Medical management of obesity occurs within publicly funded services and private clinics that might allow patients to access rebates for appointments. Primary care can provide first-line services for obesity management either through general practitioners (GPs) or allied health practitioners. The Australian Obesity Management Algorithm suggests that management of people with a body mass index (BMI) of 30–40 kg/m2 without obesity-related complications is ideally delivered in primary care, whereas shared care with specialist services should be considered for those with a BMI of 30–40 kg/m2 with complications or those with a BMI >40 kg/m2 without complications.1
Aim
This paper uses two case studies – both patients with a BMI >40 kg/m2 – managed by the same GP in different systems; one in a private general practice using Medicare rebates and the other in a publicly funded obesity management clinic (PFOMC) to illustrate the differences the system makes to timing, delivery of care, cost and access to multidisciplinary care, as well as remuneration for the doctor.
Case studies
Susan
Susan, a new patient, booked a 15-minute appointment at a private billing general practice. Her background includes type 2 diabetes for which she takes three antihyperglycaemic agents. She is teary, explaining that she is putting on weight, struggling to implement recommended strategies and that her blood sugars had increased on her last blood test. She admits that sometimes, she ‘can’t stop eating’ and is unsure whether she is hungry during these episodes. Susan is not interested in discussing diet further as she has already seen multiple private dietitians and diabetes educators before. Her Binge Eating Disorder Screener 7 score is not concerning. Susan is interested in pursuing psychology to manage her stress, which is a trigger for non-hungry eating. Advice around non-hungry eating in the context of stress and a referral to a psychologist is provided. She agrees to return for consideration of a chronic disease care plan to facilitate Medicare Benefits Schedule (MBS)-rebated appointments to other allied health professionals. The consult lasts 30 minutes and a breakdown of the time spent in the initial GP appointment is shown in Figure 1.
Susan books a 15-minute appointment one month later for a skin issue. She reports a further 2-kg increase in weight. She tried to book a psychology appointment, but the wait time was eight months and she lost motivation to seek other providers. Her other presenting complaint is addressed and motivational interviewing to help identify a single goal that Susan can concentrate on for weight management is undertaken. The consult ends in 19 minutes. A follow-up appointment is made but she does not attend. Her BMI over time is shown in Figure 2.
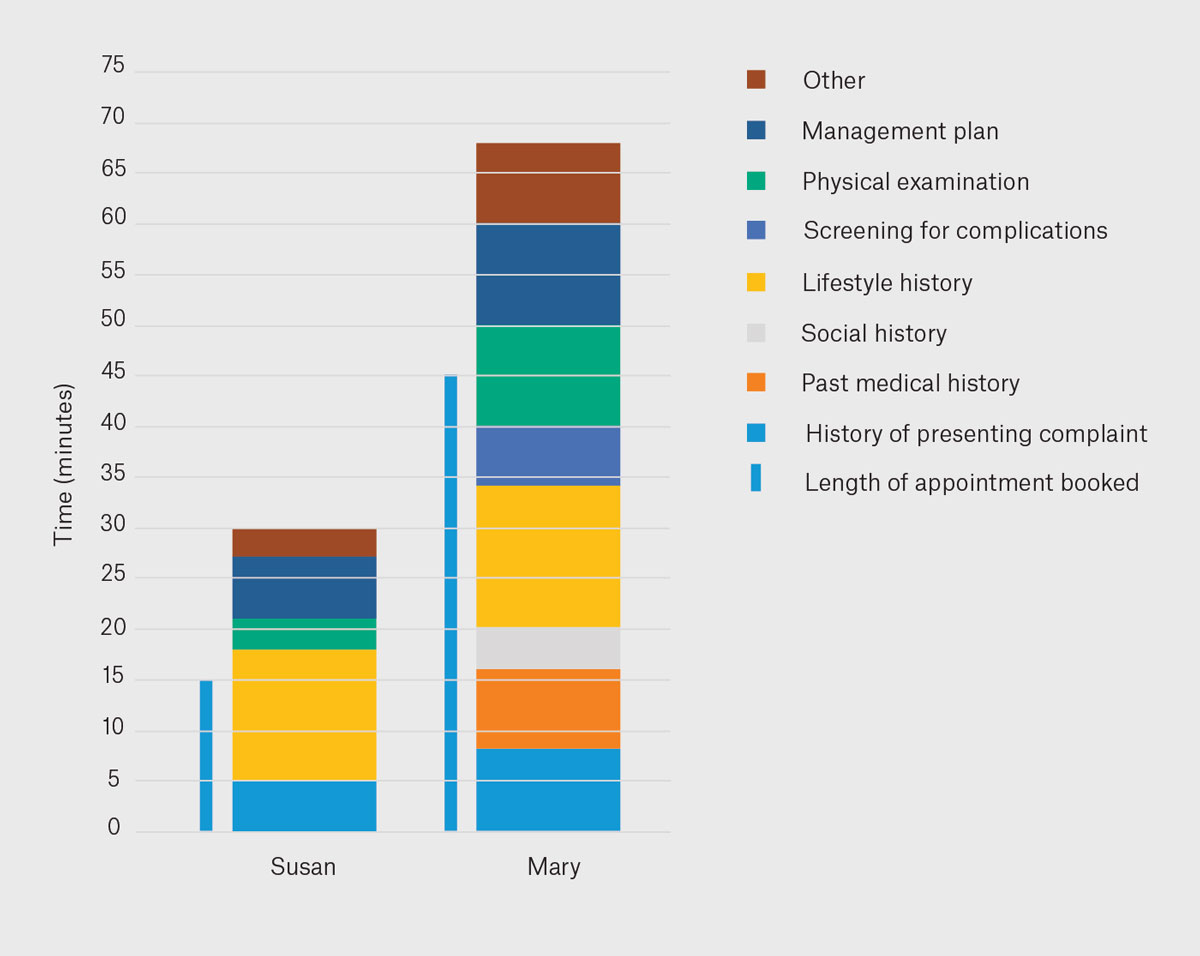
Figure 1. Breakdown of time spent in the initial consult for Susan (Patient 1 in a privately billed clinic) and Mary (Patient 2 in a publicly funded obesity management clinic).
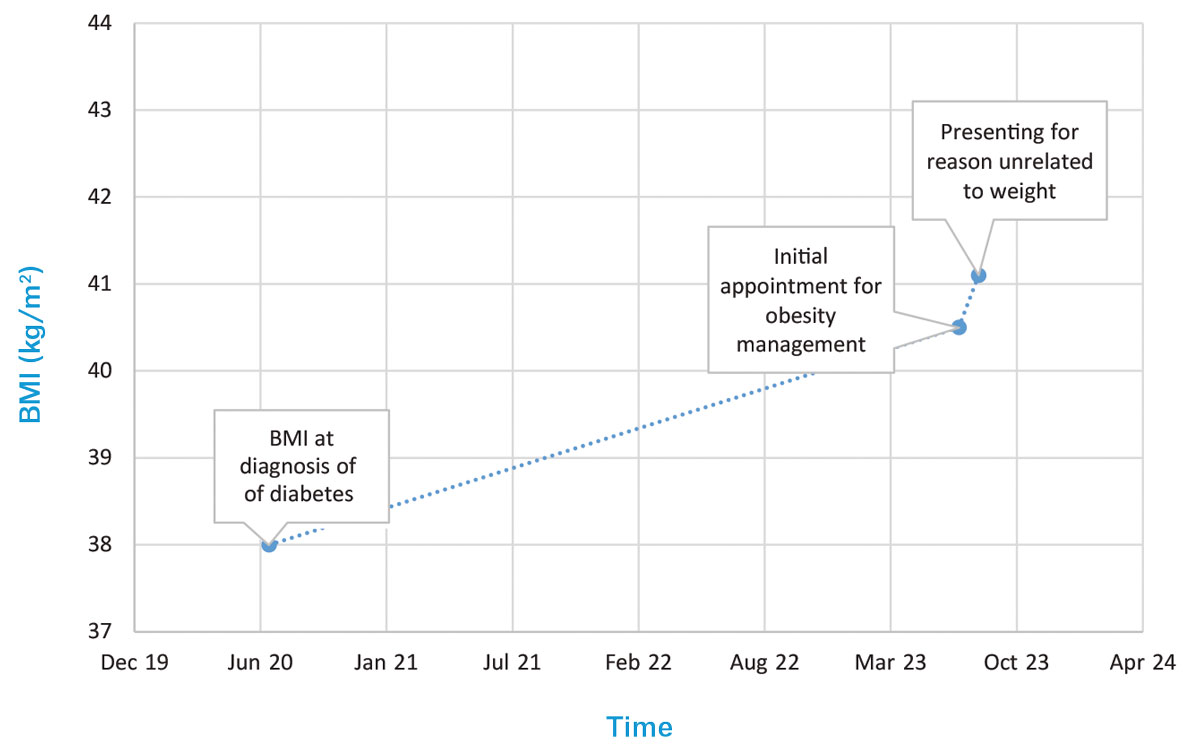
Figure 2. Body mass index (BMI) over time for Susan (Patient 1 in a privately billed clinic).
