Australia is experiencing a growing burden of hip and knee osteoarthritis and subsequent joint replacement.1,2 In 2021, over 41,000 total hip replacement (THR) and over 59,000 total knee replacement (TKR) procedures were performed nationally.2 By 2030, the incidence of THR and TKR in Australia could exceed 79,000 and 161,000, respectively.3
Although THR and TKR are highly successful procedures for patients with end-stage osteoarthritis, they are not without risk.4,5 Prosthetic joint infection (PJI) is a devastating complication, carrying significant morbidity for the patient and substantial economic cost to the healthcare system.6 Infection is the most common reason for revision of primary THR and TKR in Australia, representing 22.7% and 26.6% of all revision procedures performed, respectively.2 The Australian incidence of PJI is estimated to be 3900 cases annually, with yearly costs exceeding $50 million.7
With increasing demand being placed on finite health budgets, improving efficiency in healthcare, minimising complications and reducing unnecessary costs are vital.8 Modifiable risk factors, such as smoking, poorly controlled diabetes and excessive body mass index (BMI) increase the risk of PJI following THR and TKR.6,9 Although restricting access to joint replacement in the setting of modifiable risk factors is controversial,10 interventions to address them preoperatively have been shown to improve outcomes and reduce costs.11,12
A 2021 survey of the Arthroplasty Society of Australia (ASA) found that 91% of orthopaedic surgeons who responded restrict access to THR and TKR in the setting of modifiable risk factors.13 This study surveyed Australian general practitioners (GPs) regarding their perceptions and management of smoking, poor diabetic control and excessive BMI in patients with end-stage hip and knee osteoarthritis prior to joint replacement.
Methods
The survey tool used in the ASA study was modified for use with a GP audience and was piloted by six GPs with experience in managing hip and knee osteoarthritis.13 The final tool included two demographic questions, three clinical questions and an optional, free text question (Appendix 1). No identifiable data were collected. The survey was administered via Qualtrics XM (Seattle, Washington), an online survey platform. Invitations to complete the survey were widely distributed to Australian GPs via Primary Health Networks, University GP departments and GP Facebook groups. The survey remained open from 1 February–31 March 2023.
Statistical analysis of results was performed using Microsoft Excel (Redmond, Washington). Descriptive statistics (counts and proportions) were used to present the main findings. Ethics approval for the study was granted by the Darling Downs Health Human Research Ethics Committee (LNR/2021/QTDD/82223) and ratified by The University of Queensland Research Ethics and Integrity Department (2022/HE000211).
Results
A total of 131 survey responses were received. Respondents had a range of clinical experience: 34% (44/128) had been GPs for less than 10 years; 25% (32/128) had been practising for 10 to 20 years; and 38% (48/128) had over 20 years’ experience. Four responses (3%) were received from GP registrars. There were 56 responses (44%) from metropolitan GPs and 72 responses (56%) from rural GPs.
Most respondents attempted to modify risk factors prior to referring a patient with symptomatic hip or knee osteoarthritis to see an orthopaedic surgeon. Over 90% (111/123) attempted to address current smoking; 94% (116/123) attempted to improve diabetic control; and 89% (109/123) tried to reduce excessive BMI prior to referral. Specific HbA1c (glycated haemoglobin) and BMI targets are presented in Figure 1.
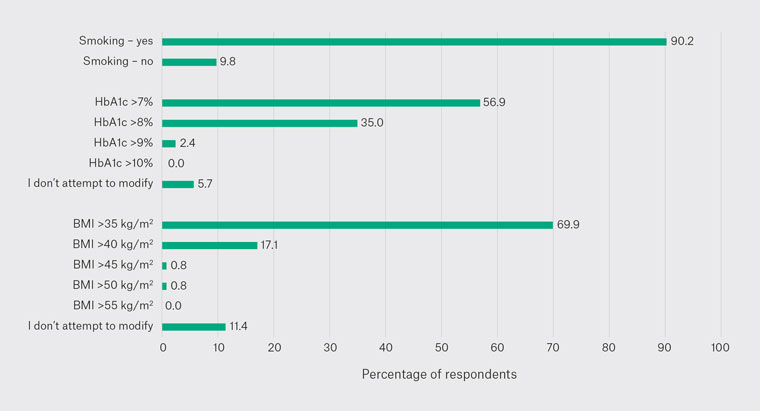
Figure 1. Responses to the question, ‘Prior to referring a patient with symptomatic hip or knee osteoarthritis to see an orthopaedic surgeon, do you attempt to modify the following risk factors?’
