Peripheral arterial disease (PAD) has been reported to affect up to 10% of patients in Australian primary healthcare settings.1,2 Chronic limb-threatening ischaemia (CLTI) represents the advanced progression of PAD where patients experience ischaemic rest pain and/or tissue loss in the form of gangrene or ulceration.3 The prognosis for patients with CLTI is poor, with a mortality risk of least 20% in one year, and over 60% in five years.4–6 At one year, at least 30% of the patients would have undergone amputation.7
In order to avoid major amputation and manage ischaemic symptoms, patients with CLTI require revascularisation. Revascularisation surgery (open or endovascular) for patients with CLTI might be limited by patient-related factors such as significant comorbidities contributing to high surgical and anaesthetic risk, or disease-related factors such as multi-level atherosclerotic disease or extensive tissue loss making it technically not feasible for revascularisation. Despite surgical advances, some patients might have no revascularisation options or are unfit to undergo surgery. Even patients who have undergone revascularisation might not be pain free, or the tissue loss might be too extensive to recover. This subset of patients is known to have end-stage CLTI. The term ‘no-option’ CLTI is sometimes used, but it inaccurately suggests that treatment options are completely absent when in reality, there are still options to improve symptoms and quality of life.
For patients with end-stage CLTI, most interventions are aimed at symptom relief or to avoid major amputation. Patients remain at high risk of disease progression despite surgical intervention. Hence, end-stage CLTI should be considered a life-limiting albeit non-malignant condition requiring mixed models of care, where active treatment and palliative care is provided until either end of life or major amputation.8
The article offers a comprehensive review of strategies to address symptoms for patients experiencing end-stage CLTI who are not candidates for surgical revascularisation (open or endovascular) and are for conservative management only.
Symptoms of CLTI
Patients with end-stage CLTI present with progressive or longstanding severe rest pain or tissue loss in the form of gangrene or ulceration longer than two weeks. The primary goals of management are to maintain their quality of life by managing pain, providing good wound care to prevent further deterioration of ulceration and ideally aim to heal wounds, while also providing psychosocial support.
Management of end-stage CLTI
The management of end-stage CLTI requires a multidisciplinary team to create an individualised management approach for the patient. Each patient’s symptoms and the impact on their quality of life will present in different ways and will evolve over time, so management should adapt to these changes. Their comorbidities, functional status, social and financial circumstances, and access to specialised healthcare and rurality should be considered when formulating their management.
General consideration
For all patients, simple measures should be maximised, and risk factors optimised to help control symptoms and curb progression. As part of their assessment, risk factors including smoking, hypertension, diabetes and hyperlipidaemia should be identified and addressed as part of patient management. Exercise can be limited by claudication, frailty or previous amputations, but should be encouraged to promote collateralisation and maintain mobility. Pressure area care, appropriate footwear and bedding are key to protecting wounds and preventing formation of new ulcers, particularly in those with reduced sensation. Limitations to a patient’s mobility from pain or amputation might affect their need for additional support or aids at home and referral to community or allied health services.
Adequate nutritional intake is needed to support wound healing and improve overall health. There is a high prevalence of malnutrition and undernutrition being reported in patients with CLTI.9 Apart from encouraging healthy diets, screening and replacement of deficient micronutrients known to improve wound healing such as vitamins A, B, C and D, and zinc should be considered.10
Wound care
Patients with end-stage CLTI often have tissue loss requiring ongoing wound care in the community, which can be managed via community nursing services or wound clinics. The patient should be counselled that without adequate perfusion, it is challenging for a wound to heal. However, there has been a study showing wound healing with conservative management despite the presence of severe CLTI (and very low perfusion).11
Wound care for patients with end-stage CLTI should be person- and symptom- specific, with the goal of reducing discomfort from the wound and addressing any negative aspects of the wound such as itch, exudate, odour, bleeding and pain that increase discomfort (Table 1).12 Vascular wound nurse advice can be accessed by the general practitioner (GP) or directly from community nurses if there are any concerns with the dressing regimen or alternative recommendation (intolerance, cheaper alternative).
