The COVID-19 pandemic accelerated the adoption of telehealth in primary care, significantly increasing services and market growth. Projections suggest that the global telehealth market might reach US$500 billion by 2030.1 This surge is particularly evident in commercial telemedicine services – defined here as direct-to-consumer (DTC) telemedicine. These services are characterised by predominantly virtual consultations through phone, video or messaging with medical practitioners that are marketed to, initiated by and mostly paid for by the consumer. There is usually no established doctor–patient relationship associated with these services, and they often feature strong marketing campaigns and cover a range of medical issues, from general consultations to specific treatments like weight loss or erectile dysfunction. Despite their rapid proliferation and significant market valuations, exemplified by US companies like Hims & Hers Health and Ro with valuations in the billions of dollars,2,3 research in this area has not kept pace. A similar pattern is observed outside the USA,4 with companies like Eucalyptus5 and InstantScripts6 in Australia and the rise and fall of Babylon Health in the UK.7
Existing research, mostly pre-pandemic, has looked at antibiotic use in acute respiratory infections (ARIs),8,9 contraception,10 hair loss11 and erectile dysfunction.12 Only a handful of studies have examined issues of accessibility,13 healthcare utilisation,14 clinician efficiency, and patient empowerment, satisfaction and preferences.15,16 There has not been a comprehensive review of the contemporary empirical literature on DTC telemedicine services within primary care. Furthermore, recent systematic reviews on the quality of telehealth consultations have either excluded this service group17 or focused on secondary or tertiary care settings.18
This review addresses this gap by identifying and assessing the nature and extent of the body of contemporary empirical research involving DTC telemedicine within primary care. We aimed to uncover knowledge deficits and propose areas for future research.
Methods
Protocol and registration
The reporting of this scoping review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist.19 The study protocol was registered with the Open Science Framework (osf.io/aw74p).
Search strategy
Three academic databases (MEDLINE, Embase and SCOPUS) were searched on 1 July 2023, for studies published from 1 January 2019 onwards. This five-year timeframe adequately captures the contemporary research in this field and the transition from pre- and post-COVID-19 periods. The search strategy utilised a combination of Medical Subject Headings (MeSH) terms and keywords to cover:
(1) telehealth or telemedicine; (2) primary care; and (3) the concept of DTC health services. The search strategy was devised in consultation with a university clinical librarian and in conjunction with published search strategies for telehealth.20 Table 1 shows a search strategy for MEDLINE.
| Table 1. Example search strategy for MEDLINE |
| Set |
Search statement |
| 1 |
exp Telemedicine/ or exp Remote Consultation/ or (cyberthera* or telecare or telecollaborat* or teleconsult* or teleconference* or teleeducat* or telediagnos* or telehealth or teleguide* or telediagnos* or telelearn* or telemed* or telementor* or telemonitor* or teleneurol* or teleopth* or telepediatric* or telepresence* or telerehab* or telerobotic* or telescreen* or teletherap* or teletransmi* or mhealth or “m heath” or ehealth* or “e health” or virtual or ((cyber or digital or remote* or distance* or tele) adj2 (care or collaborat* or consult* or conference* or educat* or diagnos* or health or guide* or diagnos* or learn* or med* or mentor* or monitor* or presence* or screen* or therap* or transmi*)) or ((cyber or digital or distance* or tele or remote* or sms or phone* or internet or “web based” or telephone* or texting or “mobile app*” or Instagram or Snapchat or Facetime or GMeet* or hangout* or Skype or Zoom or Web-ex or WebEx or Bluejeans or Facebook or e-mail* or email* or “e chat” or echat or “social media” or “text message*” or “answering machine*” or “voice mail*” or “video conferenc*” or “video link*” or “video chat*”) adj3 (consult* or support* or diagnos* or “follow-up*” or “health” or doctor* or “primary care” or clinic or clinics or clinician* or nurs* or psycholog* or therap* or intervention* or delivery))).mp. |
| 2 |
“direct to consumer*”.mp. |
| 3 |
DTC.ti,ab. |
| 4 |
or/2-3 |
| 5 |
and/1,4 |
| 6 |
limit 5 to English language |
| 7 |
limit 6 to year=”2019 -Current” |
Study selection criteria
Inclusion criteria
The inclusion criteria for this review were studies that:
- reported on DTC telemedicine services, being defined as a service providing predominantly virtual consultations with a medical practitioner for which the service was initiated by the consumer, and the main fee structure did not involve public funding or rebates
- reported research in the context of primary care settings
- reported on primary or secondary data
- were published from 2019 onwards
- were full text and published in English.
