The outbreak of the Omicron strain of COVID-19 led to the most restrictive lockdowns ever implemented in Shanghai1 – from 1 April to 31 May 2022, citizens could not leave their homes under any circumstances, with the exception of special permit holders (eg medical personnel).2 The capacity of patients with chronic disease to visit their general practitioners (GPs) has been seriously affected. We present interim data on how GPs adapted management during the first two weeks of complete lockdown.
Face-to-face consultations, including with regular patients who have chronic disease, were immediately suspended on complete lockdown. Thus, the GP response aimed to manage these patients smoothly during lockdown. To ensure that patients received their regular medications, we communicated with patients with chronic disease who had detailed medical records in our electronic file system3 to allow us to arrange for delivery of their regular prescriptions/medications via community volunteers. In cases where there were any doubts regarding management, internet consultations were used to clarify issues. Approximately 80% of all consultations were conducted indirectly via non-medical community volunteers, based on patients’ routine prescriptions, and dispensed from the pharmacy at Tongren Hospital. The remaining 20% of patients with chronic illness felt that their medical condition had changed, and they undertook internet consultation with the general practice department, followed by delivery of prescribed medications. Patients with urgent concerns must call a hotline to request to attend the emergency department of a COVID-19-designated hospital.
Our initial evaluation of the impact of the complete lockdown on the delivery of clinical care by GPs to patients with chronic disease compares the number of general practice consultations for 15 days before and after the commencement of the complete lockdown (Table 1 and Figure 1). By day 15 post lockdown, patient consultations had increased >2-fold, compared with prior to lockdown (Figure 1), particularly for hypertension, diabetes mellitus, cardiovascular disease, hyperlipidaemia and insomnia (Table 1). These increased visits may have been precipitated by psychological stress/fear being increased by the lockdown, stimulated by uncertainties associated with the Omicron outbreak and aggravated by various sources of public information, including through social media.
| Table 1. Comparison of general practice disease consultations prior to vs post complete lockdown |
| Diseases |
Number of patients |
P value |
| |
Prior to lockdown |
Post lockdown |
|
| Hypertension |
1,939 |
4,204 |
<0.0001 |
| Diabetes mellitus |
792 |
1,602 |
0.1088 |
| Coronary heart disease |
366 |
945 |
<0.0001 |
| Hyperlipidaemia |
312 |
651 |
0.1498 |
| Insomnia |
277 |
640 |
0.0062 |
| Others |
4,500 |
7,458 |
<0.0001 |
| Total |
8,186 |
15,500 |
|
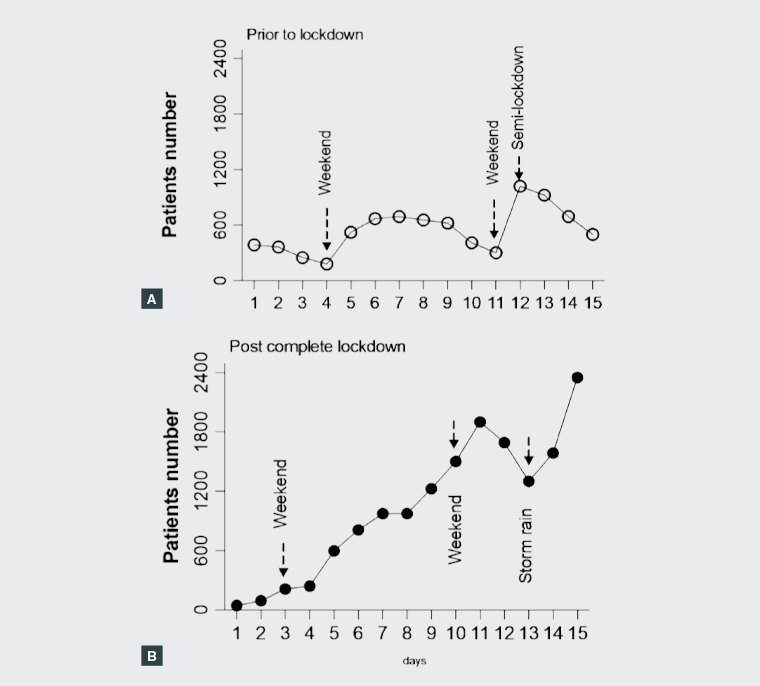
Figure 1. Number of patient–general practitioner consultations
A. Prior to lockdown; B. Post complete lockdown
There is a close link between stress and exacerbations of hypertension, cardiovascular disease and insomnia, likely to result in increased patient consultations. However, no significant differences in consultations for diabetes mellitus/hyperlipidaemia were observed prior to and after the lockdown, which may be due to a lack of short-term impact of stress associated with lockdown on these two diseases.
There was no significant difference in the number of consultations during the first five days of lockdown, probably because patients were caught unprepared. However, patient consultations rose between days six and 15 post lockdown, to >4-fold higher by day 15, compared with prior to lockdown (Figure 1), probably partially due to a compensation for the initially missing consultations, as well as patients becoming concerned about prescription shortages. Weekends have not affected the consultation numbers post lockdown (Figure 1B), which may be partially due to the lack of a weekend physical limitation for accessing consultations via volunteers post lockdown. The dramatic increase in consultations four days prior to complete lockdown (Figure 1A) was due to implementation of a less restrictive ‘semi-lockdown’ for four days prior to complete lockdown,4 motivating patients to attend the general practice department. The large decrease in consultations on day 13 post lockdown was due to a severe storm. Overall, the increased level of consultations may be due to panic associated with the lockdown coupled with the increased convenience for patients to order medications via volunteers on behalf of the patients.
In conclusion, the general practice department seems to have adapted to managing regular patients with chronic disease under severe lockdown, although the pattern of disease presentation has changed, probably reflecting increased stress under lockdown.
First published 4 July 2022.