Adjunct therapies to wound healing
Appropriate wound care remains the priority for patients with ulceration due to CLTI; however, there are adjunct therapies with limited evidence of promotion of wound healing and amputation prevention that might be considered (Table 2).
| Table 1. Common wound-specific concerns for patients with end-stage chronic limb-threatening ischaemia |
| Concerns |
Recommendation |
| Pruritus |
- Wound itch can be due to significant unviable tissue burden leading to scratching, overgrowth of granulation tissue, maceration of wound edges, irritation from exudate, dermatitis or wound infection
- Encourage good skin care with hypoallergenic wash and moisturiser and avoid using hot water for cleaning
- Assess for contact dermatitis and eliminate allergens if identified. Consider a short course of topical corticosteroid (eg hydrocortisone) if evidence of ongoing dermatitis
|
| Exudate and transudate |
- Inflammatory response in chronic wound or infection can lead to significant exudate, which can damage peri-wound tissue and contribute to significant discomfort
- Assess for evidence of infection and manage as required
- The dressing should be absorbent and non-adherent to the wound. Depending on available resources, some dressing options are:
- foam dressing such as Allevyn™ (Smith and Nephew, Watford, England), Lyofoam™ (Mölnlycke Health Care, Gotherburg, Sweden)
- pad dressing such as Zetuvit® (Paul Hartmann Ltd, Heidenheim, Germany), combine dressing
- hydrofiber dressings such as Aquacel® (ConvaTec, London, England)
- hydroactive dressings such as Biatain™ (Coloplast, Humlebaek, Denmark)
- Advanced wound dressings such as negative pressure wound therapy (such as V.A.C® [KCI Licensing, Inc., San Antonio, USA] can sometimes be used to assist with exudate management and can assist with wound closure (particularly after surgical debridement). However, this should not be used for wounds with necrotic tissue or eschar
- Dressings for exudate management should aim at maintaining a moist wound environment while preventing excess exudate from coming into contact with surrounding skin as this leads to maceration and deterioration of the wound
- Barrier creams to protect wound edges and frequent dressing changes can prevent oversaturation
|
| Odour |
- Malodorous wounds in CLTI can be due to presence of necrotic tissue, colonisation of bacteria that release compounds (cadaverine and putrescine), infection or large volume exudate
- Assess for evidence of infection in the first instance
- Maintain good wound hygiene
- Consider debriding devitalised tissue to prevent further bacteria colonisation
- Managing exudates with appropriate dressing and consider dressing that contains charcoal or carbon that might help to reduce odour
|
| Gangrene, tissue loss and auto-amputation |
- Necrotic, devitalised tissues provide an optimal environment for bacterial growth
- Antiseptic products such as topical povidone-iodine; Inadine™ (Systagenix, Gargrave, UK) should be used to dry out gangrene and reduce bacterial burden
- In some cases of expected auto-amputation, patients and carers must be aware to monitor for the occurrence
|
| Pain |
- Chronic ischaemic wounds are often painful, which can be exacerbated by dressing changes. Pain with dressing changes is commonly due to dressings drying out and adhering to the wound base causing pain on removal. The wound bed might be packed too tightly or the physical act of wound cleaning might also cause pain. Pain can be minimised by:
- considering oral analgesia prior to dressing change. This will need to be prescribed with medication authority provided to community nurses
- minimising the frequency of dressing changes where possible
- For highly exudative wounds requiring frequent dressing changes, apply non-adherent dressing (eg Mepitel® [Mölnlycke Health Care, Gotherburg, Sweden]; Atrauman® [Paul Hartmann Ltd, Heidenheim, Germany], Jelonet [Smith and Nephew, Watford, England] as the primary dressing to the wound base, and only change the secondary absorbent dressing without the need to disturb the wound base
- Consider lidocaine-soaked gauze or topical lidocaine jelly to assist with painful dressing removal. This will need to be prescribed with medication authority provided to community nurses
|
| Fragile skin and pressure area, incidental injury |
- Patients with end-stage CLTI often have limited mobility and are at risk of developing pressure ulcers. Poor perfusion puts these pressure ulcers at high risk of becoming non-healing wounds. For leg or foot pressure care, consider:
- prevention of pressure area with a protective boot such as Z-flex heel boot at rest
- referral to a podiatrist for regular foot care and footwear advice to prevent new wounds due to poorly fitting footwear. Consider the use of a general practitioner management plan to document the patient’s individualised goals, coordinate the patient’s multidisciplinary care with team care arrangement, and assist the patient with the cost of allied health appointments.
