In recent years, increasing numbers of e-mental health (eMH) programs have been designed to provide treatment and early intervention to patients with depression, anxiety and other common mental disorders (Box 1). These tools can be used with health professional support or independently by patients. Recent government initiatives, including the Fifth National Mental Health and Suicide Prevention Plan,1 have suggested eMH provides a solution to the significant treatment gap that exists for patients with mental health conditions, especially those who cannot access face-to-face services.2
| Box 1. What is e-mental health? |
e-Mental health (eMH) ‘refers to mental health services and information delivered or enhanced through the internet and related technologies’.19 It includes all technology-enabled therapies, including internet-based programs, mobile phone applications, telehealth and informational websites. An extensive list of information resources, apps, forums and services is maintained at the Head to Health website (https://headtohealth.gov.au/search-resources).
For the purposes of this article, we have focused on programs delivered via the internet that use text to deliver psychological therapies or educate consumers on mental health concerns. While some of these applications are clinician assisted, we have focused on the asynchronous material; this is designed to provide access to services whenever and wherever the consumer may be. eMH programs are a cornerstone of the Fifth National Mental Health and Suicide Prevention Plan,1 and are seen as a solution to access issues in mental health service delivery, particularly for consumers who are geographically isolated or lack access to face-to-face services. |
Mental illness is more common among Aboriginal and Torres Strait Islander peoples,3 people in rural and remote communities,4 and people with low socioeconomic status.4 Unfortunately, these people access mental health services at far lower rates than the general population.5 There is an assumption that eMH will address this treatment gap by providing an accessible, affordable, empowering and patient-centred solution for these patients and others who currently lack access to mental health services.6
Efficacy of e-mental health
The Royal Australian College of General Practitioners’ eMH guide claims there is strong evidence to support the use of eMH interventions in the management of mild-to-moderate depression and anxiety, although it notes English literacy competencies as a barrier to access.6 Trials of eMH resources have been positive, but some research suggests that uptake and use of eMH was low, and drop out was high, even with intensive telephone support.7,8 It is unknown whether these trials included representatives from the diverse populations that are currently underserved; they excluded patients who had severe or multimorbid illness, or who were minors or elderly. We also know little about those who dropped out. In the initial published trial of MoodGYM, the researchers commented that their participants were highly educated, and we do not know whether this is the case for many of the trials with these resources.8 There is also little evidence about the risk of harm. One meta-analysis suggested that in trials of online guided self-help, study participants with lower levels of education who were depressed were more likely to deteriorate during the trial.9
If we are to accept that eMH is a policy solution to inequitable access to services, we need to determine whether these programs can target patients in underserved populations. We believe that one of the key barriers to patients benefiting from these services is their ability to access and understand them. Unfortunately, there is little written about the impact of literacy levels on the capacity of patients to benefit from e-therapy.
Population literacy
Literacy levels vary across the Australian population. The Australian Bureau of Statistics’ adult literacy survey10 uses levels of literacy defined by the Organisation for Economic Cooperation and Development. They define five levels, with levels three and above being considered ‘adequate’ for ‘coping with the many demands of life in contemporary Australian society’.10 Fewer than 50% of Australians who have not completed an advanced diploma or higher degree have ‘adequate’ literacy. Only 25% of adults who have completed no higher than grade 9 high school education have ‘adequate’ literacy.11 Very little reputable online Australian health information is written at grade 8 or lower level.12
Australian high school data clearly show the gap in literacy between disadvantaged populations and Australia as a whole. At the grade 9 National Assessment Program – Literacy and Numeracy (NAPLAN) in 2015, children with low socioeconomic status or English as a second language have lower literacy, and literacy declined with rurality. Of Aboriginal and Torres Strait Islander students, 25.5% were below the national minimum standard for reading, compared with 4.7% of non-Indigenous students.13
Access to e-mental health
There may be other barriers preventing disadvantaged patients from accessing eMH resources. Although the proportion of households with internet access rose steadily for a decade, it plateaued at approximately 80% in 2014. Internet use for health purposes has risen rapidly since 2014 but had not yet reached a majority of households in 2017.14 People with high socioeconomic status are more likely to use internet resources more extensively, so it is likely they will also derive greater benefits from it.15 This ‘digital divide’ affects rural communities, who are less able to access and use eHealth, particularly in disadvantaged households.16
We also need to consider the skills needed to find, evaluate and apply eHealth information to personal health problems.16 eHealth ‘could unintentionally increase health inequalities because those in more advantaged circumstances might be able to access and use eHealth more easily than those more disadvantaged’.16
A mobile phone is a personal asset in some communities but may be quite restricted in areas of disadvantage. Prepaid services are often shared in remote communities, in which individuals need to share resources between family and friends, including phone or tablet credit.15 There is a similar digital divide among refugee migrant groups.17 Given the sensitivities of accessing and using eMH resources, it is likely that the digital divide means people with lower socioeconomic backgrounds, people located in rural and remote areas, those with lower education and those with culturally and linguistically diverse backgrounds are less able to access eMH resources, even if they are able to comprehend them.
