Sudden sensorineural hearing loss (SSNHL) is an otologic emergency that demands prompt evaluation and intervention. This review article provides an extensive overview of the current state of SSNHL management, encompassing its epidemiology and aetiology, diagnosis and evolving treatment modalities.
Aims
This review aims to equip healthcare providers with a comprehensive understanding of SSNHL and its management strategies through collating up-to-date research and clinical guidelines. Furthermore, an evidence-based approach on the aetiology, diagnosis, investigations, treatment and prognosis is examined, along with Australian-specific healthcare considerations to guide the Australian general practitioner (GP) specialist in providing comprehensive care for the patient who presents with SSNHL.
Aetiology
SSNHL is a rapidly progressing hearing loss (defined as occurring within a 72-hour period), often unilateral in nature. The cause of SSNHL is idiopathic in over 70% cases.1,2 Other causes can also be infectious or inflammatory (often viral), neoplastic, autoimmune, vascular, trauma or iatrogenic.1
Bilateral SSNHL is exceedingly rare; however, it can still occur. Examples include ototoxic medication (eg aminoglycosides or chemotherapy), syphilis or certain autoimmune or vascular conditions. SSNHL due to aminoglycoside ototoxicity might initially progress undetected as it typically affects the higher frequencies first before progressing to lower speech frequencies.3,4 Patients with bilateral SSNHL are often older, have a positive antinuclear antibody titre and have a higher prevalence of vascular disease.5
Although the aetiology is important for prognosis and might change future management, the immediate management of SSNHL at the initial GP specialist appointment remains the same for all SSNHL cases.
The exact incidence of SSNHL is unknown, as many patients do not seek medical attention or the condition might spontaneously resolve. Within the literature, estimates of SSNL annual incidence ranges from five to 27 cases per 100,000.6,7
Since the COVID-19 pandemic, it was theorised that a viral pandemic might lead to an increased incidence of viral-induced SNHL; however, the literature on this relationship remains equivocal.8
Diagnosis
Diagnosis of SSNHL can be challenging and delay to diagnosis can result in poorer outcomes due to the time-critical relationship between onset of symptoms, initiating steroid therapy and prognosis.
SSNHL can often be masqueraded by other benign ear conditions, such as otitis media with effusion or cerumen impaction. Further, the prevalence of pre-existing hearing impairment in the general Australian population is high; 3.6 million people have some degree of hearing loss and more than one in three Australians have noise-related aural damage, which can often further confound the diagnosis.9 In these cases, if the clinical history is not entirely clear, then comparison to previous recorded audiometry is of value to aid in diagnosis.
Table 1 outlines the key features in the history and physical examination in SSNHL. Box 1 details the key differentiating factors between conductive hearing loss (CHL) and SSNHL. Box 2 demonstrates how the authors conduct the tuning fork examination within clinic.
Audiogram is the gold standard and most definitive method in diagnosing SSNHL; however, if same day audiogram cannot be achieved, do not delay treatment while awaiting investigations, as delay to treatment results in poorer outcomes.10 Figure 1 shows the audiogram of a patient with right SSNHL.
In cases where a tuning fork might not be available to the GP specialist, it has been shown that a smartphone application (The Real RazorTM) might be a practical alternative in the primary care setting.11 When placed on silent mode, the app causes the mobile to vibrate at a frequency of 163 Hz. The Weber test is then conducted with the corner of the vibrating smartphone; results from the study showed >97% agreement when compared to the standard tuning fork for the Weber test.11
| Table 1. Key features in the history and examination for sudden sensorineural hearing loss |
| History |
Examination |
- Often unilateral hearing loss
- Sudden onset
- ± vertigo
- ± preceding coryzal symptoms
|
- Overall benign or unremarkable otoscopic examination with absence of infection or pathology
- Pinna/external ear; unremarkable
- External auditory canal; clear or with benign cerumen
- Tympanic membrane; clear
A full cranial nerve examination should also be performed to exclude any concomitant or causative pathology. |
| Box 1. Clinical pearl |
- Often, otoscopic examination for sudden sensorineural hearing loss is normal, whereas acute hearing loss secondary to conductive causes more often has a ‘positive’ finding.
