Background
Tuberculosis infection (TBI) is an asymptomatic state in which people have been exposed to Mycobacterium tuberculosis, but not yet developed active disease. Most Australian models of care for TBI have been based in tertiary clinics, but people from affected communities consistently would prefer to receive care in a general practice setting.
Objective
This project aimed to develop and implement a model of care for providing safe and effective management of TBI in general practice settings. We describe a pilot program, including training, algorithms for management and resource development, to support holistic care.
Discussion
More than 20 general practices and pharmacies in south-eastern Melbourne have now adopted this model of care, involving community-based education, diagnosis and treatment, which has been integrated into existing practice approaches. A range of resources is now available to support general practice clinics in providing TBI care, including both professional development and patient-facing materials.
Tuberculosis infection (TBI; also known as latent tuberculosis infection) is an asymptomatic state in which people have been exposed to Mycobacterium tuberculosis, but not yet developed active disease.1 People with TBI can remain well for a prolonged and indefinite period after infection, and most people who develop active tuberculosis (TB) in Australia do so years or decades after migration from a high-incidence country.2 Estimates of TBI prevalence in the Australian community suggest that it is becoming more common, now affecting over 5% of all residents and 17% of residents born overseas.3 Identification of TBI is valuable because completing treatment with a variety of antibiotic regimens has been shown to reduce the risk of active TB by over 90%.4 However, most people with latent TBI have never been diagnosed and are unaware of their future risk of TB and of the availability of therapy to effectively prevent progression to disease.
Previous qualitative research with affected community groups in Australia has highlighted the perceived importance of local access to testing and treatment programs, and emphasised that general practice is the preferred site for education and management to occur.5,6 It has also been recognised that hospital-based outpatient services are unlikely to be able to scale sufficiently to provide accessible care for the large number of Australian residents potentially impacted affected by TBI.7 Establishing and resourcing an approach to providing holistic management of TBI in Australian general practices would be valuable in providing patient-centred care for people at risk of TB.
Aim
This project aimed to develop and implement a model of care for providing safe and effective management of TBI in general practice settings.
Development of the model of care
Since 2018, a partnership between the Victorian Tuberculosis Program (VTP) and the South-Eastern Melbourne Primary Health Network (SEMPHN) has developed and implemented a model of care for the management of TBI in general practice settings. There has been an emphasis on identifying younger (age <35 years) recently arrived (ideally within two years) migrants from high-incidence countries in order to reach those most likely to benefit from testing and treatment.
Prior to establishing this model of care, it has been uncommon for TBI to be managed entirely within general practice settings. Typically, people who were tested for TBI and found to have positive results have been referred to tertiary infectious diseases and respiratory clinics for exclusion of active disease and consideration of treatment. It was also recognised that many community members at risk of TB would not be tested for TBI routinely unless study or occupational assessment was mandated. Therefore, a central focus of this program was to develop educational tools for general practice clinics that would support awareness of appropriate testing practices, as well as algorithms for whole-of-cycle management of TBI in general practice settings. An initial algorithm was developed by medical and nursing staff of the VTP, with subsequent refinement in consultation with general practitioners (GPs) and practice nurses in participating clinics. Figure 1 shows the core pathway adopted for the model, allowing for appropriate selection of community members for testing, exclusion of active disease and treatment of TBI where appropriate, without the need for routine referral beyond general practice clinics.
Educational materials offered by the model include providing an understanding of Australia’s generally low TB incidence and focused risk in people who have migrated from higher-transmission settings. Training for this program covered selection of people for testing, interpretation of test results and the identification of people who would benefit from treatment, as well as management tools to support initiating, monitoring and successfully completing treatment for TBI. Resources such as patient-facing videos were also made accessible via QR codes on handouts and clinic posters to allow people considering testing/treatment for TBI the opportunity for review and to improve efficiency within consultations.
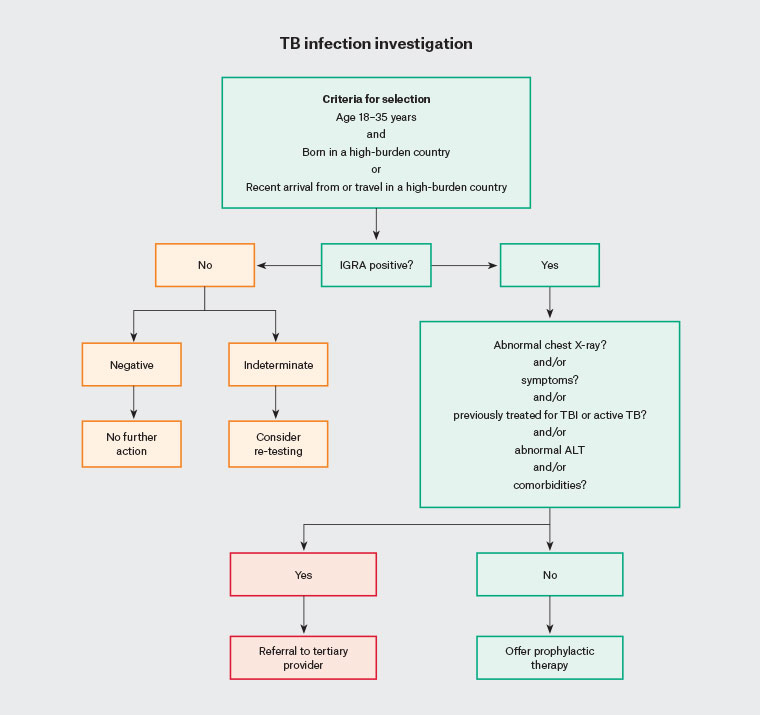
Figure 1. Flow chart of initial assessment for latent tuberculosis.