- Patients with restricted mobility who require a wheelchair or who are unable to leave bed will be at risk of developing sacral and heel pressure sores. They might also be at risk of incidental injury during transfer, or from dressing application or removal. A comprehensive wound management plan should ensure that appropriate equipment is in place to prevent injury, and that high-risk areas are monitored regularly. This might require a team including occupational therapists, physiotherapists, wound care nurses and carers
|
| Table 2. Adjunctive therapies to wound healing |
| Hyperbaric therapy |
- Hyperbaric therapy involves the administration of a high concentration of pure oxygen to a patient in a sealed pressurised oxygen chamber (hyperbaric chamber) to increase the amount of oxygen dissolved in the bloodstream
- This aims to promote wound healing by enhancing tissue oxygenation, reducing inflammation and swelling, promoting angiogenesis and inhibiting bacterial growth3
- The role of hyperbaric therapy is adjunctive in wound healing and does not prevent major limb amputation3
- Non-medical hyperbaric therapy services exist in Australia; however, given the comorbidities of the patients with CLTI, patients should only be referred to medically supervised hyperbaric therapy providers
- Referrals can be made by the general practitioner to the hyperbaric medicine unit in each state. There is at least one public hyperbaric medicine unit within each state
|
| Topical oxygen |
- Topical oxygen can be administered directly to the wound using small pressurised medical devices purchased by the patient from a local distributor
- It can be delivered via a specialised interface (dressings) or as a chamber over the extremity
- The International Working Group for Diabetic Foot (IWGDF) guidelines recommend it to be used only if standard care has failed and resources are available to provide this intervention22
|
| Biologic and regenerative medicine therapies |
- Biologic and regenerative medicine therapy consists of gene therapy or stem cell therapy that aims to promote growth of new blood vessels (angiogenesis) in the extremities
- Preliminary safety and efficacy trial findings are promising for angiogenic therapies; however, efficacy has not yet been demonstrated in phase 3 trials
|
| CLTI, chronic limb-threatening ischaemia. |
Access to wound dressings and associated costs
In the community, wound care can be undertaken by community nurses or by attending general practice clinics. Unfortunately, there is limited Medicare funding for the management of chronic wounds, with no specific Medicare Benefit Schedule (MBS) item for consumables used in wound dressing. Historically, this cost would be borne by the patients and general practices. Silver-based dressings are particularly costly ($292 for five pieces of 10x10 cm dressing). For patients on home care packages, this extra cost affects the availability of funds for other essential services; hence, it is important to balance the clinical benefits with cost considerations to help mitigate the financial impact of wound care.
The incoming Chronic Wound Consumable Scheme (CWCS) is due to commence in Australia in mid-2025 and is designed to subsidise the expenses associated with wound consumables for eligible patients. This funding scheme will hopefully reduce the financial burden on eligible patients aged >65 years (or >50 years for Aboriginal or Torres Strait Islander Australians) as well as service providers.
Pain management
Pain is one of the most challenging symptoms for patients with end-stage CLTI and the impact on quality of life is comparable to that of advanced cancer patients.13 Management of pain relating to CLTI is challenging due to the complex underlying pain pathophysiology and coexisting comorbidities limiting therapeutic options. Additionally, many patients also have other underlying pathologies such as arthritis or venous insufficiency, which also contribute to pain. There should be realistic expectations of treatment, and the most appropriate therapy should be a personalised approach balancing efficacy and side effects. For those with complex or difficult-to-manage pain, palliative care or chronic pain services can be involved to guide management as it might be a life-long issue.
Pain associated with CLTI is often of mixed nociceptive, inflammatory and neuropathic origin, with complex interacting mechanisms making management of pain in CLTI challenging (Figure 1).14 Management generally requires multi-modal analgesia such as non-steroidal anti-inflammatory drugs (NSAIDs), anti-neuropathic agents and opioid therapy in conjunction with non-pharmacological pain management (Tables 3 and 4).