- Clinical examples of sudden CHL include: otitis externa (pain, swelling and purulent canal debris), otitis media (pain, red TM ± fevers), acute TM perforation from infection or barotrauma (perforated TM), otitis media with effusion (aural fullness or ‘blocked ear’, might have preceding coryzal symptoms).
|
| CHL, conductive hearing loss; TM, tympanic membrane. |
| Box 2. Tuning fork examination |
Tuning fork examination is key to differentiating CHL from SSNHL and should be performed in all patients presenting with hearing loss. The authors describe how this is typically conducted in an ENT specialist clinic:
- Optimise environment
- Position/environment: ideally the patient should be sitting on a chair, with any head gear/glasses removed. b. Examination should be performed in a silent room.
- Equipment: a 512-Hz tuning fork.
- Weber’s test
- Strike the fork against knee/elbow or surface to create reverberation.
- Place the fork midline on the patient’s forehead.
- Ask the patient to identify if the sound is louder in one ear or the same in both.
- In SNHL, the sound will be heard louder in the contralateral (unaffected) ear.
- Rinne’s test
- Introduce the test prior to performing it; explain to the patient that the fork will be held in two positions; behind the ear and in front of the ear. Ask the patient to identify in which position the sound is loudest.
- Strike the fork against the knee/elbow/surface to create reverberation.
- Place the fork directly on the mastoid process (tests bone conduction), then move the fork to approximately 1 cm from the ear (tests air conduction).
- In SNHL, this test will be ‘normal’ with air conduction and greater than bone conduction.
- Clinical pearl: Take caution in interpreting Rinne’s test in the patient with total SNHL (ie a ‘dead’ ear) as testing will yield a ‘false‑negative’ result.
- Clinical example: in a patient with left total SNHL, on testing Rinne’s on the left ear, bone conduction will be louder than air conduction, thereby producing a false‑negative Rinne’s result.
|
| CHL, conductive hearing loss; ENT, ear, nose and throat; SNHL, sensorineural hearing loss; SSNHL, sudden sensorineural hearing loss. |
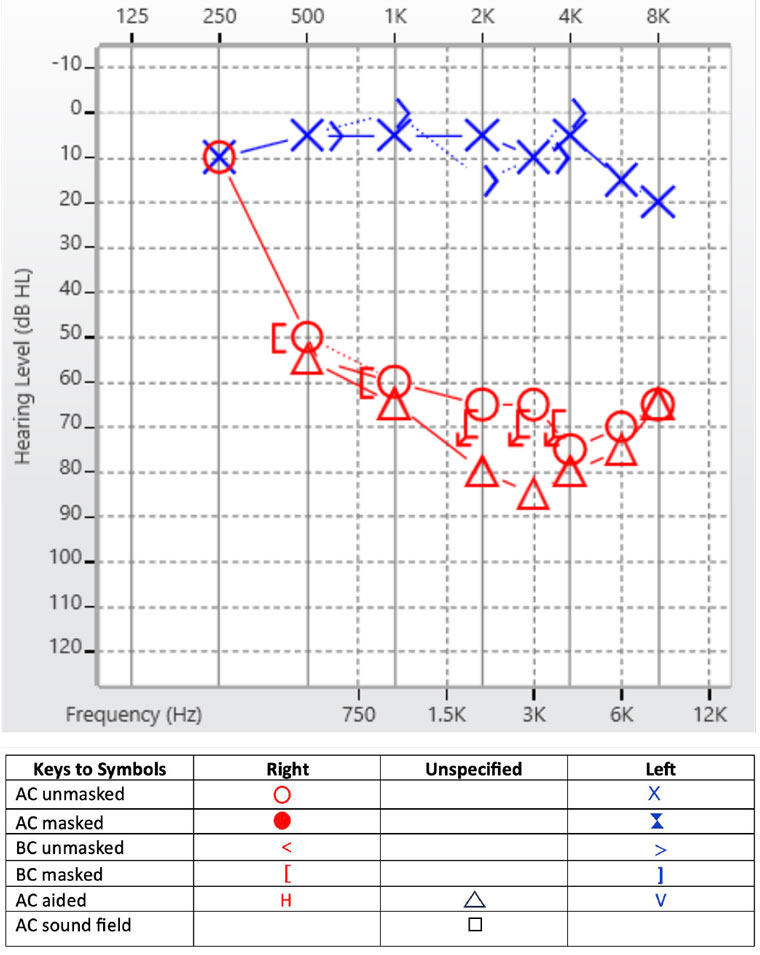
Figure 1. Audiogram in a patient presenting with sudden sensorineural hearing loss.
