The term ‘general practitioner with special interest (GPwSI)’ refers to a GP who functions as a clinical intermediary between primary, secondary and tertiary care.1,2 The role originated in the UK as part of a workforce strategy that aimed to decrease the burden on specialist services and improve patients’ access to specialist care.2–6 Since 2000, a number of countries, including the UK, Netherlands, Canada, Australia and New Zealand, have introduced GPwSIs into their health services, with significant heterogeneity of the role, competency framework, performance management and formal assessment.7–9 To properly understand the role, impact and potential of the GPwSI, the authors undertook an integrative review, particularly appropriate for the topic as the emerging body of literature includes a diverse range of empirical studies.
Methods
Overview
In contrast to a systematic review, which addresses a specific clinical question, an integrative review synthesises a diverse range of literature (both qualitative and quantitative) to provide a comprehensive understanding of the phenomenon of interest.10 To maintain a rigorous review process, this integrative review was conducted using the five steps outlined by review guidelines:10 problem identification, literature search, data evaluation, data analysis and presentation. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used for all applicable items.
Sample and inclusion criteria
A lack of understanding of the definitions, roles, locations and outcomes of the GPwSI was the problem this integrative review addressed. From it, the review question, ‘What is currently known about GPwSI?’ was developed using the SPIDER tool (Sample, Phenomenon of Interest, Design, Evaluation and Research type).11 Studies were included if: 1) an aspect of the study described the work of the GPwSI (ie described GPs with additional training or extended scope of practice); 2) the study examined how GPwSIs provide services to patients, including context, roles and outcomes; and 3) the study was empirical, full-text and in English.
Although the term ‘GPwSI’ was first coined in 2000, studies were not excluded on the basis of their year of publication because of the presence of GPwSI-type roles prior to the official terminology. Additionally, studies conducted prior to 2000 aid in understanding the history and evolution of GPwSIs. Studies prior to 2000 were included if they discussed a specialised GP role that was outside the scope of usual practice. Studies were excluded if they focused on hospital clinicians, settings or subspecialties.
Literature search
A systematic literature search was conducted between May 2017 and July 2018. A health librarian aided the literature search. Databases searched included MEDLINE, PubMed, Cumulative Index of Nursing and Allied Health Literature (CINAHL) and SCOPUS. Boolean connectors AND, OR and NOT were used to combine search terms. Medical subject headings (MeSH), were used in the execution of PubMed and MEDLINE database searches. Search terms relating to GPwSIs included: ‘General Practitioner’, ‘GP’, ‘Primary Care Physician’, ‘Primary Care Doctor’, ‘Generalist’, ‘Family Physician’, ‘Physicians, Family’, ‘GPwSI’, ‘Family Medicine’, ‘Special Interest’, ‘Specific Interest’ and ‘Subspecialty’. All database search results were imported into EndNote for screening.
A systematic grey literature search was conducted during December 2017 and January 2018. Databases searched included WorldCat, BASE and Google. Additionally, government websites, such as the National Health Service of England, were searched for relevant information. For large databases, results from the first five pages of the search were imported into EndNote for screening. Reviewing the first five pages was done because of the large number of results and the decline in relevance after the initial pages.
Screening and data extraction
The title and abstracts of all papers identified by the search were screened in duplicate by three researchers using the inclusion and exclusion criteria. Studies that appeared to meet the inclusion criteria on the basis of their titles and abstracts were retrieved for further review and screened in duplicate by the three researchers. Any disagreements in screening were resolved by discussions between the researchers. Data extracted included: title, author, year published, aim, methods, results and key findings that related to GPwSI. To support accuracy, one author extracted all data and two other researchers who were familiar with the included studies carefully reviewed the data extraction table.
Data analysis
This integrative review included both qualitative and quantitative studies, which were analysed thematically using meta-synthesis. Meta-synthesis is an integrative interpretation of results to offer a novel finding.12 Data analysis involved iterative comparison of studies to cluster recurrent themes and sub-themes.10 All authors participated in data analysis. Findings of all studies were independently read and re-read, coded and organised into categories, which were then compared across studies to identify relationships and themes.10 This process continued until data saturation was achieved, and no new themes emerged.
