non-Pharmaceutical Benefits Scheme prescription of grass, pollen and dust mite sublingual tablet or wafer therapy is safe and within the remit of GPs for monosensitised patients who have a consistent clinical history and aligning investigations. For more complex patients, usually an allergist will need to be involved.33
New biological agents have shown benefits that might be relevant in the management of AR.34 These monoclonal antibodies can target specific aspects of the allergy pathway. Omalizumab, which targets IgE, has a significant body of evidence supporting its use in AR, but it is currently not approved for use for this indication.34
Surgery
If medical measures are insufficient to treat the patient’s symptoms, then referral to an otolaryngologist should be considered. Inferior turbinate surgery might be performed to reduce the soft tissue bulk of the nasal sidewall, thereby decreasing nasal congestion and rhinorrhoea. If a significant septal deviation exists, then a septoplasty can help address nasal obstruction. In children, adenoidectomy and/or ablative procedures on the inferior turbinate can be undertaken. Of note, however, the underlying allergic tendency will not be addressed by surgery and the patient will likely still require pharmacotherapy to address itch, sneeze and rhinorrhoea.35 Vidian neurectomy and radiofrequency ablation are procedures that disrupt the posterior nasal nerves and are only considered infrequently in the management of AR.4
See Figure 1 for a flowchart summary of the approach to the management of AR.
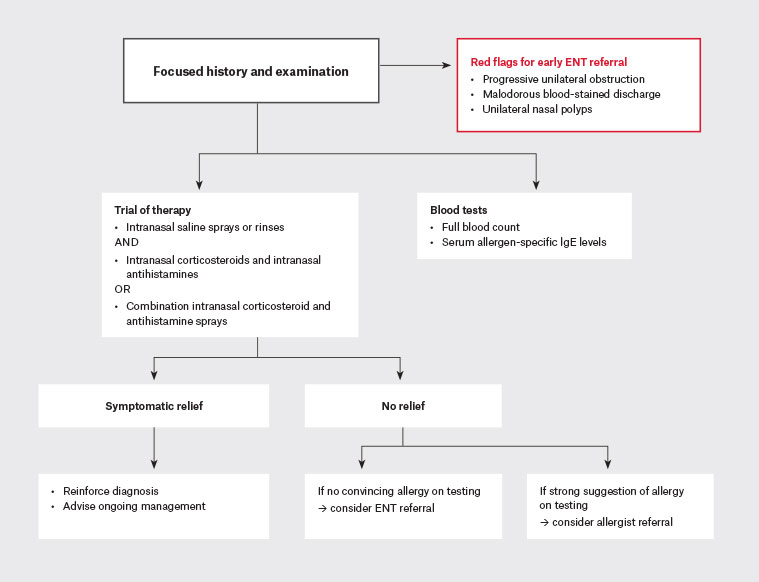
Figure 1. Flowchart of management for allergic rhinitis.
ENT, ear, nose and throat; IgE, immunoglobulin E.
Conclusion
AR causes debilitating symptoms for up to 19% of Australians, with significant effects on quality of life and function.3 An assessment in the primary care setting, with a targeted history, examination and panel of investigations, should be able to identify those with a significant burden of allergic disease. Radiological imaging is not part of the work-up for AR unless there is uncertainty regarding the diagnosis. Allergen avoidance, as well as treatment with intranasal saline, corticosteroids and antihistamines, might provide relief for the majority of those with AR. Combination corticosteroid/antihistamine sprays are highly effective and convenient and are increasingly considered a first-line therapy. The increased availability of prepackaged self-administered sublingual immunotherapies targeted towards dust mite and pollen allergies has made immunotherapy much more feasible and convenient. Referral to an allergist should be considered if specific allergen tests show significant airborne allergen sensitivity. Surgical referral is required if red flags are present, if significant anatomical obstruction exists or if there is inadequate response to medical management. Biological agents have an emerging role and might become part of the treatment paradigm in the future.
Key points
- Rhinorrhoea, postnasal drip, sneeze, nasal congestion and irritation are common symptoms.
- Serum specific IgE and skin testing help diagnose allergic rhinitis.
- Imaging does not play a role in the diagnosis.
- Combination intranasal corticosteroids and antihistamine sprays are a new and effective treatment.
- Immunotherapy has a well-established role in therapy, with self-administered wafers now available on prescription for dust mite and grass pollens.