ALT, alanine aminotransferase; IGRA, interferon-γ release assay; TB, tuberculosis; TBI, tuberculosis infection.
Barriers and enablers
In Australia, diagnostic tests for TBI and excluding active TB are available through community-based providers, and available for order by GPs rather than restricted to TB programs or hospital-based services. Identified enablers for increased testing included the provision of education regarding the selection of those most appropriate to test and interpretation of results, as well as accessible patient-facing materials to encourage awareness of TB and preventive therapy. Commonly used medications for treating TBI, particularly rifampicin, are not listed on the Pharmaceutical Benefits Scheme for this purpose, and so additional barriers to access relating to cost and availability were recognised. Therefore, the program enlisted convenient local pharmacies and provided medication for dispensing without cost to the patient.
Key stakeholders for this project have included the VTP, SEMPHN, participating general practices, pharmacies and radiology and pathology services. In order to maximise accessibility for people undergoing testing and management for TBI, financial support for the cost of interferon-γ release assay (IGRA) testing was provided by the SEMPHN through a commercial pathology service for those not eligible for Medicare Benefit Schedule reimbursement. Medication for treatment of TBI was provided by the VTP, and dispensed from a local partner pharmacy nominated by each participating general practice clinic.
Implementation
As of February 2023, 21 general practices have participated in the program, including onsite and videoconference training in the diagnosis and management of TBI. Initial sessions include education relating to TB epidemiology and TBI diagnosis and treatment, as well as logistic support regarding accessing medication and resource materials. Onsite visits from VTP clinical nurse consultants and telephone follow-up were also provided to support testing, initiation of therapy and monitoring during treatment.
Project implementation was iterative across this period, with experiences and feedback reflected in the development of new tools and approaches as perceived to be helpful. New video resources for patients and families were produced, for example, in response to feedback about streamlining care and reinforcing key messages from practice staff. This flexibility in terms of structure has also allowed for the expansion of services provided by the participating practices, including new referrals from migrant screening services and involvement in contact tracing activities following household exposure to active TB.
A survey of participating practices was conducted in March 2023, at the time of concluding the initial introduction program. Although the emergence of COVID-19 had introduced well-recognised barriers to healthcare access during this time, the practices reported that over 900 people had been counselled with regard to TB risk and mitigation. Overall, practices were keen to continue providing services relating to TBI in their communities.
Sustainability
With regard to the sustainability of the model in general practice settings, our experience has allowed for the development and refinement of a range of support materials, including online video and print resources, which are now available for general use. Participating general practices and pharmacies are identified on the publicly available Victorian TB Program website (www.thermh.org.au/services/victorian-tuberculosis-program) as part of the latent TBI community of practice. Testing for TBI is widely accessible through commercial pathology networks, although cost remains an issue where individuals are not eligible for Medicare Benefit Schedule reimbursement.
Currently, the most commonly used treatments for TBI in Australia are rifampicin or isoniazid. Alternatives globally include shorter-course or intermittent regimens including rifapentine (which is not routinely accessible in Australia at present), and it is anticipated that in future other options will become available. The model and stakeholders established here will remain relevant, with these logistic arrangements able to incorporate new treatments and other emerging evidence as they become available.
Conclusion
This program has developed a model of care that supports holistic management of TBI, including education, testing and treatment, within a general practice setting. Funding for the project has supported the development of resources to improve sustainability and expansion to other general practice settings, including materials that are now available for general use.
Given the large number of people already resident in Australia with unrecognised TBI, this program has substantial benefits to offer clinics and communities. Even where treatment is not considered appropriate for an individual, the opportunity to provide education regarding active TB symptoms and pathways to access care are likely to support better healthcare engagement and less delay in diagnosis, leading to better health outcomes and less onwards transmission.8
There remain some barriers to optimal TBI care in Australia. Although there is a commitment to the provision of free medication for the treatment of TBI nationally, availability in some jurisdictions might be limited to defined hospital-based chest clinics, and active steps to distribute medication through community pharmacies or other accessible locations might vary. Testing for TBI with tuberculin skin tests and/or IGRA might also have varying degrees of accessibility Australia-wide, particularly for individuals without access to Medicare-funded services or who are not deemed to meet criteria for access. Finally, new and shorter courses of medication (particularly those based on rifapentine) that are not registered products in Australia will have limited uptake. Future expansion of TBI treatment in general practice contexts nationally will require consideration of these issues at local and jurisdictional levels. However, as we have demonstrated here, existing structures can already be used to support significant expansion of the availability and accessibility of TBI management, with incremental advances likely to follow in the future.
Key points
- TBI is a common condition in the Australian community that can be managed effectively in general practice for many people.
- People who have migrated from countries with a higher incidence of TB should be prioritised for latent TBI testing, especially younger people and those who have recently arrived.
- General practice is the preferred setting for TBI education and testing.
- Resources for patients and practitioners are now available for use, and can be accessed via the VTP (www.thermh.org.au/services/victorian-tuberculosis-program/about-vtp/managing-ltbi-in-general-practice-community-settings).
- People with suspected active TB should continue to be referred to jurisdictional TB services as per local pathways.