Treatment
As per recently updated National Institute for Health and Care Excellence (NICE) Guidelines, an adult with sudden hearing loss within the last 30 days requires immediate referral (to be seen within 24 hours) to an ENT service or an emergency department.12,13
Oral high-dose systemic corticosteroids are the gold standard treatment for SSNHL, with initiation of therapy immediately at the time of suspected diagnosis essential. At our centre, a daily morning dose of prednisone 1 mg/kg (max 75 mg) for a minimum of five to seven days is the targeted treatment of choice. Further dosing and tapering of medication is generally clinician dependent. Early initiation of therapy improves prognosis, with the greatest advantages observed within the first two weeks of onset. Following this window, there is a significant decrease in the amplitude of hearing improvement.14
Contraindications to the corticosteroids, patient counselling and monitoring for side effects might be considered.
For SSNHL greater than 30 days ago, urgent referral to an ENT service is indicated to view candidacy for intra-tympanic corticosteroid injection in which the steroid is directly infiltrated into the middle ear space with diffusion via the round window into the inner ear to reduce local inflammation.
A systematic review and meta-analysis demonstrated the role of intra-tympanic dexamethasone to be equivalent to oral steroid therapy as primary treatment but has greater improvement in hearing outcomes as salvage treatment, with a mean improvement of 13.3 decibels (dB).15
Overall, SSNHL greater than 30 days ago is a clinical ‘grey window’ within primary care. Apart from referral to an ENT service, there is no specific treatment algorithm to follow and cases would require a case-by-case analysis and discussion with each individual patient. Many clinicians continue to offer systemic steroid treatment for SSNHL lasting longer than 30 days but generally not past six weeks. We recommend a shared decision-making model, including discussions of risk, benefit and expected prognosis (which is poor).
Hyperbaric oxygen therapy (HBOT) is a useful adjunct for the treatment of SSNHL in adults and might have benefit when combined with steroid treatment in the acute setting or as salvage treatment within one month of onset.16
A shared decision-making model might be of benefit when considering HBOT due to social and financial considerations. Factors that might influence the patient’s decision include accessibility to the service, travel and the time-intensive nature of treatment typically requiring 10–20 sessions within a few weeks. Further, if sought privately, HBOT can be costly if not covered by the patient’s health fund. In Australia, there are nine publicly funded hyperbaric facilities with comprehensive cover; referral to these services to assess patient eligibility might be worthwhile.
Investigations
Audiogram is the most definitive investigation to diagnose SSNHL. There are varying diagnostic criteria for SSNHL, with the most common being a sensorineural hearing loss (SNHL) of 30 dB or greater over three consecutive test frequencies over a 72-hour period.2,16 SSNHL has also been described as a loss of 10–20 dB in two or three frequencies occurring within 12 hours.17
Magnetic resonance imaging (MRI) of the internal acoustic meatus (IAM) with contrast is the most sensitive and specific test in detecting retrocochlear pathology and can detect cerebellopontine angle tumours as small as 1 or 2 mm.18 It is recommended that an MRI be performed within three months of onset in all patients with SSNHL.16 Other pathologies that might be identified on MRI include intracranial lesions, such as multiple sclerosis or meningeal carcinomatosis.19
For patients in which MRI is contraindicated, computed tomography (CT) with contrast of the temporal bone in conjunction with an auditory brainstem response (ABR) on audiometry, can be performed.
The most recently updated guidelines and systematic review from the American Academy of Otolaryngology Head and Neck Surgery do not recommend obtaining routine laboratory tests in patients with idiopathic SSNHL.16 However, a tailored clinical approach to the patient is still recommended, particularly if the clinician suspects an underlying aetiology such as vascular or autoimmune conditions. Ultimately, the management of SSNHL can be challenging, thus a treatment algorithm or ‘roadmap’ for the management of SSNHL (see Figure 2) has been created for use within the primary care setting.