Mary
Mary was referred to a PFOMC that uses a multidisciplinary model of care. Due to long wait times, an updated referral was sent by her GP for increasing weight, but unfortunately her triage category did not change. Her initial appointment of 45 minutes is scheduled two years after the first referral. She is diagnosed with diabetes after her initial appointment at the PFOMC. Mary admits to significant stress resulting in her indulging in poor dietary choices ‘after a bad day’. Mary is booked for education sessions on lifestyle interventions and self-management principles, and referrals to other allied health members of the team are made. A follow-up medical appointment is made for six months. A breakdown of her initial appointment at the PFOMC is shown in Figure 1.
Five months before her second appointment at the PFOMC, Mary was commenced on phentermine by her regular GP. The dose was later reduced due to the side effect of insomnia. Mary is still having some insomnia but has not followed-up with her regular GP. At the PFOMC, phentermine is swapped to a phentermine/topiramate combination to limit side effects but maintain weight loss. Mary reduces most of her alcohol, soft drink and discretionary food intake on her own after the group education and only sees the dietitian and exercise physiologist after her fourth PFOMC medical appointment. She discusses strategies to further improve her protein intake with the dietitian to help reduce hunger through the day after the exercise physiologist flagged this as a concern during an exercise assessment. Her BMI over time is shown in Figure 3.
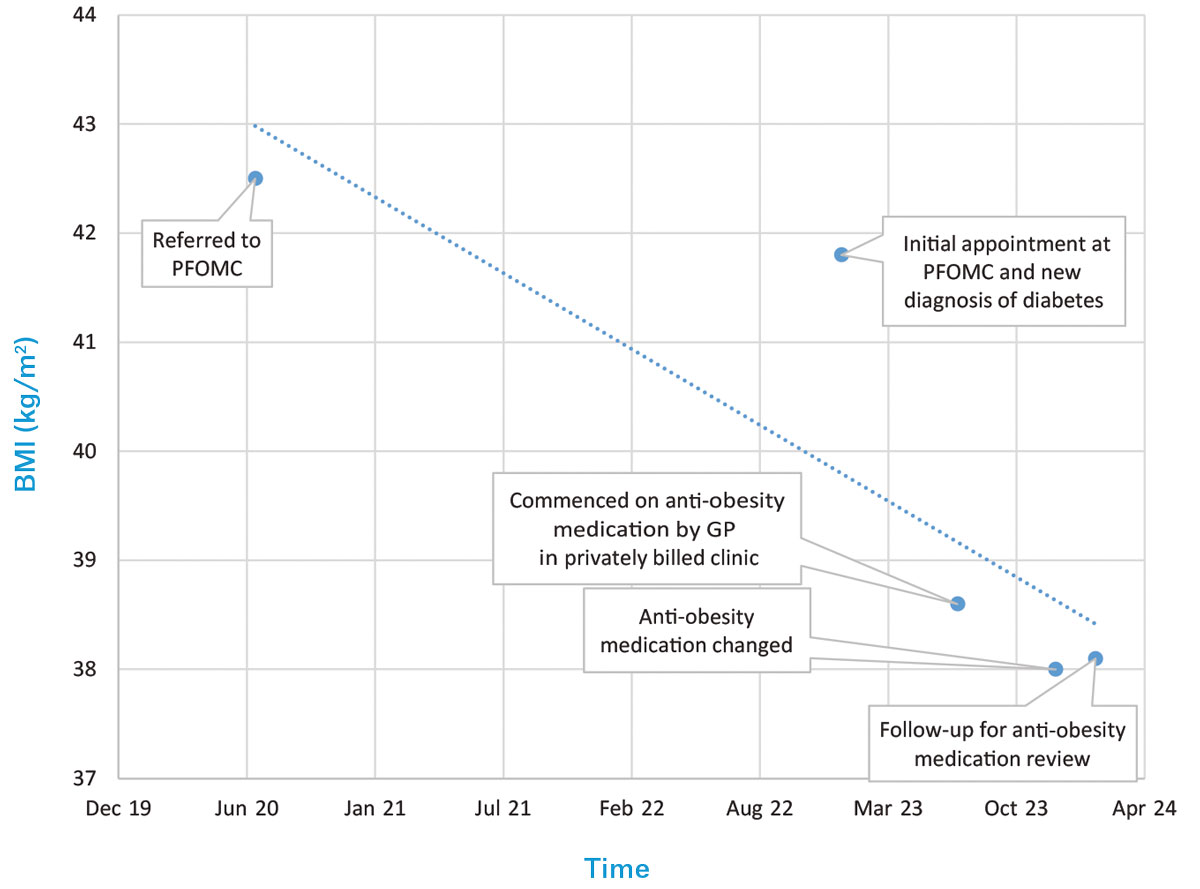
Figure 3. Body mass index (BMI) over time for Mary (Patient 2 in a publicly funded obesity management clinic).