There has been increased interest in the use of cannabis in management of chronic pain; however, the role of cannabis in patients with end-stage CLTI is still to be determined, in particular noting that long-term cannabis users have an associated higher risk of PAD and incidence of acute limb ischaemia.15,16
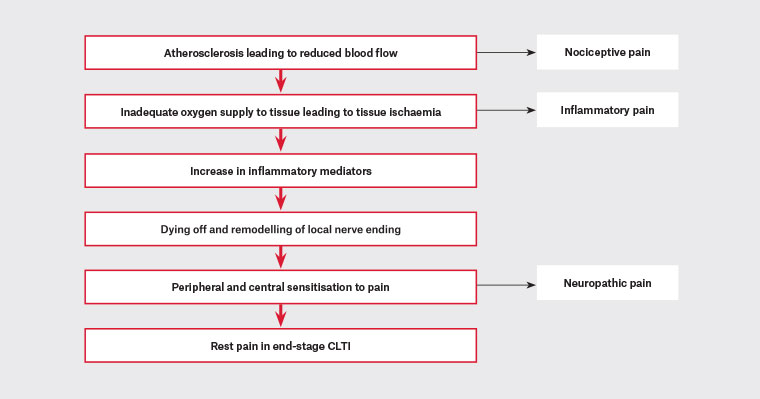
Figure 1. Physiology of pain in CLTI.14
CLTI, chronic limb-threatening ischaemia.
| Table 3. Non-pharmacological pain management |
| General advice |
- Some patients might find relief by positioning their legs in a dependent position (hanging their legs down over the end of the bed or allowing them to hang freely while seated)
- This position helps improve blood flow by taking the advantage of gravity; however, this might not be suitable for patients who are at risk of developing dependent oedema, which will contribute to worsening pain
- Patients might benefit from OT assessment for home care equipment such as recliner chairs or medical beds that can be adjusted to the position that can alleviate pain
|
| Compression therapy |
- For patients who are experiencing pain due to oedema, gentle low level compression therapy might be considered to improve venous return and reduce swelling in the affecting limb
- Compression therapy in this patient cohort requires careful consideration due to the risks of further compromising arterial blood flow
- Toe pressures and ABI should be performed prior to commencement of compression therapy and can be organised via an outpatient vascular clinic or radiology services with a vascular sonographer
- Tubigrip (elastic bandage) can be considered for patients with toe pressures <40 mmHg and not suitable for more aggressive compression therapy
- Intermittent pneumatic compression can also be considered (refer to vasomodulating therapy in Table 5)
- Additionally, close monitoring is required to detect any complications promptly, especially at the initiation of compression therapy
|
| CBT |
- CBT has not been widely studied in the management of pain in CLTI; however, it has an established role in the management of chronic pain23
- Integrating CBT into the treatment plan can be considered to minimise psychological factors that could further aggravate pain and improve adherence to medical treatment
|
| Complementary therapies |
- A variety of complementary therapies, such as meditation, yoga, music therapy, guided imagery and biofeedback, are frequently employed for chronic pain patients. Their efficacy in managing pain for individuals with CLTI lacks comprehensive research to advocate for their standard implementation
- Nonetheless, patients might reasonably contemplate these modalities to enhance their psychological welfare
|
| ABI, ankle-brachial index; CBT, cognitive behavioural therapy; CLTI, chronic limb-threatening ischaemia; OT, occupational therapist. |
| Table 4. Pharmacological analgesia regimen for patients with end-stage CLTI |
| Non-opioid agents
|
- These should be first line medication prescribed to all patients if there is no contraindication3
- It is crucial to discuss with patients the importance of having regular paracetamol for its opiate-sparing activity that might reduce adverse events and risk associated with high doses of opioids
|
|
Non-opioid agents
|
- Despite the inflammatory component of CLTI, prescribing NSAIDs must be undertaken with caution for this patient population
