A watery eye is a common presentation that might perplex the primary care physician with a wide range of differential diagnoses and varying acuity. Epiphora refers to eye watering that involves a distinct overflowing of tears down the face, and typically points to lacrimal outflow obstruction.
A distinction is made between true epiphora and the watery eye that instead presents with tear welling; the latter being more suggestive of reflex tear production following ocular surface stimulation.1 Excess tear production is usually reactive and, rarely, can occur as a result of primary hypersecretion. Common causes of reflexive lacrimation include dry eye, blepharitis, foreign bodies and eyelid malposition.
Impaired drainage can result in tear pooling, and might result from lid malposition, as seen in ectropion and entropion, or be due to blockage anywhere along the nasolacrimal duct from puncta to the intranasal opening.2
The watery eye has vast differential diagnoses, and it is important to consider the diversity of causes across different patient populations. Paediatric glaucoma, for example, is important to consider given its significant treatment implications for the patient if left unmanaged. Common causes of epiphora and the watery eye are outlined in Table 1.3
| Table 1. Causes of epiphora |
| General |
Causes |
| Reflex tear production |
- Eyelash malposition – trichiasis, distichiasis
- Blepharitis/meibomian gland dysfunction
- Conjunctivitis – allergic, viral, bacterial
- Foreign body
- Dry eye
- Keratitis
- Uveitis
- Angle-closure glaucoma
|
| Reduced tear outflow |
Lid malposition
- Entropion (in-turned eyelid)
- Involutional
- Cicatricial
- Spastic
- Congenital
- Ectropion (out-turned eyelid)
- Involutional
- Cicatricial
- Mechanical
- Paralytic
- Congenital (rare)
- Floppy eyelid syndrome
Punctal stenosis
Nasolacrimal duct obstruction
- Iatrogenic – rhinoplasty, sinus surgery
- Traumatic – facial fractures, canalicular involving lid lacerations
- Sinusitis
- Systemic inflammatory conditions
- Neoplastic
|
| Paediatric specific |
- Ophthalmia neonatorum (neonatal conjunctivitis)
- Congenital glaucoma
- Punctal atresia
- Congenital nasolacrimal duct obstruction
|
Aim
This article aims to review potential causes of the watery eye, discuss its work-up with helpful adjuncts, and provide a framework for its systematic assessment and management in the primary care setting.
Anatomy and drainage
An understanding of the lacrimal apparatus and tear drainage system might help clarify how epiphora arises (Figure 1). Tears are primarily produced by the lacrimal gland, which resides in the superolateral aspect of the globe.4 Tears are produced as a combination of a baseline rate of secretion as well as a reflex following stimulation of the optic nerve (light reflex) or trigeminal nerve (touch reflex).5 After coating the ocular surface, contraction of the orbicularis oculi muscle assists with fluid drainage through the upper and lower puncta of the eyelids and into the upper and lower canaliculi.4 The upper and lower canaliculi then join to form a common canaliculus, which, in turn, drains into the lacrimal sac.4 The lacrimal sac lies lateral to the nasal cavity and is connected by the nasolacrimal duct to the nose through Hasner’s valve.4 Obstruction at any point along this pathway can impair drainage and lead to a watery eye.
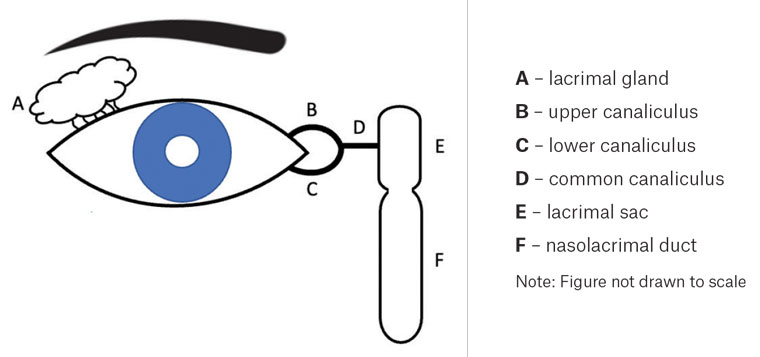 Figure 1. Anatomy and drainage pathway of the lacrimal system.
Figure 1. Anatomy and drainage pathway of the lacrimal system.
Assessment
History
A systematic history is important in the evaluation of the watery eye, and general questions regarding onset, duration, laterality of disease and pattern (constant or intermittent) should be noted.
Age at presentation is useful when considering likely causes. Congenital nasolacrimal duct obstruction is the most common cause of eye watering in patients aged less than four years, whereas issues such as lid malposition and dry eye disease might be considered in an older cohort.
