The COVID-19 pandemic has exposed the public health crisis created by lack of exercise.1 The stay-at-home restrictions have drastically limited physical activity and halted organised sport globally.2 For those who have had COVID-19, the pathway back to physical activity needs a roadmap.
While COVID-19 was initially thought to be primarily a respiratory condition, at least five other systems are commonly affected: cardiovascular, immunological, renal, haematological and neurological.3,4 More than one-quarter of patients with severe illness have evidence of cardiac damage, which may lead to myocardial scarring, exercise intolerance and arrhythmia.3 Presentations with post-viral chronic fatigue–like symptoms are increasing, and there is emerging evidence of long-term respiratory complications.4
Physical activity is a key component of long-term recovery from illness, and it has profound physical and mental health benefits.2 Patients recovering from COVID-19 will require guidance through a gradual reintroduction of activity,5 with due consideration given to possible complications. The Australasian College of Sport and Exercise Physicians has developed a guideline for all primary care practitioners to assist with safe return of patients to physical activity after a diagnosis of COVID-19.3,5,6
Assessing return to physical activity
To determine the appropriate return to physical activity, the relative risk of the patient returning to physical activity must be considered, in particular the risk of cardiovascular, respiratory and chronic fatigue complications. A thorough clinical assessment is required to evaluate initial symptom severity and secondary complications that may hinder exercise tolerance. This will stratify patients into three categories:
- Low risk – younger patients (aged <50 years) with recreational exercise goals who have had an asymptomatic infection or mild upper respiratory symptoms that have resolved within seven days.6
- Intermediate risk – patients who experienced prolonged symptoms or fatigue (>7 days) or ongoing shortness of breath or chest pain, which did not require hospitalisation.6 This group also includes elite and/or endurance athletes or those with pre-existing comorbidities that may affect recovery.
- High risk – individuals who required hospitalisation.6 This includes patients with any evidence of system involvement outside the respiratory tract,3,6 prolonged shortness of breath or chest pain at rest or with activities of daily living, along with significant cardiac comorbidities or abnormal electrocardiogram (ECG) or troponin findings during the illness.
Low-risk patients can enter a graded return to physical activity without further investigation. Intermediate- and high-risk patients should be considered for an ECG and baseline pathology, including a troponin test in the setting of chest pain, dyspnoea or an abnormal ECG.3,6 High-risk patients should be considered for a team approach to management including a cardiologist, respiratory physician and a sport and exercise physician to help with individualised exercise prescription.3,6
Graded return to physical activity following COVID-19
After a COVID-19 diagnosis, it is important that low-risk patients rest for at least 10 days. A graded return to physical activity can begin once the patient is symptom-free for seven days and no analgesia is required.5
The first priority is returning to baseline cognitive and physical loads at work/school, and to normal routines and sleep patterns. Physical activity should resume with 15 minutes of light activity until energy levels are restored, as lack of fatigue has been described as an important measure for patients in their recovery.7 The duration of light exercise should then be extended, followed by the addition of bodyweight exercise (eg yoga or resistance exercise), with adequate rest between sessions. This can be progressed to skills training, heavier resistance exercise and sport-specific training to restore pre-COVID-19 fitness. The presence of red flag symptoms such as chest pain, palpitations and severe shortness of breath or concerns about exercise intolerance warrants a review by the general practitioner, and the potential for referral to a cardiologist or respiratory physician.
Figure 1 is designed to assist primary care physicians with assessing risk, implementing a safe return to physical activity and developing team care arrangements where appropriate. This is a vital component of recovery from COVID-19, and this framework will help clinicians in guiding their patient’s return to physical activity, no matter their athletic ability.
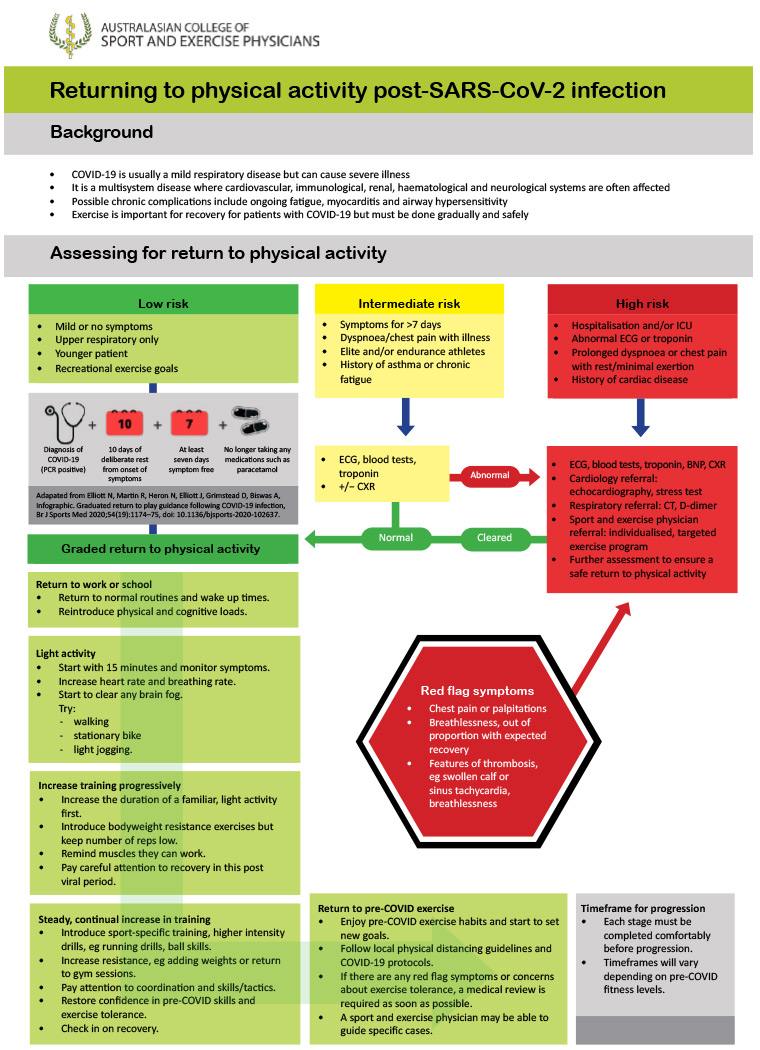
Figure 1. Return to physical activity flowchart. Click here to enlarge
BNP, B-type natriuretic peptide; CT, computed tomography; CXR, chest X-ray; ECG, electrocardiography; ICU, intensive care unit; PCR, polymerase chain reaction
Additional resources
British Journal of Sports Medicine podcasts
Elite athlete return-to-play guidelines
First published online 25 November 2020.