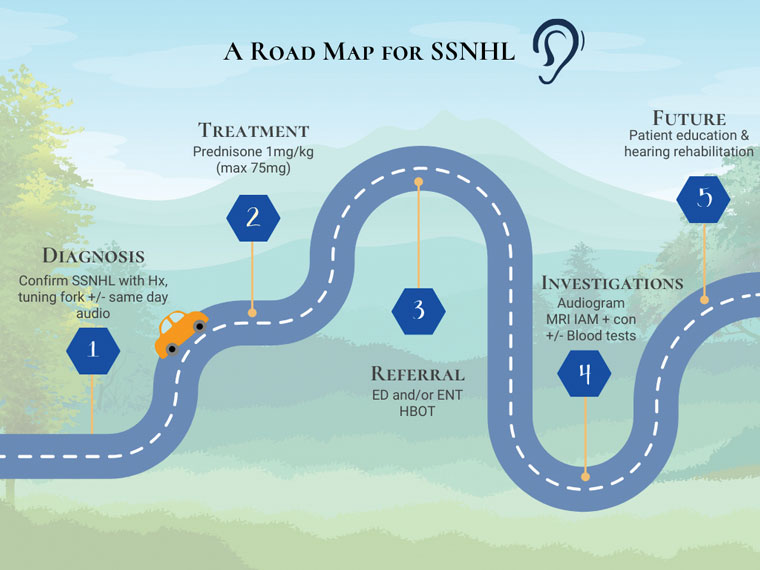
Figure 2. A road map for sudden sensorineural hearing loss (SSNHL) in the primary care setting. This figure demonstrates a practical algorithm to guide general practitioner specialists in the management of SSNHL.
ED, emergency department; ENT, ear, nose and throat; HBOT, hyperbaric oxygen therapy; Hx, history; IAM, internal acoustic meatus; MRI, magnetic resonance imaging.
Future considerations: Where to from here?
Overall, patients who have experienced only one episode of SSNHL, particularly when idiopathic, are unlikely to have another episode. However, providing counselling on the management of future episodes and ensuring the patient understands the emergent nature of the condition can lead to better patient empowerment and improved health literacy. A repeat audiogram in 6–12 months to ensure hearing levels are stable might be useful.
If the patient experienced concomitant vertigo, this typically indicates a poorer prognosis in recovery of hearing loss. Meniere’s disease might also be considered; a condition characterised by two episodes or more of vertigo with aural symptoms (hearing loss, aural fullness, tinnitus). The hearing loss is predominantly a low frequency SNHL, and tinnitus is characteristically ‘roaring’ in nature. The vertiginous episodes typically last from 20 minutes to 12 hours with the likelihood of diagnosis less likely if only lasting minutes or on the contrary for days.20
Indications for hearing rehabilitation devices are generally indicated, particularly if the hearing loss is moderate–severe or if it is affecting the patient’s quality of life. It might also be useful to consider the eligibility criteria under the Australian Government Hearing Services Program for conventional hearing aids, as privately purchased hearing aids can be costly for the patient. If the patient is aged <26 years or >75 years, then they will be eligible for a government subsidy. Therefore, if patients are close to these age thresholds and remain unsure, appropriate counselling and education on this might encourage them to seek hearing aids while they are still eligible. The full eligibility criteria are available on the Australia Government Health website.21 Referral to ENT services for discussion of hearing rehabilitation options might be indicated if the hearing loss is not managed by conventional hearing aids alone due to the severity and/or if the hearing loss is impacting the patient’s quality of life.
Conclusion
In conclusion, effective SSNHL management in primary care necessitates a multidisciplinary approach, with GP specialists often serving as the initial point of contact. Improved awareness, timely diagnosis and evidence-based therapeutic interventions can significantly impact patient outcomes in this challenging clinical scenario. Ultimately, primary care providers play a pivotal role in optimising care for patients presenting with SSNHL, contributing to improved hearing preservation and quality of life.
Key points
- Sudden sensorineural hearing loss is an otologic emergency.
- Prompt diagnosis and initiation of treatment with high-dose corticosteroids improves patient hearing outcomes.
- Do not delay treatment while awaiting investigations (ie audiogram).
- Prompt referral through to an ENT service and/or an emergency department is recommended.
- Consider adjuncts to therapy including hyperbaric oxygen therapy, audiovestibular services and/or intra-tympanic dexamethasone.