Exclusion criteria
The exclusion criteria for this review were studies that:
- reported on DTC telemedicine services provided by health providers other than medical practitioners (eg nurse practitioners, psychologists or physiotherapists)
- reported on DTC telemedicine services exclusively in secondary or )tertiary care settings
- reported on telehealth services provided by a traditional primary care health service, general practice clinic or hospital-based primary care service
- were non-empirical journal articles (eg reviews, protocols, editorials, conference proceedings, commentaries and letters)
- had no full text available.
Screening and data extraction
Reference details were downloaded into Endnote 20 and duplicates were excluded. References were then exported to Microsoft Excel and divided among the research team for title, abstract and full-text screening processes. To ensure consistency in screening, three reviewers (DF, SS and GD) independently reviewed 10% of the titles and abstracts and 10% of full-text articles during subsequent full-text screening.
Interrater reliability between the three reviewers was assessed to be sufficiently high during each stage with Cohen κ≥0.80. Iterative meetings were held to discuss
any discrepancies in screening decisions
that arose.
Data extraction was conducted using a customised form (Appendix 1). The form was piloted by each of the three reviewers with a subset of papers (n=5). Issues in consistency of data entry and usability of the template were discussed and modifications made accordingly. Key information extracted included article characteristics (authors, year and country), study design and method as defined by the Mixed Methods Appraisal Tool (version 18),21 modality of consultations, stakeholder group of focus, and specific population, condition and treatment of focus.
Data synthesis
The overall characteristics for each data extraction field were summarised as categorical variables. A narrative synthesis of the included articles was performed to identify primary focuses or themes of the research. The five themes identified were: (1) user characteristics and perspectives; (2) quality and safety; (3) healthcare utilisation; (4) health economics; and (5) validation of tools. There were some overlaps between articles that had more than one research domain of focus. The country of the corresponding author was coded by income classification based on the World Bank’s definitions of gross national income per capita per year.22
Results
Search results
Our initial searches retrieved a total of 689 records. After title, abstract and full-text screening, 44 (6.3%) papers met the inclusion criteria. Figure 1 demonstrates the inclusion and exclusion decision for papers at each stage of the screening process.
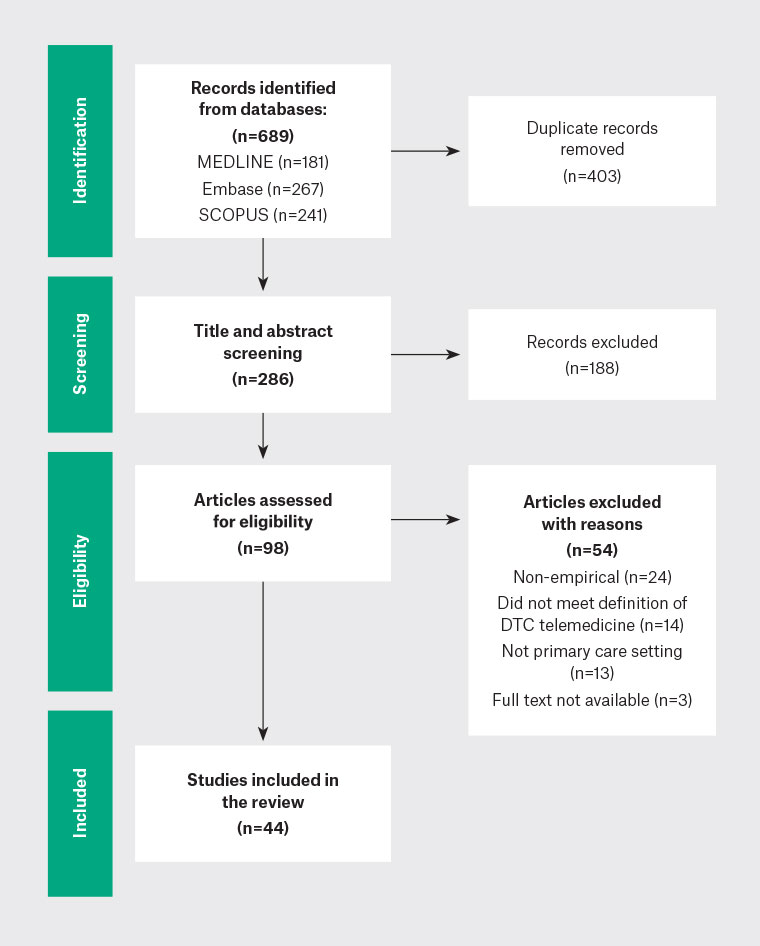
Figure 1. Inclusion and exclusion of papers at each stage of the screening process.