BMI, body mass index; HbA1c, glycated haemoglobin.
Regarding timing of surgery, most respondents felt that it was appropriate for patients to have their hip or knee replacement delayed until risk factors had been modified. For current smokers, 57% of GPs (68/120) thought that surgery should be delayed until cessation; 84% (101/120) felt that diabetic control should be optimised preoperatively; and 74% (89/120) responded that surgery should be delayed until patients had reduced their BMI. Specific HbA1c and BMI targets are presented in Figure 2.
However, many GPs did not believe that modifiable risk factors were absolute contraindications to hip or knee replacement. Over 76% of respondents (90/118) did not feel that current smoking was a contraindication; 46% (54/117) did not think that poor diabetic control precluded surgery; and 43% (51/118) did not believe that excessive BMI was a contraindication to joint replacement. For respondents who did believe that these risk factors were contraindications, specific HbA1c and BMI thresholds varied (Figure 3).
Overall, 47 GPs provided comments in the optional, free text question. A common theme was the challenge primary healthcare providers faced trying to address modifiable risk factors, in particular excessive BMI. A lack of referral pathways for morbidly obese patients, particularly in the public sector, was identified. Several GPs commented that using strict ‘cut-offs’ for surgery was inappropriate; others suggested that if patients had made a significant effort to reduce their BMI but were still morbidly obese, they deserved to undergo joint replacement. In contrast, three respondents stated that health service-imposed restrictions were beneficial in their efforts to assist patients to modify risk factors.
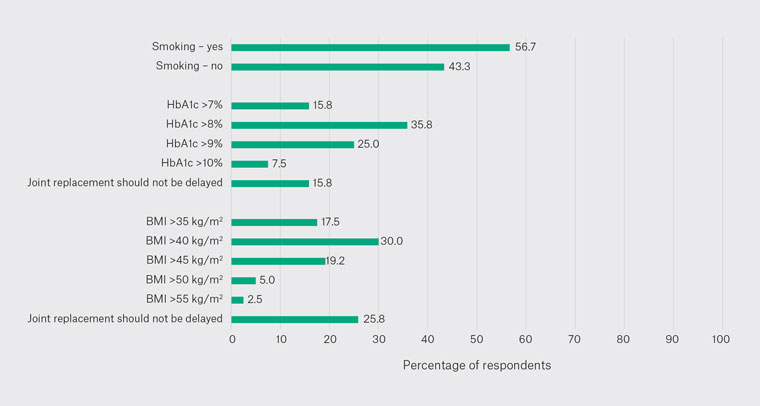
Figure 2. Responses to the question, ‘Do you think that patients should have their hip or knee replacement delayed until the following risk factors have been modified?’
BMI, body mass index; HbA1c, glycated haemoglobin.
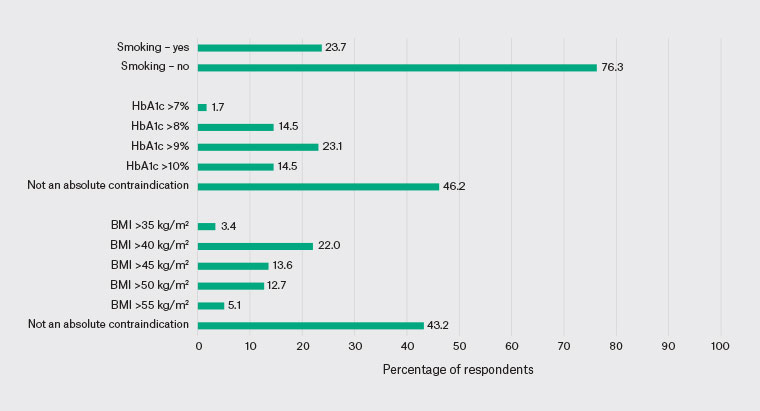
Figure 3. Responses to the question, ‘Do you think that the following risk factors are absolute contraindications to hip or knee replacement?’
BMI, body mass index; HbA1c, glycated haemoglobin.