GP, general practitioner; PFOMC, publicly funded obesity management clinic.
Case discussion
Referencing the framework initially outlined by Swinburn et al to categorise obesity determinants and solutions, both patients discussed above require physiological interventions as distal interventions that target environmental and behavioural drivers are unlikely to significantly change obesity and its associated comorbidities in these individual patients.2 Although upstream interventions that tackle systemic drivers have larger population effects, these are harder to implement, thereby contributing to higher prevalence of obesity2 and leaving patients like Susan and Mary to navigate different models of care on their own to achieve their health goals.
Reflections on the system
Wait times
Data for routine wait times in primary care are sparce, but evidence suggests that it takes an average of nine years after patients first struggle with their weight before they present to their GP for weight management.3 This might be due to inadequate self-awareness of obesity or perceived weight stigma.3,4 For Susan, the long wait time for psychology review was a significant barrier to care. The wait time was not communicated to the GP, so they did not know the outcome of the referral until Susan returned for review.
Mary spent over two years waiting for an appointment at the only dedicated PFOMC in the region. This particular PFOMC uses a multidisciplinary and case management model.5 Appointments at this service are typically 45 minutes and time is allocated for anthropometry and screening. Access to PFOMCs is challenging, with most having strict entry criteria, prolonged wait times or being located in a major city.6 In 2017, of 16 such services in Australia, six had more than 300 patients on the waitlist, with waiting times ranging from months to years.6 Referrals also appear to be increasing, with 100 referrals between 2017 and 2018, 142 referrals between 2018 and 2019, and 457 referrals to a PFOMC between 2021 and 2022.5
Delivering care
GPs were the most common healthcare professionals approached to discuss weight by people with obesity.7 The role of primary care in the Australian Obesity Management Algorithm is described as identification of obesity and its associated comorbidities with regular monitoring and application of intensifying weight loss strategies if weight and health targets are not achieved.1 Causes of obesity are multifactorial and taking a relevant history could include comorbidities, dietary habits, physical activity and screening for mental health symptoms, eating disorders and complications of obesity, all of which are difficult to cover in a standard appointment. In Australia, 60% of healthcare professionals cited short appointment times as a barrier to discussing weight management.3 Mary however, attended education sessions on lifestyle interventions and principles of weight management after her initial appointment, thus freeing up time in her consult. It is hard to know, however, whether this is standard practice in PFOMCs, as even within Australia, there is great variability in the composition of public clinics impacting the interventions on offer.6