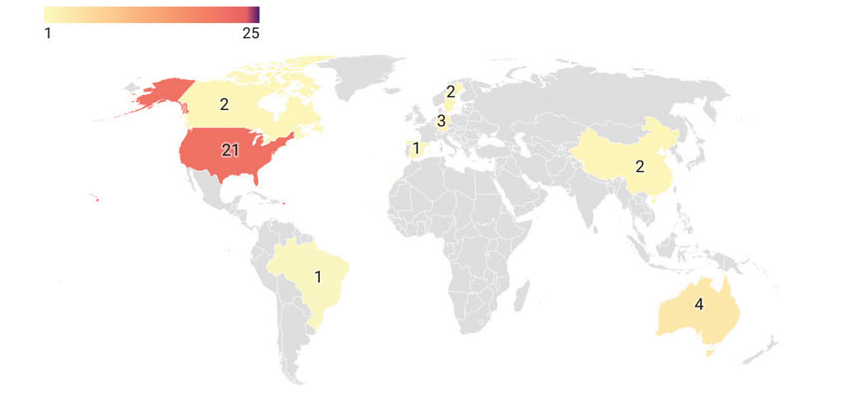
Summary characteristics of included publications
A summary of the key characteristics of the 44 included articles is presented in Table 2. Almost all studies were conducted in high-income countries (n=41, 93%), with most from the USA (n=29/44, 66%). The remainder of the articles were from Australia (n=4/44, 9%), Germany (n=3/44, 7%), Sweden (n=2/44, 4.5%), China (n=2/44, 4.5%), Canada (n=2/44, 4.5%), Spain (n=1/44, 2.3%) and Brazil (n=1/44, 2.3%). There were no publications from low-income countries. Figure 2 illustrates the geographical distribution of the included articles.
Most articles used quantitative methods (n=41/44, 93%), with the small remainder comprising two mixed methods studies (5%) and one qualitative study (2%). A large proportion of included articles were cross-sectional (n=26/44, 59%) and retrospective cohort studies (n=12/44, 27%), and the remaining were quasi-experimental studies (n=6, 14%). Cross-sectional studies were further classified into analytical (n=4/26, 15%) or descriptive studies (n=22/26, 85%). Overall, the cross-sectional studies focused on user characteristics and perspectives of a particular DTC telemedicine service,12,23–47 whereas the retrospective cohort and quasi-experimental studies focused on prescribing patterns, access to care and healthcare utilisation.8,11,48–63
| Table 2. Summary of key characteristics of included publications |
| Classification |
Papers
(N=44), n (%)A |
| Country of corresponding author |
|
| USA |
29 (65.9) |
| Australia |
4 (9.1) |
| Germany |
3 (6.8) |
| Sweden |
2 (4.5) |
| China |
2 (4.5) |
| Canada |
2 (4.5) |
| Spain |
1 (2.3) |
| Brazil |
1 (2.3) |
| Country income classification of corresponding author |
| High income |
41 (93.2) |
| Middle income |
3 (6.8) |
| Low income |
0 (0.0) |
| Study methods |
| Quantitative methods |
41 (93.2) |
| Mixed methods |
2 (4.5) |
| Qualitative methods |
1 (2.3) |
| Study design |
| Descriptive cross-sectional study |
22 (50.0) |
| Retrospective cohort study |
12 (27.3) |
| Quasi-experimental study |
6 (13.6) |
| Analytical cross-sectional study |
4 (9.1) |
| Modality: Synchronicity |
| Synchronous |
20 (45.4) |
| Asynchronous |
12 (27.3) |
| Both |
5 (11.4) |
| Not specified |
7 (15.9) |
| Modality: Technology |
| Video only |
15 (34.1) |
| Messaging based only |
12 (27.3) |
| Video and telephone and messaging based |
5 (11.4) |
| Video and telephone |
3 (6.8) |
| Telephone only |
2 (4.5) |
| Not specified |
7 (15.9) |
| Specific population of focus |
| All adults |
17 (38.6) |
| All patient groups |