Results
Descriptive findings
A total of 59 articles were included in the review from a total of 1501 screened articles, as described in Appendix 1 and shown in Figure 1. All studies were published between 1992 and 2017. Of the published literature, studies were conducted in the UK (n = 36), Australia (n = 8), the Netherlands (n = 2), Canada (n = 1) and New Zealand (n = 1). The studies had a wide range of methodological designs. Qualitative studies (n = 3) included interviews and/or focus groups.4,6,13 Quantitative studies (n = 22) included surveys,14–17 cohort studies,18 retrospective and prospective observational studies,19–32 randomised controlled trials33,34 and experimental design.35 Two studies had a mixed methods design.36,37 Two studies were systematic literature reviews.1,38 Nineteen publications were professional opinion articles or essays.2,3,5,9,39–53 The grey literature results (n = 11) included journal articles not listed in a journal database,54,55 guidelines,8,56–58 reports,59–61 a medical appraisal62 and an example portfolio.7
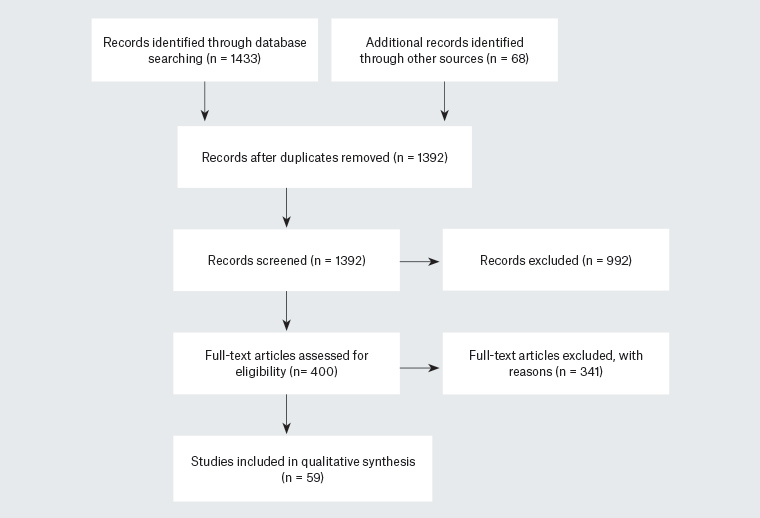
Figure 1. Study selection process
Five studies examined the history and evolution of GPwSIs.1,13,15,45,48 Eight studies measured clinical outcomes.20,23,27,30,31,33,35,36,40 Five of these studies examined measurable clinical outcomes and surveyed patient satisfaction.20,23,33,35,36 One study exclusively studied clinical outcomes in terms of the efficacy of a procedure.30 One study compared clinical outcomes of patients of GPwSIs to specialists.27,31 One paper discussed clinical outcomes in terms of a potential model of care.40 Five studies examined the efficacy of GPwSIs. One of these studies examined referrals that could be appropriate for GPwSIs in certain specialist fields.32 Four of these studies compared GPwSI treatment decisions in comparison to non-GP specialists.14,16,19,24
One study directly measured the cost-effectiveness of GPwSIs.21 One study did not have GPwSIs as the subject of the paper, but the participants.29 This study focused on new tools and methods for improving care provision. Seven studies examined the advantages and disadvantages of GPwSIs.4,5,9,39,41,43,46,52 Ten studies examined potential models of integration for implementing GPwSIs. Three of these studies examined potential policies for implementing GPwSIs,17,50,60 and seven studies examined potential future roles of GPwSIs.6,25,26,28,36,42,53
Meta-synthesis
Three themes were discovered inductively from the literature: 1) diversity in settings, conditions and roles; 2) superior patient satisfaction and comparable outcomes to non-GP specialists; and 3) need for greater workforce clarity or regulation.
Diversity in settings, conditions and roles
The first theme captured the diversity of the GPwSI role within healthcare systems. The literature included examples of GPwSIs operating in independent clinics,20,37,40,50 hospital outpatient departments,27 as a part of specialist teams, or as a part of primary care teams.1,15,23,48,53 Remuneration was also diverse, including fee-for-service,43 salary or uncontracted.15,48,49,52,60 GPwSIs provided care to patients with a variety of health conditions. The most commonly reported were in respiratory, dermatology, palliative and neurology care.