Discussion
The results of this study suggest that Australian GPs are aware of the significance of modifiable risk factors in patients with end-stage hip and knee osteoarthritis requiring joint replacement. Most respondents attempted to address current smoking, poor diabetic control and excessive BMI prior to referral to an orthopaedic surgeon. Similarly, most GPs surveyed felt that joint replacement should be delayed until modifiable risk factors had been addressed. However, many did not believe that current smoking, poor diabetic control or excessive BMI represented absolute contraindications to THR or TKR.
In 2021, a similar survey was distributed to the membership of the ASA, a subspecialty group of the Australian Orthopaedic Association (AOA).13 Responses were received from 77 of the 121 members, representing a response rate of 64%. Most respondents were experienced, high-volume joint replacement surgeons. Overall, 91% of surgeons restricted access to THR or TKR in patients with modifiable risk factors. The majority (72%) employed a BMI threshold in their practice, although specific cut-offs varied. BMI thresholds of 40, 45 and 50 kg/m2 were used by 34%, 15%, and 21% of respondents, respectively. Most respondents (85%) did not offer joint replacement to patients with poorly controlled diabetes, and nearly half (46%) restricted access to current smokers. A comparison of Australian surgeons’ and GPs’ responses is presented in Table 1. An earlier survey of the American Association of Hip and Knee Surgeons (AAHKS) found that American surgeons were more restrictive than Australian surgeons in all domains.14
| Table 1. Proportion of surveyed Australian arthroplasty surgeons who restricted access to joint replacement in the setting of modifiable risk factors compared to the proportion of surveyed Australian GPs who felt that these risk factors were absolute contraindications to joint replacement13 |
| Modifiable risk factor |
Surgeons (%) |
GPs (%) |
| Excessive body mass index |
71.8 |
56.8 |
| Poor diabetic control |
84.5 |
53.8 |
| Current smoking |
46.5 |
23.7 |
When comparing the results of the present study and the ASA study, it is interesting to note that Australian orthopaedic surgeons are more conservative in offering joint replacement to patients with modifiable risk factors than referring Australian GPs believe is appropriate. The discrepancy in these findings might be explained by a lack of universally accepted guidelines for the management of modifiable risk factors.
As far as we are aware, only one previous study has investigated GPs’ perceptions of modifiable risk factors in patients undergoing joint replacement. In 2011, Wright et al reported the results of a survey of orthopaedic surgeons and referring physicians (family physicians and rheumatologists) in Ontario, Canada, regarding indications for TKR.15 In total, 135 surgeons, 165 family physicians and 111 rheumatologists responded to the survey, representing response rates of 67%, 36% and 79%, respectively. Respondents were asked how 34 different patient characteristics, one of which was obesity, affected their decision to either perform a TKR or refer a patient for TKR. Overall, 42% of surgeons stated that they were less likely to perform a TKR in an obese patient, and 2% felt that obesity was a contraindication to TKR. Similarly, 48% of referring physicians stated that they were less likely to refer an obese patient for a TKR and none felt that obesity was a contraindication to TKR. Interestingly, obesity was one of only two patient characteristics (out of 34 in total) where surgeons and referring physicians agreed on the influence it would have on their decision making.