11 (25) |
| Adult men |
6 (13.6) |
| Children or adolescents |
5 (11.4) |
| Adult women |
2 (4.5) |
| Clinicians |
1 (2.3) |
| Veterans |
1 (2.3) |
| Not specified |
1 (2.3) |
| Specific condition of focus |
| ARIs |
11 (24.4) |
| No specific focus |
9 (20.0) |
| Dermatological conditions |
8 (17.8) |
| Erectile dysfunction |
3 (6.7) |
| Contraception |
2 (4.4) |
| General paediatrics |
2 (4.4) |
| Hair loss |
2 (4.4) |
| UTIs |
2 (4.4) |
| ADHD |
1 (2.2) |
| Low acuity infectious diseases |
1 (2.2) |
| Men’s health |
1 (2.2) |
| Mental health |
1 (2.2) |
| Obesity |
1 (2.2) |
| Urgent care conditions |
1 (2.2) |
| Specific treatment of focus |
| No specific focus |
24 (54.5) |
| Antibiotics |
9 (20.5) |
| PDE5 inhibitors |
3 (6.8) |
| Finasteride or minoxidil |
2 (4.5) |
| Oral contraceptives |
2 (4.5) |
| Corticosteroids |
1 (2.3) |
| Non-stimulant ADHD therapies |
1 (2.3) |
| Oseltamivir |
1 (2.3) |
| OSH (Plenity) |
1 (2.3) |
| Research domain of focus |
| User characteristics and/or perspectives |
32 (55.0) |
| Quality and safety |
21 (36.0) |
| Healthcare utilisation |
3 (5.2) |
| Health economics |
1 (1.7) |
| Validation of tools |
1 (1.7) |
AColumns might not equal 44 due to overlap in some categories.
ADHD, attention deficit hyperactivity disorder; ARI, acute respiratory infection; n, number of articles included in descriptive analysis; OSH, oral superabsorbent hydrogel; PDE5, phosphodiesterase 5; UTI, urinary tract infection. |
Research domain of focus
Most articles (n=32/44, 72%) focused on user characteristics and perspectives. These articles tended to describe the patient, clinician or encounter characteristics for a particular DTC telemedicine service and might have included analysis of data regarding patient preferences, attitudes or perceptions. Some articles had more than one research domain of focus, resulting in some overlap. Twenty-one articles (47%) discussed some form of care quality and patient safety. Within this group, most of these articles analysed prescribing patterns (n=12/21, 57%),8,11,12,24,25,27,28,45,53,58,59,63 and the remainder assessed consult quality or patient satisfaction (n=9/21, 43%).26,29,30,39,42,48,49,57,61 Three articles (7%)37,52,56 considered healthcare utilisation and one article (2%)60 was a health economics approach describing a cost analysis comparison of DTC telemedicine versus traditional prescriptions of phosphodiesterase 5 (PDE5) inhibitors for erectile dysfunction. One article (2%)35 validated a checklist tool that was developed to assess the quality of skin lesion images submitted by consumers.