There are also cultural barriers for populations with culturally and linguistically diverse backgrounds, many of whom are not open to the idea of eMH. In one language group, only 55% ‘indicated they would or might try internet-delivered treatment for their concerns about stress, anxiety or depression’.18 Aboriginal people in remote communities may not expect urban solutions to be useful.19 It is difficult, in an abstract area such as mental health, to describe in text such a layered and socioculturally embedded experience.20
Method
In this study, we aimed to assess the readability of common eMH resources and compare them with other texts in popular media and English literature. There is no universally accepted way of assessing readability, or a universal benchmark that is applied to health resources. However, the Tasmanian Department of Health and Human Services recommends that consumer health information should be targeted for grade 6 reading level or lower.21 Literacy levels also decline with illness, leading some US authors to suggest health information should be pitched a few grades lower than average to be understood by disadvantaged populations with chronic illness.11
We selected information and evidence-based asynchronous eMH services available online in Australia. On information sites, we chose the first page that described depression on each site. On interactive services, we logged in as a fictitious person and captured text from the depression programs up to the point requiring either payment or review by a human, along with the terms of use.
For comparison, we chose popular magazine titles available in a medical clinic waiting room, and found the most recent online article that specifically addressed depression. We also selected books with published readability scores that are likely to be recognised by Australians, but have somewhat archaic or foreign style, to reflect the complexity experienced by the non-medical reader of health information. On each web page, we stripped interface elements and rationalised punctuation to avoid inflated sentence-counts, and truncated long texts to approximately 3000 words.
We calculated Flesch–Kincaid Grade Levels (FKGL) and Simple Measure of Gobbledygook (SMOG) scores with the Readability Formulas website.22 Grade levels calculated from the FKGL or SMOG scores are commonly used in assessment of readability of health information.12 Both scores indicate the number of years of schooling after which an average US reader can understand the text, which approximate to Australian grade levels.23
Human research ethics committee approval was not required as only previously published material was considered in this research.
Results
We assessed common eMH resources, texts of varying readability and popular articles in print media about depression (Table 1).
| Table 1. Readability of selected e-mental health resources and popular literature |
| Source/author |
Title |
FKGL* |
SMOG* |
| This Way Up |
Terms of use |
16.6 |
13.4 |
| myCompass |
Terms of use |
15.3 |
13.5 |
| MoodGym |
Terms |
14.6 |
12.9 |
| Fyodor Dostoevsky |
The Brothers Karamazov, chapter 1 |
13.7 |
11.3 |
| MindSpot |
Terms of use |
12.9 |
11.6 |
| Beyond Blue |
Signs and symptoms of depression |
12.9 |
11.6 |
| Victor Hugo |
The Hunchback of Notre Dame† |
12.0 |
— |
| SANE |
Depression |
12.7 |
11.8 |
| myCompass |
Depression further reading |
12.7 |
11.7 |
| E-couch |
How is depression diagnosed? |
12.6 |
12.6 |
| BITE BACK |
Terms of use |
11.1 |
11.1 |
| ReachOut |
What is depression? |
11.0 |
10.2 |
| Nathaniel Hawthorne |
The Scarlet Letter† |
11.0 |
— |
| MoodGym |
Why you feel the way you do |
10.9 |
11.6 |
| Emily Brontë |
Wuthering Heights† |
10.0 |
— |
| MindSpot |
About low mood and sadness |
9.7 |
9.6 |
| MindSpot |
Helpful information |
9.4 |
9.0 |
| Men’s Health magazine |
Dwayne ‘The Rock’ Johnson opens up about his struggles with depression |
9.3 |
9.0 |
| This Way Up |
How to deal with depression and sadness |
9.3 |
9.4 |
| Bram Stoker |
Dracula† |
9.0 |
— |
| Black Dog Institute |
What is depression? |
8.7 |
8.9 |
| Head to Health |
Depressive disorders |
8.7 |
8.8 |
| MindSpot |
Depression quiz |
8.6 |
8.6 |
| Sydney Morning Herald |
Nearly one in 10 Australians take antidepressants.
Are there other solutions? |
8.3 |
8.1 |
| headspace |
Understanding and dealing with depression |
8.2 |
8.4 |
| Charles Dickens |
Great Expectations† |
8.2 |
— |
| Youth Beyond Blue |
Depression |
8.1 |
8.4 |
| LM Montgomery |
Anne of Green Gables† |
7.5 |
— |
| Kenneth Grahame |
The Wind in the Willows† |
6.4 |
— |
| Lewis Carroll |
Alice’s Adventures in Wonderland† |
5.5 |
— |
| Dolly magazine |
How to deal with depression |
5.2 |
6.3 |
| Anna Sewell |
Black Beauty† |
4.2 |
— |
| Dr Seuss |
Oh, the Places You’ll Go |
1.8 |
3.3 |
*Values shown for FKGL and SMOG represent the number of years of schooling required for an average reader to understand the text.