- Prescribing of NSAIDS requires close monitoring and only for a short period of time as they are known to be associated with gastrointestinal, cardiovascular and renal adverse events
- Patients with CLTI are often on ACE-I and aspirin for which co-prescription of NSAIDs could reduce their therapeutic effects while increasing risks of side effects
- The PRECISION trial demonstrated that a moderate dose of a COX-2 inhibitor, Celecoxib 200 mg, has lower rates of adverse events when compared to non-selective agents such as ibuprofen24
|
|
Adjuvant agents
- Anti-neuropathic agents such as gabapentinoids (pregabalin, gabapentin), antidepressants (amitriptyline, duloxetine)
|
- Patients with CLTI might experience significant neuropathic pain due to the neural damage from chronic ischaemia, in addition to other co-existing neurological damage such as diabetic neuropathy14
- Agents to reduce sensitisation due to nerve damage such as antidepressants (serotonin and noradrenaline reuptake inhibitors and tricyclic antidepressants, but not selective serotonin reuptake inhibitors) and gabapentinoids can be considered25
- Both gabapentin and pregabalin have been studied and shown to have a role in pain management, reduce opioid use and side effects in patients with CLTI
- Anti-neuropathic agents need to be prescribed with care for elderly patients, patients with renal failure or heart failure as it can contribute to peripheral oedema and worsening wound exudate26
|
Conventional opioids (immediate and extended release)
- Oxycodone
- Morphine
- Fentanyl
|
- The use of opioids should be avoided where possible. When used in isolation, they are rarely effective for ischaemic pain
- Studies have shown that opioids might diminish immune activation, reduce tissue oxygenation and angiogenesis and hence hinder wound healing27
- Doses should be titrated to effects, and available in short-acting and slow-release formulations
- There is a risk of opioid-induced hyperalgesia, abuse and dependence28
- Use is also limited by renal and hepatic comorbidities in patients with end-stage CLTI
- Therefore, prescription of opioid in this patient population must involve thorough assessment of risks against the benefits
|
- Atypical opioids
- Buprenorphine
- Tramadol
- Tapentadol
|
- If opioid analgesia is deemed required, consider prescribing atypical opioids
- Atypical opioids have demonstrated better efficacy in the treatment of ischaemic pain when compared with conventional opioids29
- Buprenorphine and tapentadol are noted to have better side effect profiles and are better tolerated in older patients compared to tramadol and conventional opioids
|
| ACE-I, angiotensin-converting enzyme inhibitors; CLTI, chronic limb-threatening ischaemia; COX-2, cyclooxygenase-2; NSAIDs, non-steroidal anti-inflammatory drugs; PRECISION, Prospective Randomised Evaluation of Celecoxib Integrated Safety Versus Ibuprofen or Naproxen. |
Vasomodulating therapies
In addition to or when pharmacological analgesic regimens remain inadequate, pharmacological or interventional therapies aiming to promote vasodilation can be considered with input from specialists (Table 5). Evidence for these interventions is limited.
If patients’ symptoms cannot be effectively managed in the community, it would be appropriate to refer them back to a vascular surgeon. This would allow for the evaluation of their condition, adjustment of pain management strategies and wound care regimen as necessary, and consideration of major limb amputation for those who might consider it.