Modality of consultations
A large proportion of articles described services delivered using video (n=23/44, 52%), followed by messaging-based platforms (n=17/44, 39%) and telephone (n=10/44, 23%). There were some overlaps as some articles described services where multiple modalities were used. Any form of direct communication between the patient and the medical practitioner via a text-based message was categorised as using a messaging-based platform. This included messages via web-based applications, mobile phone applications or secure messaging platforms.
Specific populations of focus
One-third of articles involved specific populations (n=15/44, 34%), such as men (n=6/44, 14%)11,12,23,31,47,60 or women (n=2/44, 5%),8,34,40,43,44,54,62 children and/or adolescents (n=5/44, 11%)8,43,44,54,62 or veterans (n=1/44, 2%).61 A single study (2%) examined clinicians rather than a patient group, investigating the relationship between consultation length and quality using standardised patients.26 The remainder were articles that generalised to an adult population (n=17/44, 39%) or did not specify who the population was (n=1/44, 2%).
Specific conditions and treatments of focus
There were 13 specific conditions or condition groups of focus identified across 35 articles (80%), whereas the remaining nine (20%) had no specific disease or condition focus. There was a small amount of overlap, with one article investigating both ARIs and urinary tract infections (UTIs).25 The predominant condition group of focus was ARIs (n=11/44, 25%),8,24,25,27,28,45,53,54,56,62,63 followed by dermatological conditions (n=8/44, 18%),26,33,35,36,46,48,49,57 general paediatrics (n=2/44, 5%),43,44 low acuity infectious diseases in addition to ARIs (n=1/44, 2%),58 men’s health (n=1/44, 2%),31 mental health (n=1/44, 2%)30 and urgent care conditions (n=1/44, 2%).41
The predominant condition was erectile dysfunction (n=3/44, 7%),12,47,60 followed by contraception (n=2/44, 4%),34,40 hair loss (n=2/44, 4%),11,23 UTIs (n=2/44, 4%),25,59 attention deficit hyperactivity disorder (ADHD) (n=1/44, 2%)29 and obesity (n=1/44, 2%).55
Articles dealing with a specific condition or condition group generally had a corresponding treatment of focus. For example, articles describing services for the management of ARIs often had a focus on antibiotic prescribing (n=9/44, 21%).8,25,27,28,53,54,58,59,63 Those that examined conditions such as erectile dysfunction, ADHD or obesity also focused on treatments for each corresponding condition, such as PDE5 inhibitors (n=3/44, 7%),12,47,60 non-stimulant ADHD therapies (n=1/44, 2%)29 or an oral superabsorbent hydrogel (n=1/44, 2%).55
Discussion
Summary of main findings
Our findings reveal a mismatch between the burgeoning demand and market growth of DTC telemedicine services and the pace of research conducted. The reviewed articles were largely cross-sectional analyses of user characteristics for various services. General user characteristics of DTC telemedicine services were considerably mixed and were largely dependent on the type of service being offered and if it was restricted to specific conditions or populations. Most articles examined acute or subacute conditions that were treated in isolation with a clear gap in the literature on the use of DTC telemedicine for chronic conditions or multimorbidity. Publications focusing on aspects of quality and safety mainly looked at prescribing patterns and particularly antibiotic prescribing. Even articles that specifically reported on the overall quality of a particular service12,27,42 mainly analysed prescribing patterns and rates of side effects without assessing other aspects of quality, such as efficiency, effectiveness, safety, patient-centredness, timeliness and equity, as defined by the Institute of Medicine’s theoretical framework.64 There was also heavy reliance on quantitative research methods using retrospective study designs, leaving a substantial gap in qualitative insights and prospective research. Notably, there was also a lack of contemporary studies exploring clinicians’ perspectives on DTC telemedicine.