†Values for selected literature were taken from Flesch–Kincaid Grade Levels as listed on the Lit2Go website.34
FKGL, Flesch–Kincaid Grade Level; SMOG, Simple Measure of Gobbledygook; —, Measures not available |
Discussion
Nearly all the eMH resources we sampled needed sufficient literacy to read Great Expectations, a grade 8 text. It is troubling that to read the terms of use pages within the eMH resources that we sampled required a university education. We speculate that the trials of these resources used similar documents to obtain consent for research participation and wonder whether the participants adequately understood the consent, or whether this barrier excluded participants with average or lower literacy from the studies.
However, text readability is not the only issue for people accessing eMH resources. Online resources add cognitive tasks to the processing of text. Readers must distinguish the content from navigation and contextual elements on the page, intuit how the interface elements behave, and build a mental model to locate information. In addition, many webpages are visually crowded with brand signifiers and links to distractors: internet literacy includes habits of focusing attention away from these. We expect that the cognitive slowing experienced by people with mental health disorders may make these tasks even more difficult.
Are e-mental health resources the wire monkeys of our generation?
A recent qualitative metasynthesis suggests eMH currently offers privacy and a sense of control that people value, but that it lacks the elements of support and interconnectedness that face-to-face services offer.24 However, there is potential for therapeutic relationships to be part of internet-based therapies, and some programs do incorporate personal support (eg MindSpot). There is some evidence that technology-mediated therapeutic relationships can be just as effective as face-to-face services, so there is potential for telehealth and other forms of therapeutic connection.25 Of course, patients supported by clinicians (general practitioners [GPs], rural and remote nurses, Aboriginal Health Workers and others) may use internet-based resources as a supplement to care, rather than a main focus.
In 1958, Harlowe described baby rhesus monkeys reared with surrogate mothers made of wire and wood (Figure 1). Despite being adequately fed, the monkeys had a lack of maternal attachment.26 Since the 1950s, we have become increasingly aware of the importance of attachment, not just in families, but also in therapy. Balint famously described the therapeutic relationship as ‘the drug, doctor’ in his early work in the 1950s.27 Since then, the evidence for the importance of the therapeutic relationship in mental health has mounted, and it has arguably the strongest evidence for therapeutic interventions in mental healthcare.28–30 Therapeutic relationships are particularly important to survivors of trauma,31 and unfortunately childhood trauma is common,32 particularly in marginalised communities.33 Therapeutic relationships take time to deepen and cannot be outsourced to multiple providers without a loss of attachment. Given the evidence regarding the importance of the therapeutic relationship, it appears that excluding it from the delivery of therapy is not wise.
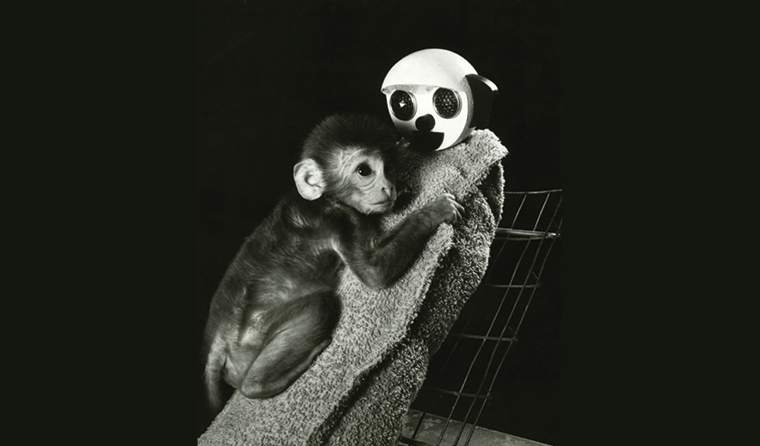
Figure 1. Harlow’s wire monkey experiments
Implications for general practice
There is evidence that eMH programs provide symptom relief for some patients and some mental health conditions. However, eMH programs may exacerbate the treatment gap for disadvantaged patients because of inherent high literacy requirements. When these resources are prescribed in general practice, the literacy and resources required to use them need to be considered, particularly when patients are cognitively impaired because of illness. Other alternative forms of patient education may be more useful for disadvantaged patients, and may include face-to-face discussions over time.
Future research into eMH should specifically include participants with differing levels of English literacy to enable policy makers to make informed decisions about equitable access to mental health services. It is recommended that researchers use consenting processes that do not exclude people with low English literacy. Such trials would ideally include participants from a range of demographic groups and report the outcomes against these population characteristics.
Conclusion
By using eMH as a policy solution, we may be creating an illusion of access while perpetuating disadvantage. Availability does not guarantee accessibility. eMH resources may well be helpful for a subset of patients who have high literacy. Unfortunately, this is not the group in most need of services.
There may be a greater role for clinician-mediated and peer-mediated support and psychoeducation available to disadvantaged communities through technology-enabled systems (such as telehealth). However, if we are to meet the needs of diverse communities, we need the flexibility to adapt our interventions in culturally sensitive ways. That may include removing the device from the conversation.
We need to be clear what text can and cannot do. Those people in our community who cannot decipher Dickens still deserve care.