As in Susan’s case, GPs manage competing health issues, making consistent follow-up for obesity alone challenging, particularly when the duration of the consult impacts patients’ out-of-pocket costs. However, Susan’s second appointment for a skin issue was another opportunity to revisit health goals and encourage behavioural change as part of holistic care. Alternatively, Mary, in contrast, used follow-up appointments at both the PFOMC and the privately billed GP clinic. Encouraging consistent follow-up for obesity is challenging. Of people living with obesity across 11 countries, 39% reported that the prices of obesity medications, programs or services were barriers to weight loss.7 Follow-up appears important to clinical outcomes, with there being 21.4% greater odds of the patient achieving clinically significant weight loss with every additional follow-up visit in a private clinic.8 Only 15% of people with obesity reported weight-related follow-up appointments in a self-reported survey,7 reflecting perhaps that obesity is not recognised as requiring GP follow-up even among patients. Interestingly, however, reattendance rates reported in private facilities specifically for weight management were higher at 80.2%8 compared to 70.5% in a PFOMC.5
Out-of-pocket costs for patients
PFOMCs have high demand for their services, thus impacting their ability to follow-up patients frequently, so Mary still incurred out-of-pocket costs associated with private GP appointments. Furthermore, anti-obesity medications are not subsidised by the Pharmaceutical Benefits Scheme in Australia,4,9 and this contributed to Mary’s higher out-of-pocket costs (Figure 4). Comparatively, research from 2012 reported the cost per kilogram of weight loss as $137, with an average of 10 GP visits per participant over 12 months, with each visit lasting ≤20 minutes.10 However, the burden of obesity might disproportionately affect those who are already financially disadvantaged, which makes access to PFOMCs important. Sixty-eight per cent of adults in the lowest socioeconomic areas were living with overweight/obesity compared to 60% of adults in the highest socioeconomic areas11 and between 2021 and 2022, 7% of people needing to see a GP delayed or did not see a GP due to cost.12
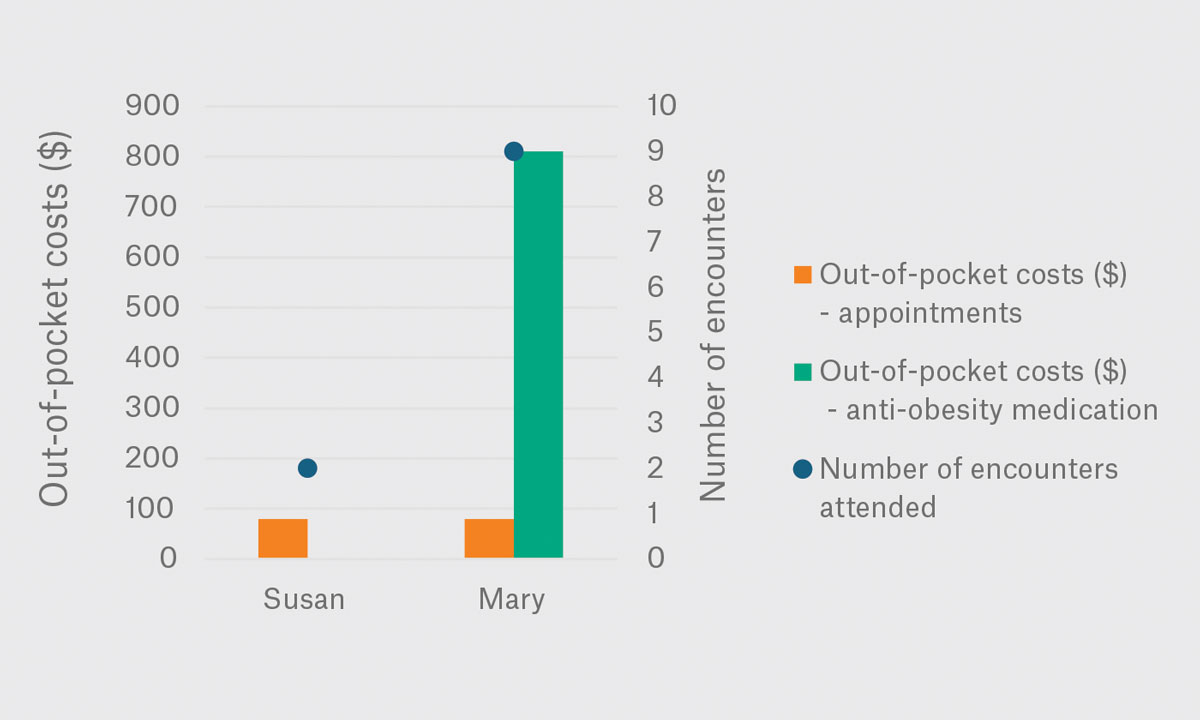
Figure 4. Number of encounters and costs associated with care for Susan (Patient 1 in a privately billed clinic) and Mary (Patient 2 in a publicly funded obesity management clinic) over the last 6 months of treatment.