The duties described of GPwSIs were also diverse, ranging from clinical roles, giving opinions (including educating other healthcare professionals),1,3 performing specific procedures,1,3,49 and leading and developing services.3,50,52,55,60 In hospital settings, GPwSIs were found to take on roles that were previously fulfilled by registrars or junior doctors.32,34,47 Several examples were found of GPwSIs focusing only on their specialist duties, while other studies described cases of GPwSI integrating their extended role into their ongoing general practice duties.47
Superior patient satisfaction and comparable outcomes to non-GP specialists
The second theme related to the clinical and economic impacts of the GPwSI. Studies found that patients tended to be more satisfied with GPwSI services when compared with traditional hospital or specialist clinics.23,27,33 This was attributed to increased convenience and shorter waiting times.1,5,15,23,28,33,52 Additionally, GPwSIs were found to achieve comparable clinical outcomes to specialists.20,27,33,34,38 They also reduced the burden on specialists.5,9,23,33 In cases where GPwSI care resulted in poorer outcomes than specialist care, the role of the GPwSI was either not well defined or not regulated.14,16,31
Three studies examined the cost-effectiveness of GPwSIs.21,34,52 One study published in 2009 estimated that a nine-month intervention using a single GPwSI to support allergy care saved the local health economy £13,580.21 A second study in 2005 assessed the GPwSI model as slightly more costly than hospital outpatient care, but enabled improved access for patients and resulted in similar health outcomes.34 A third article from 2003 was not original research, rather an opinion piece on the economic perspectives of the GPwSI, cautioning that these services could decrease efficiency of care, counterproductive to the aim.52
Need for greater workforce clarity or regulation
The third theme identified that the role of GPwSI is poorly defined in most countries. This may be attributed to the ad-hoc nature in which the role has developed. Early definitions were vague and did not refer to any particular training or specific role.1 While the UK’s 2000 National Health Service (NHS) plan was the first government initiative to formally implement GPwSIs into the healthcare system,1,3,15,36 it did not contain a clear definition of the GPwSI.9 GPwSIs could be trained by a specialist physician in the field of interest,39,48,50 or receive additional education during their medical education, or after completion of a degree.15,39,42 Regulation of training included routine, ongoing review to assure national quality standards were met.23,50 Online models of training were also proposed.5
The UK has expanded nationally accredited training requirements and audit practices for special interest fields beyond the traditional obstetrics, anaesthetics and emergency settings. Between 2007 and 2013, the Royal College of General Practitioners (RCGP) produced a number of frameworks that set out the competencies, educational attainment and service provision considered important for the commissioning of a GPwSI. From 2015, the RCGP has renamed the GPwSI as a ‘GP with extended role (GPwER)’.56,58 This reflects the need for greater clarity of the role, and commitment to ongoing training, support, mentorship and review.58
Discussion
The past 15 years have witnessed an escalating interest in the role of the GPwSI in Australia and other countries. The Royal Australian College of General Practitioners’ (RACGP’s) Faculty of Specific Interests numbers >17,000 Fellows across 29 Specific Interests Networks;63 universities offer advanced special interest diplomas;64 and Queensland Health currently employs 48 GPwSIs in areas as diverse as general surgery, dermatology, neurology, gastroenterology, orthopaedics and gynaecology.
This review was undertaken to learn from international evidence regarding the role and its impact, allowing Australian practitioners and employers to maximise optimal employment of and support for the GPwSI within our healthcare setting. Our review shows significant heterogeneity of both role and impact. It also provides a warning regarding appropriate training, mentoring and ongoing professional development for GPs and employers adopting this role. Based on our findings, such ongoing professional support is essential to maximise both quality and impact.
In the UK, the RCGP and NHS England have recently partnered to support and further formalise the GPwSI role as the GPwER.58 This has been in response to the implementation of new models of care such as Multispecialty Community Providers, and Primary and Acute Care Systems, which require increased capacity-building within general practice. The GPwER is a GP who undertakes, in addition to their core general practice, a role that is beyond the scope of the Membership of the RCGP, requiring further formalised training. The RCGP has developed a consistent framework, accreditation and revalidation process to show ongoing competency and support, and is currently trialling a demonstration module to test the key principles. This may be of interest and importance for Australian clinicians.
The study has several potential limitations. The range of international terms and acronyms used to describe the GPwSI was broad. In order not to miss relevant information, we were inclusive of any role that placed a GP between primary and secondary care. Although we are confident we thus identified all relevant papers, most studies identified were at the lower end of the evidence hierarchy. Finally, the bulk of experience with the GPwSI role comes from one country – the UK – where GPwSIs are well integrated into the healthcare system.
Conclusion
The GPwSI/GPwER workforce model will continue to attract ongoing interest as healthcare reform internationally requires increased community management and complex chronic disease care close to home. This review summarised the current international evidence relevant to the role. It highlighted large diversity in the settings, conditions and roles of GPwSI, with superior patient satisfaction and comparable outcomes to non-GP specialists. In the current environment, there is a clear need to more closely examine the many settings in which the role can improve both patient care and more efficiently use scarce health resources. There should also be a focus on greater workforce clarity and ongoing monitoring and review to ensure optimal service provision. Further research to rigorously evaluate the impact of GPwSIs on service delivery outcomes, access and costs, compared with traditional care, should be a health service research priority.
Appendix 1