A distinction might be made between acute or chronic presentations. Eye watering that has persisted over three months is considered chronic and usually implies the presence of lacrimal outflow obstruction in an otherwise normal examination.
Ocular symptoms should be explored, and patients should be asked about any visual changes including diplopia and reduced visual acuity.1 The presence of crusting or any discharge should be noted. Tear colour might be altered in some patients, in addition to the presence of any blood or purulent discharge. A history of ocular trauma or previous ocular/periocular surgery should also be enquired.1,6
A clear sinonasal history should also be taken for patients with undifferentiated epiphora, including rhinorrhoea, nasal obstruction or anosmia. Laterality is important when considered in conjunction with patients’ ocular symptoms, and unilateral epistaxis should be explored to rule out a potential sinonasal mass.7 A history of any previous sinonasal surgery and trauma is also essential, given the risk of nasolacrimal obstruction.1
Examination
A well-rounded nasolacrimal examination can be performed without a slit lamp and should commence with a thorough general inspection of the face. Obvious facial asymmetry or palsy should be noted, in addition to the presence of eyelid malposition (ectropion or entropion).8 The presence of any ingrown lashes, eyelid masses, poor lid closure or any other periorbital anomaly should be considered.
An eye examination should then follow, starting with visual acuity and an assessment of extraocular movements. Lid position should be assessed for ectropion causing reduced tear drainage or entropion causing ocular surface disease and reflex tearing.1 Access to slit-lamp examination can be limited in the general practice setting, but use of a direct ophthalmoscope with a blue filter can be useful in identifying obvious corneal pathology such as keratitis, foreign bodies and dry eye. Clinics equipped with a tonometer might consider measuring intraocular pressure, which, when elevated, might suggest the presence of intraocular inflammation or acute angle closure glaucoma as a cause of reflex tearing.
Fluorescein dye is reasonably accessible and can offer helpful information regarding tear drainage and corneal abnormalities. A dye disappearance test can assist with visualisation of tear drainage and the residual tear lake.1,9 Fluorescein is instilled to the inner aspect of the lower lid, and the eye is reinspected after five minutes to assess for any excessive dye in the tear film. This may be assessed with a blue-filter light, although any bright light source should adequately highlight residual dye. The presence of residual fluorescein suggests failure of appropriate drainage due to nasolacrimal obstruction, and is thus considered a positive test. It should be noted that patients with blepharospasm or strong blinking might disrupt the tear film, and thus prevent accurate interpretation.1,9
A sinonasal examination should be considered in patients with history concerning for nasal causes of epiphora.10 Inspection of the nose should be performed to describe any obvious nasal bone or septal deformity and is helpful in the setting of recent trauma, fracture or surgery. Anterior rhinoscopy should follow and can be performed with an otoscope to further assess for septal deviation, turbinate hypertrophy, nasal polyps or any other obvious mass lesion within the nasal cavity.1 Flexible nasoendoscopy is a helpful adjunct to examination, although the patient might require referral to an ear, nose and throat (ENT) specialist service.
Due to variable access to specialised equipment, particularly in rural and remote settings, it is understandable that some of the aforementioned ancillary investigations might not be possible to perform in a primary care setting. In such cases, liaison with the local optometry, ophthalmology or ENT service might be advised.
Investigations
Imaging is not routine in the primary care work-up of all epiphora and is preferably organised on the advice of a specialist ophthalmologist.1 Computed tomography (CT) of the orbits might help assess suspected traumatic, mechanical, sinonasal or neoplastic causes of nasolacrimal obstruction.11 Other adjuncts such as magnetic resonance (MR) imaging and dacrocystography have limited application in the primary care setting, and the patient should be referred to an ophthalmologist for consideration.1,12,13
Blood tests are not routinely organised and also have a limited role in the primary work-up of the watery eye. Primary autoimmune or inflammatory causes of epiphora are rare, and inflammatory markers should only be considered at the advice of an ophthalmologist, or if there is an otherwise strong suspicion of an underlying systemic inflammatory condition.1,14
Conjunctival swabs should be considered if there is suspicion of conjunctivitis; however, this typically presents with acute ocular discharge rather than true eye watering.15 If taken, swabs should at least include herpes simplex, varicella–zoster virus and adenovirus, whereas swabs for Chlamydia trachomatis and Neisseria gonorrhoeae should also be performed if there is significant concern for a sexually transmitted infection, with urgent referral to an ophthalmology service.
Management
First-line management
Although definitive management for epiphora can only be instituted once its underlying aetiology is confirmed, some treatment can be initiated in the primary care setting in the interim.
If the suspected cause is reactive secondary to ocular surface disease, such as dry eye disease, treatment can be initiated in a general practice setting but should be referred to an optometrist for ongoing management due to complexity of disease.16,17 Preservative-free lubricants four-times daily can be initiated with or without chloramphenicol ointment depending on severity.