Access to multidisciplinary care
A multidisciplinary approach is recommended for weight loss and long-term weight maintenance, as well as for chronic disease management.1,8 However, dietitians treating obesity under general practitioner management plans (GPMPs) identify insufficient rebates, insufficient time allocated to consultations and insufficient number of consultations for adequate follow-up as barriers to care.13 Weight management services in which providers are co-located facilitate interdisciplinary collaboration and communication6,8 as well as easier access to multidisciplinary, patient-centred care for patients. In Australia, only 47% of PFOMCs reported providing multidisciplinary care like that received by Mary.6 Additionally, Mary’s multidisciplinary team were co-located and used the same documentation system so providers could track anthropometry from each visit over time. Sharing of information did not rely on individual providers sending letters or on Mary relaying information between them. Furthermore, a multidisciplinary meeting allowed team members to raise concerns and adjust management contemporaneously. Mary admitted having found it inconvenient to attend multiple appointments but also found the interval between medical appointments at the PFOMC too long, leading to her seeking anti-obesity medication from her regular GP. Interestingly, of PFOMCs in Australia, only 33% offered pharmacotherapy services,6 making patients reliant on their regular GP for pharmacotherapy.
Remuneration of the doctor
GPs who work as contractors in private clinics take home a percentage of their billings based on the number of patients seen, with few additional benefits. Meanwhile, PFOMCs offer the doctor contained responsibilities, co-location of a multidisciplinary team, more time for consultation without impacting take-home pay and leave and professional development entitlements. This gives a relative disincentive for management of obesity in primary care by GPs; a challenge not limited to obesity alone. Overcoming these disincentives could facilitate improved management of comorbid conditions and holistic person-centred care with better continuity of care for patients as well as reduced pressures on PFOMCs.
Obesogenic environments
Managing obesity once complications are established is considered tertiary prevention,14 which is more costly and complex than earlier intervention. There is broad recognition that we live in an obesogenic environment2,15 and yet cost-effective strategies that target the upstream environmental drivers of obesity, such as regulation and taxes related to advertising of unhealthy foods and beverages and front-of-pack nutrition labelling, are not widely implemented.15,16 As detailed in the framework by Swinburn et al to categorise obesity determinants and solutions, interventions with greater population effects are essential to reduce the distal drivers of obesity.2 However, between 2013 and 2022, only 0.1% of the Australian Federal Government health budget was allocated to obesity prevention17 when obesity is related to 7% of the total burden of disease.4
Conclusion
In addition to weight stigma4 and the lack of coordinated regulatory actions to reduce the obesogenic environment,18 patients face system-specific barriers that impact timing, delivery of care and cost of managing obesity.4 PFOMCs are scarce, hetergenous and not adequately resourced to provide timely and comprehensive follow-up for patients, whereas private general practice does not typically support co-location of multidisciplinary teams that facilitate collaboration of team members as well as easier access to recommended multidisciplinary care for patients.6 Private general practice could provide better continuity of person-centred care but is over-burdened with little capacity currently for GPs to provide preventative education or to provide group-based interventions for their patients. Although care plans are enablers to accessing multidisciplinary care, barriers such as those faced by Susan are not resolved by care plans. Furthermore, despite provision of care plans, the additional costs of anti-obesity medications fall almost entirely on patients. Those who are already socioeconomically disadvantaged and more vulnerable to developing obesity are consequently less able to access care.11,15,19 Managing obesity requires preventative strategies as well as a multimodal approach to reduce weight stigma and system-related barriers to accessing care in both the public and private settings.
Key points
- Compared to global results, Australians with obesity take three years longer to present for weight management.3
- Inadequately resourced PFOMCs contribute to long wait times for patients seeking care in the public system,5 whereas short appointment times, lack of dedicated follow-up for obesity and remuneration can be a barrier to delivering care for GPs.
- Multidisciplinary care, which is recommended in the Australian Obesity Management Algorithm, can be difficult to access in both public and private systems.
- Weight stigma is a barrier to accessing care in both private and public systems and is perpetuated not only by individual health professional attitudes towards patients living with obesity but also by systems that do not identify obesity as a public health issue and allocate resources appropriately.
- Reducing obesity at a population level will require preventative strategies to reduce exposure to the obesogenic environment as well as public and private services that can manage obesity in individual patients.