| Table 5. Pharmacological and interventional vasomodulating therapy |
| CLS |
- CLS decreases pain by denervating lumbar sympathetic ganglia, which interrupts the pain pathway and neurolyse the nociceptive fibre3
- It also leads to vasodilation of the collateral circulation and shunting of blood through cutaneous arteriovenous anastomoses, which in turn assists with pain relief by improving tissue oxygenation
- These effects might be short-lived; however, due to the minimally invasive nature, CLS can be repeated29
- This is commonly performed by interventional radiologists
|
| SCS |
- Electrodes implanted into the lumbar epidural space are used to stimulate sensory fibres, which leads to vasodilation and improves microcirculation. It also suppresses sympathetic vasoconstriction and pain transmission3
- Spinal cord stimulators are being trialled, but its future in the management of end-stage CLTI remains uncertain at this stage and is greatly limited by cost, accessibility and complications
- Spinal cord stimulators are normally implanted by a neurosurgeon
|
| IPC |
- IPC involves the application of external pressure to the lower limbs using inflatable cuffs or sleeves, which intermittently inflate and deflate
- It promotes blood flow by increasing the arteriovenous pressure gradient and reversing vasomotor paralysis. It also promotes the release of nitric oxide, a potent vasodilator
- It is also effective in oedema management
- IPC can be hired via a lymphoedema clinic, vascular clinic or a medical equipment hire company
|
| Prostanoids such as prostaglandin E1 (Alprostadil), prostacyclin and iloprost |
- Prostanoids promote vasodilation via anti-thrombotic and profibrinolytic activities
- Prostanoids can be used selectively with input from vascular specialists for patients in whom revascularisation is not possible or has failed
- Agents such as iloprost require a 5-day, 6 hours per day intravenous infusion with strict monitoring as it is known to be associated with common side effects and should be used with caution for patients with ischaemic heart disease or heart failure
- There is limited evidence to support its routine use for rest pain relief30
|
| Vasoactive medications such as naftidrofuryl, pentoxifylline or cilostazol |
- There is very limited evidence to support the use of vasoactive medications in improving symptoms of end-stage CLTI
|
Topical vasodilators such as topical GTN or ISDN paste
or patch |
- Topical nitrates such as GTN or ISDN have local vasodilatory effects on vascular smooth muscles, which might lead to improvement in pain31
- Topical nitrates can be applied to limited areas of discoloured digits, or skin adjacent to dry gangrene
- Application of a large volume could lead to systemic absorption and cause unintended hypotension
- There has been evidence for use in vasopressor-induced digital ischaemia or meningococcal-induced digital ischaemia, but there is a lack of evidence in the treatment of CLTI
|
| CLTI, chronic limb-threatening ischaemia; CLS, chemical lumbar sympathectomy; GTN, glyceryl trinitrate; IPC, intermittent pneumatic compression; ISDN, isosorbide dinitrate; SCS, spinal cord stimulation. |
Major limb amputation
The need for amputation indicates the end of a limb and possibly the end of life.8
For patients who have intractable pain or a life-threatening infection, or who find long-term dressings intolerable, or the risk of complex revacularisation outweighs the benefit, major limb amputation (MLA) can be considered. Minor amputations (toes or forefoot amputations) are often futile given that without adequate perfusion, patients will likely experience ongoing pain and leave behind a larger non-healing wound. Nevertheless, some patients unwilling to accept long-term wound care or major amputation might require staged amputation as a physical or psychological bridge to major amputation.
The goal of MLA is to preserve quality of life and relieve symptoms due to CLTI; however, this is not without the risk of negatively impacting patients’ quantity and quality of life. It has been reported that more than 50% of patients who have undergone major limb amputation due to CLTI will die within five years.4,17 Mortality rates of up to 85% within five years have been reported in no-option CLTI elderly amputees.18,19 This has also been observed in a local study in New South Wales (NSW), Australia, where 28.3% of patients died two years following discharge from their primary CLTI procedures.20 Nevertheless, for patients who have good rehabilitation prospects, this might allow them to achieve an improved functional outcome. Multidisciplinary pre-amputation counselling is often helpful in these settings.
Patients will need to be counselled on the risks associated with surgery, including but not limited to perioperative cardiovascular events, reduced independence, phantom limb pain and risk of non-healing of amputation stumps. The psychological effect of MLA and its impact to their functional status needs to be considered by patients and care providers, and additional supports or aids might be required to assist them at home afterwards.
Psychosocial support
Living with severe CLTI can be mentally and emotionally challenging for patients and their carer(s). It is the key to caring for patients with end-stage CLTI to have
a good therapeutic relationship with a regular GP who has a thorough understanding of their goals and is able to coordinate their multidisciplinary care. Psychosocial support via counselling and referral to support groups or therapists familiar with care of patients with end-stage CLTI should be considered. Encourage carers to make regular appointments to ensure that their own psychosocial wellbeing and physical health are attended to as well.
Palliative approach to end-stage CLTI
CLTI is a progressive disease and prognostication is difficult. Patients with untreatable, no-option end-stage CLTI will deteriorate slowly over a period of time, or sometimes acutely due to wound infections, or due to other underlying comorbidities. Despite being palliative from a CLTI perspective, many patients with end-stage CLTI wish to pursue active treatment for their other medical conditions as they still maintain reasonable quality of life. Ongoing advanced care planning should occur.