Equity and access
There is a notable lack of understanding of equity in and access to DTC telemedicine services. Most studies were conducted in high-income countries, raising questions about the generalisability of these findings to global populations. This skew towards high-income nations might reflect a tendency of neoliberalist economies to rapidly adopt and integrate new technologies, particularly those with commercial potential.65 Alternatively, it could be indicative of a broader reflection of global wealth disparities, where only regions with substantial financial resources can afford to invest in and research these emerging healthcare modalities. Both factors could be relevant. Regardless of which, this disparity highlights a significant concern about the equitable distribution of telemedicine services and the potential exclusion of low- and middle-income countries from both research and the benefits of such innovations.66
Health economics and healthcare utilisation
From a health economics perspective, the literature is notably lacking in cost–benefit analyses at the health system level. Although one study addressed the consumer cost of obtaining prescriptions for PDE5 inhibitors,60 there is a paucity of work seeking to understand the overall economic effects of DTC telemedicine services on healthcare systems. Filling this gap is particularly critical for countries with predominantly publicly funded health systems, where it is essential to ascertain whether commercial telemedicine entities contribute to cost savings or result in increased healthcare expenditures for governments.67,68
Only three articles analysed the effects of DTC telemedicine on healthcare utilisation. All three studies explored downstream utilisation, whereas only one study looked at upstream utilisation. Lapointe-Shaw et al found that compared to patients who had consults with their regular physician, DTC telemedicine patients had lower previous healthcare use, were less likely to have a subsequent in-person physician visit and were more likely to visit the emergency department within 30 days.37 Li et al and Dahlgren et al also found similar associations that DTC telemedicine use was predominantly associated with downstream care encounters.52,56 Given the modest number of studies in this area, there is an ongoing need for data-linkage studies and thorough health economics analyses to understand the effects of these services on healthcare systems and guide policymaking for the optimal integration of DTC telemedicine into
primary care.
Qualitative insights
The existing literature is heavily reliant on quantitative research methods, leading to a shortfall in qualitative insights. Only three studies used some form of qualitative method, one of which was a usability assessment of a services website interface;50 the other two evaluated healthcare practitioners’ views and consumer preferences on using mobile teledermoscopy for skin cancer diagnosis.33,36 This lack of qualitative research leaves unanswered questions about the reasons patients choose to use DTC telemedicine services and their perceptions of these services. Qualitative studies looking at other conditions and more general services are essential to further explore the patient experience, understand the motivations behind the use of these services and assess patient satisfaction.
Clinicians’ perspectives
Another notable omission in the current body of research is the lack of studies exploring clinicians’ perspectives on DTC telemedicine. Only one study focused on healthcare practitioners’ views.33 Understanding the views and experiences of healthcare providers can shed light on the challenges and opportunities presented by this mode of service delivery, including aspects of care quality, the efficacy of communication methods and the effects on their professional practice.69 Integrating the clinicians’ viewpoint is essential to ensure that DTC telemedicine services are not only patient-centric but also sustainable and effective from a provider’s standpoint.
Strengths and limitations
To the best of our knowledge, this review is the first to assess the contemporary empirical literature on DTC telemedicine within primary care. The findings highlight the type, breadth and range of DTC telemedicine services, as well as main health conditions serviced and treatments offered. This review has enabled the identification of critical gaps in the research on DTC telemedicine in primary care that can be leveraged in future research efforts.
This review has several limitations worth noting. Studies included in the review were not assessed for risk of bias, and the quality of evidence for each study was not appraised. The predominance of studies from high-income countries will limit generalisability to low-income regions with differing health systems. Eligible studies were restricted to those published within the past five years, potentially omitting relevant papers published in earlier years. However, this time frame was purposively selected as appropriate for capturing the evolving healthcare landscape since the onset of the COVID-19 pandemic. A grey literature search was not included, which might offer other insights and could be considered in the future.
Conclusion
Our review highlights a critical need for multifaceted research on DTC telemedicine within primary care. Future research should focus on understanding the reasons behind patients’ preference for DTC services compared with traditional primary care, assessing the effects of these services on the primary care workforce, developing quality assessment tools and examining the health economic implications of DTC telemedicine services. Additionally, exploring these services from a commercial determinants of health perspective is essential, particularly considering growing investments from major corporations. Comprehensive research is vital to inform policy and regulatory decisions, ensuring that commercial services are integrated effectively with traditional primary care systems, ultimately enhancing the overall quality and efficiency of primary healthcare.