Warm compress, gentle eyelid massage and lid hygiene should be suggested for patients with suspected blepharitis or meibomian gland dysfunction. A cotton bud or pad dipped in a dilute solution of baby shampoo might be utilised to gently cleanse the lid and lash line twice a day.
Patients with suspected rhinosinusitis or allergy should be commenced on intranasal topical corticosteroids, either in conjunction with an antihistamine orally or as a combined spray.1
Escalation to a specialist otolaryngologist should be considered in patients with obvious sinonasal symptoms, or by the involved ophthalmologist.
Paediatric epiphora
The management of paediatric epiphora differs and should always be conducted alongside consultation with the ophthalmology service. Due to sight and life-threatening implications of ophthalmia neonatorum (neonatal conjunctivitis) secondary to chlamydia or gonorrhoea,15 neonates aged under one month should be discussed with an ophthalmology service to arrange urgent review. Similarly, children with suspected congenital glaucoma who present with signs of buphthalmos (a bulging eye) or photophobia should be urgently discussed with an ophthalmology service.17 Children with nasolacrimal duct obstruction without red flags, such as those outlined above, can be managed with lacrimal massage and lid cares until non-urgent review with an optometrist or ophthalmologist can be arranged.18 The vast majority of infants who present with congenital nasolacrimal duct obstruction will have spontaneous resolution of their symptoms.
Surgical management
Surgical management might be considered following discussion with a specialist ophthalmologist or ENT surgeon. Type of intervention varies depending on the underlying cause of epiphora. Examples of surgical procedures that might be considered include ectropion or entropion repair, and dacryocystorhinostomy (DCR).1,19 Patients with eyelid malposition, punctal ectropion and eyelid laxity should be referred to the oculoplastics service for consideration of surgical correction. DCR involves the formation of a fistula from the lacrimal sac to the nasal mucosa and can either be performed via an external approach or endoscopically in conjunction with an ENT surgeon.1,19,20
Common causes
Reflex lacrimation
Reflexive lacrimation can occur as a result of a multitude of stimuli, including but not limited to: dry eye disease, blepharitis, foreign bodies and eyelid malposition. Onset is typically seen in an older demographic of patients, with management typically involving a trial of lubricants and correction of the underlying irritative stimuli.
Nasolacrimal duct obstruction
Nasolacrimal duct obstruction (NLDO) should cause a true tearing epiphora that lasts over at least three months. Patients’ symptoms can be either uni- or bilateral, and will usually present with an otherwise normal examination. Intervention for NLDO, on failure of first-line management with lubricants and warm compress, might require surgical management. Surgery would aim to correct the underlying cause of obstruction and maintain duct patency, to prevent secondary complications including mucocoeles and dacryocysitis. Patients should be referred if their symptoms significantly impact their day-to-day activities.
Facial palsy
Facial nerve palsy might cause both true epiphora and reflex lacrimation through respective lacrimal pump failure and subsequent drying of the ocular surface. Management normally involves at least lubricating the eye, while trying to identify and reverse any underlying cause of facial nerve dysfunction. Permanent paralysis might require more definitive surgical correction and protection of the ocular surface, which can be achieved through surgical means of tarsorrhaphy, gold weight insertion or other forms of surgical facial re-animation.8
Eyelid malposition
Eyelid malposition can lead to reflex lacrimation from both ocular surface drying and corneal injury. This can normally be addressed with lubrication in the first instance. Forms of malposition, including entropion, ectropion, excessive eye laxity or Floppy eyelid syndrome, do respond well to surgical correction and should be considered for referral to an oculoplastics service.
Conclusion
The watery eye is a common presenting complaint for primary care practitioners. A good understanding of the presenting symptoms and signs of epiphora is essential in differentiating between its various causes, and will help guide clinicians in its appropriate investigation, management and escalation in the general practice setting. Early involvement of an optometrist might assist in the triage and delivery of multidisciplinary care for cases with preserved vision. Significant loss of visual acuity warrants direct consultation with an ophthalmology service.
Key points
- The differential diagnoses for epiphora is broad, and a systematic history and examination is crucial in its assessment.
- Both ocular and sinonasal causes should be considered in the patient with undifferentiated epiphora.
- A fluorescein-assisted eye exam can be a simple but helpful ophthalmoscopic adjunct.
- Most causes of paediatric nasolacrimal duct obstruction can be managed with lacrimal massage and lid cares in the absence of any red flags signs or symptoms.
- A multidisciplinary team for the patient with epiphora should ideally involve the primary care clinician, optometrist, ophthalmologist and an otolaryngologist.