Some patients might wish to pursue long-term suppressive antibiotics for infected wounds, acknowledging that it would be a temporising measure, and might lead to antibiotic resistance. It is encouraged for patients and families to have discussions about goals of care and advanced care planning in the event that patients deteriorate acutely. When appropriate, patients with end-stage CLTI should be linked in with palliative care services to ensure that their needs are being addressed.
If pain remains unmanageable despite the discussed management options, referral to chronic pain or palliative care services would be warranted. Early referral to these services (if available) is wise as CLTI pain will usually never resolve.
Social and cultural factors
Access to specialised healthcare and allied health input will be affected by the patient’s social circumstances and their location. Patients with CLTI typically have increased care needs in the community. For patients who are aged >65 years, comprehensive aged care assessment should commence early to ensure that patients receive adequate funding and the support they require to remain at home or should they require residential aged care. For younger patients, the National Disability Insurance Scheme (NDIS) can be considered to address these increased care needs. In rural or remote areas, there might be limited allied health, outpatient wound clinics or dressings available for patients, especially in community settings. Patients with limited mobility as a result of CLTI depend on family, friends or other services to attend appointments. This poses a challenge for those requiring regular dressing changes, as the frequency of appointments might be influenced by how often their transport is available. In all regions, the costs of expensive frequent dressings and poorly rebated regular appointments pose significant financial challenges for both the patient, the GP and the clinic/practice.
Healthcare practitioners need to consider a patient’s cultural and spiritual beliefs when managing CLTI. An open and culturally sensitive discussion is key, and should consider involving a suitable cultural liaison if appropriate and available. In Australia, First Nations people are more likely to have symptomatic CLTI and have higher rates of limb loss and major adverse cardiovascular events.21 Discussions regarding amputation should be sensitive to the spiritual connection between body and soul. Spiritual grief and loss can follow amputation as this connection is disrupted, and it is not uncommon for requests for amputated limbs to be preserved.
Conclusion
Management of end-stage CLTI is complex and GPs play a vital role in facilitating a patient-centred approach to their care, even in the absence of curative treatment. It involves a multidisciplinary approach and management should adapt to progressive symptoms over time.
Key points
- CLTI is a progressive disease where not all patients are suitable for revascularisation.
- Patients with end-stage CLTI have variable levels of symptom burden and impact on quality of life that requires individualised care in the community.
- Management requires a multidisciplinary team including community nurses, GPs and allied health services, with input from specialised vascular wound nurses (Figure 2).
- Pain management in patients with end-stage CLTI can be complex, and will require a multi-modal analgesic regimen and optimisation of non-pharmacological measures.
- Clear communication with patients and carers is important to manage expectations.
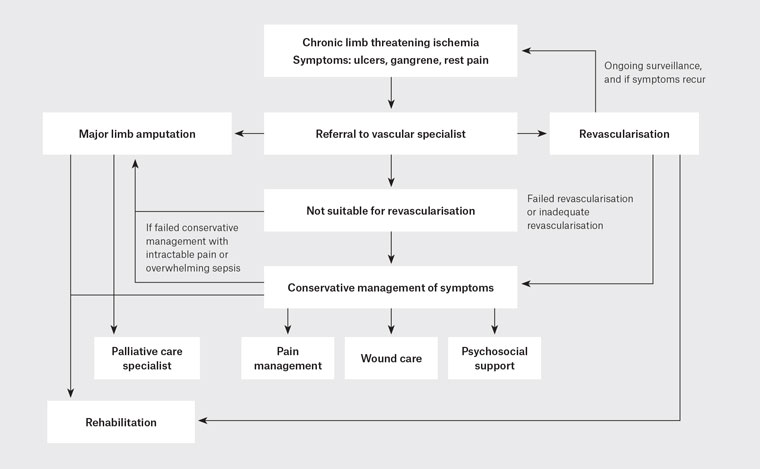
Figure 2. Flow diagram of management of end-stage chronic limb-threatening ischaemia in the community.