There has been a dramatic increase in the incidence of global obesity since 1975.16 Nearly one-third of Australian adults are obese.17 Obesity is a known risk factor for the development of hip and knee OA and the subsequent need for joint replacement.18,19 Obesity, and in particular morbid obesity (BMI ≥40 kg/m2), increases the risk of PJI and other postoperative complications for both THR20 and TKR.21,22
Obesity and type 2 diabetes mellitus (T2DM) often co-exist.23 Approximately one million Australians (4.1%) have T2DM, and this figure has increased from 3.3% in 2001.17 Patients with T2DM are at higher risk of PJI and other postoperative complications following joint replacement.24,25 However, good diabetic control reduces these risks.26 The Royal Australian College of General Practitioners’ guidelines recommend a glycated haemoglobin (HbA1c) of ≤7% (≤53 mmol/mol) in patients with T2DM.27
Despite ongoing public health messaging about the detrimental effects of smoking, 2.6 million adult Australians (13.8%) continue to smoke tobacco daily.17 Smoking increases the risk of PJI and other postoperative complications following THR and TKR.28,29
Restricting access to joint replacement in the setting of modifiable risk factors is controversial.10 Taking morbid obesity as an example, restricting joint replacement to patients with a BMI <40 kg/m2 would prevent one major complication but would deny 14 patients from having a successful, complication-free procedure.30 Obese patients have similar improvements in patient-reported outcome measures following THR and TKR compared to non-obese patients, albeit from lower baselines.2
However, structured interventions to address modifiable risk factors preoperatively have been shown to reduce complications and costs associated with joint replacement. In implementing a preoperative optimisation protocol, screening for 19 specific risk factors, Bernstein et al demonstrated reduced hospital length of stay (LOS) and reduced costs for patients undergoing THR and TKR.11 Similarly, by instituting a preoperative risk factor optimisation protocol, focusing on 16 different risk categories, Dlott et al found a reduction in LOS, improved rate of home discharge, and reduced 30- and 90-day emergency department presentations following THR and TKR.12 The risk factors screened for in these two preoperative optimisation protocols are presented in Table 2. Recommended targets for the modifiable risk factors in this study were included in Wall and de Steiger (Table 3).9
| Table 2. Previously published preoperative optimisation protocols for patients undergoing total hip and knee replacement11,12 |
| Risk factors screened for by Bernstein et al11 |
Risk factors screened for by Dlott et al12 |
| Complete blood count |
Allergies |
| Haemoglobin |
Medical history |
| Comprehensive metabolic panel (Chem-12) |
Infection risk |
| Prothrombin time/internationalised normalised ratio |
Smoking |
| Haemoglobin A1c |
Obesity |
| Methicillin-resistant Staphylococcus aureus screen |
Malnutrition |
| Electrocardiogram |
Cardiovascular disease |
| Body mass index |
Venous thromboembolism |
| Modified risk assessment and prediction tool |
Neurocognitive compromise |
| Deep vein thrombosis prophylaxis evaluation |
Substance dependence |
| Depression screen |
(Suitability for) telerehabilitation |
| Anxiety screen |
Diabetes |
| Dental screen |
Anaemia |
| Obstructive sleep apnoea screen |
Systemic steroid use |
| Tobacco use |
Obstructive sleep apnoea |
| Lower extremity skin check |
Social support |
| Narcotic use |
|
| Cardiac records/results |
|
| Alcohol use |
|
| Table 3. Recommended preoperative targets for modifiable risk factors9 |
| Modifiable risk factor |
Recommendation |
| Obesity |
Aim for a BMI <40 kg/m2 prior to joint replacement |
| Diabetes mellitus |
Aim for a HbA1c of ≤53 mmol/mol (≤7%) prior to joint replacement |
| Tobacco use |
Aim for smoking cessation at least 4 weeks prior to joint replacement |
| BMI, body mass index; HbA1c, glycated haemoglobin. |
Our study has several strengths. As far as we are aware, this is the first study to investigate Australian GPs’ perceptions of modifiable risk factors for patients with end-stage hip and knee osteoarthritis requiring joint replacement. The survey tool was designed to facilitate comparison with results from the recent ASA survey.13 Improving joint replacement outcomes, minimising complications and reducing costs are critical, and it is hoped that the results of this study will stimulate ongoing discussion around this topic.
We also acknowledge several limitations of our study. Unlike the ASA study, we did not distribute the survey to all GPs in Australia, and we are unable to calculate the response rate.13 Although we attempted to distribute the survey widely, it is possible that the respondents were not representative of the entire Australian GP population. Metropolitan GPs were under-represented, and hence the results might not be generalisable. We did not define metropolitan or rural practice locations, and we acknowledge that there might be differences in the interpretation of these terms. In addition to the three modifiable risk factors included in the current study, the ASA study investigated other medical and behavioural risk factors known to influence the risk of complications following THR and TKR.13 We elected not to include these other risk factors to shorten the survey and improve the response rate.
Conclusion
The results of this study suggest that Australian GPs are mindful of modifiable risk factors in patients with hip and knee osteoarthritis. Most respondents attempted to address current smoking, poorly controlled diabetes and excessive BMI prior to referral to an orthopaedic surgeon, and they supported delaying surgery until these risk factors had been modified. However, many GPs did not support restricting access to joint replacement.