Background
The benefit of exercise in the prevention and management of type 2 diabetes (T2D) has a strong evidence base, so it is important to ensure exercise is part of every patient’s management plan.
Objective
This article reviews the evidence for exercise in T2D and the factors affecting a patient’s willingness to commence and sustain enough exercise to gain benefit. The article offers tips about how to safely and effectively prescribe the ‘medicine’ of exercise for all, even the frailest patients; who to stabilise before an exercise program should begin; and how to use the skills of an accredited exercise physiologist (AEP) to deliver the best ‘prescription’ possible.
Discussion
General practitioners and their teams, along with other healthcare providers such as AEPs, can increase the amount of exercise medicine a patient receives. This is the case for those at risk of developing T2D, those with T2D and those with the many comorbidities associated with T2D.
Physical inactivity is the fourth leading risk factor for global mortality.1 Substantial research supports the benefits of regular physical activity for the prevention and treatment of chronic medical conditions.2,3 Patients who are insufficiently active cost more to care for,4 and a 2016 report conservatively estimated that physical inactivity cost the Australian health system over $800 million in 2013.5 Yet despite the substantive evidence, 85% of adult Australians participate in insufficient levels of physical activity to meet current physical activity guidelines and obtain the major benefits of participation,6 including the prevention of type 2 diabetes (T2D).
The aim of this article is to review the evidence for including structured physical activity goals, often termed ‘exercise goals’, in all management plans for patients with, or at risk of developing, T2D. The article also discusses the barriers associated with beginning and maintaining regular exercise. Additionally, advice is offered on why, and how, to include allied health providers such as accredited exercise physiologists (AEPs) as part of the treating team to optimise the incorporation of exercise in a management plan.
Overview of evidence for exercise
The benefits of regular exercise for diabetes management are well understood, with structured exercise training associated with absolute reductions in glycated haemoglobin (HbA1c) of 0.67%,7 improvements in muscle strength by 38%,8 and reductions in cardiovascular risk factors such as blood pressure (systolic blood pressure: –5.6 mmHg; diastolic blood pressure: –5.5 mmHg) and waist circumference (–0.8%).9 Aerobic exercise has also been demonstrated to result in improvements in quality of life.10 Lifestyle counselling, including a combination of diet and exercise advice, can delay progression to T2D more effectively over a two-year period than treatment with metformin (–58% compared with –31%, respectively).11 Furthermore, reduced fitness has been shown to be an independent predictor of mortality for people with T2D, with similar increases in relative risk from reduced fitness regardless of body mass index (BMI).12 This suggests that the protective effect of higher fitness is independent of body weight and equally beneficial for people with a normal, overweight or obese BMI.
The general recommendations for the amount and type of exercise for people with T2D are to engage in at least 150 minutes of moderate-to-vigorous aerobic exercise per week, and 2–3 half-hour sessions of resistance (strength) exercise on non-consecutive days each week.13 Patients should exercise at least every second day to optimise the exercise-induced benefits on insulin sensitivity.14 While there is less evidence for balance and flexibility exercise in the direct treatment of diabetes and cardiovascular risk, these exercise modalities may benefit the management of comorbidities. Therefore, they are also recommended on 2–3 days per week, as they can assist in maintaining functional independence and reducing the risk of adverse events such as falls, particularly for older or frail patients, or when peripheral neuropathy is present.13 The intensity and subsequent stimulus for positive adaptation of any activity is relative to the current level of fitness of the individual engaging in the activity and, as such, must also be tailored to the specific requirements of the patient. A slow walk on a flat path may induce a moderate-intensity cardiorespiratory response in some patients, whereas others may need to walk up an incline or at a brisker pace to elicit the desired response. A good general guide to intensity that can be used to assist patients to gauge their level of activity is to use the ‘talk and whistle’ test. If a patient can whistle while exercising, the intensity can be considered low; if they can hold a conversation but do not have the breath to whistle, it can be considered moderate; if they are breathing too heavily to comfortably speak in sentences, the intensity can be considered vigorous or high. Many common exercise activities contain elements of multiple exercise modalities, and these can assist in achieving multiple goals. For example, yoga combines elements of resistance, balance and flexibility exercise. A range of activities that may be applicable to patients with T2D and the types of modalities involved in those exercises are included in Table 1. In addition to structured exercise, individuals with T2D are encouraged to increase their incidental physical activity (eg taking the stairs rather than an elevator at work) in order to gain additional health benefits.13 An overview of the benefits of different exercise modalities to individuals with T2D and associated comorbidities are outlined in Table 2.
| Table 1. Physiological components of common exercise activities |
| Exercise activity |
Aerobic component |
Resistance component |
Flexibility component |
Balance component |
| Yoga |
* |
** |
*** |
*** |
| Circuit training |
** |
** |
* |
* |
| Tai chi |
– |
* |
* |
** |
| Walking |
** |
* |
– |
* |
| Jogging/running |
*** |
* |
– |
* |
| Pilates |
– |
** |
* |
* |
| Cycling |
*** |
* |
– |
– |
| Dancing |
** |
– |
* |
* |
| Gardening |
* |
* |
* |
* |
| Weight training |
* |
*** |
* |
* |
*** Strong benefit, ** Moderate benefit, * Minor benefit, – No benefit
Note: The ratings here are estimates and will vary depending on the way any activity is prescribed and/or structured and how challenging it is based on an individual’s fitness level. For example, yoga can be structured as a very light-intensity activity or can be very high intensity depending on the sequencing and pacing of movements and the participant’s relative fitness. It is advisable for patients to discuss the specifics of any activity they are doing with their general practitioner and/or accredited exercise physiologist to determine if it is safe for them and likely to deliver the desired benefits. |
| Table 2. Effect of exercise modalities on health-related outcomes in type 2 diabetes |
| Health-related outcome |
Aerobic exercise |
Resistance exercise |
Flexibility exercise |
Balance exercise |
| Glycaemic control |
*** |
** |
– |
– |
| Cardiovascular risk reduction |
*** |
* |
– |
– |
| Mental health/mood |
*** |
* |
– |
– |
| Balance/proprioception |
* |
* |
** |
*** |
| Muscle strength |
* |
*** |
– |
* |
| Bone health |
* |
*** |
– |
– |
| *** Strong benefit, ** Moderate benefit, * Minor benefit, – No benefit |
Overview of factors associated with starting and maintaining an exercise program
Factors affecting a patient’s willingness to commence an exercise program include a patient’s previous exercise history, their understanding of the role of exercise in the prevention or treatment of diabetes, their expectations regarding the likely outcomes from regular exercise as well as their motivation to achieve these outcomes, their confidence to exercise in public and their confidence that it is safe to exercise. While the risk of an adverse event is elevated during exercise for patients with T2D, including those with comorbidities, the occurrence of adverse events is low with the benefits of regular exercise greatly outweighing the risks.15 Additional common barriers to starting an exercise program include lack of interest and perceived lack of fitness and energy as well as ingrained sedentary behaviours.16 The term ‘exercise’ itself may be a barrier to some individuals because of a lack of information from health professionals and a lack of knowledge surrounding exercise type and intensity that is safe and effective, as shown within cancer survivor populations.17 It may therefore be preferable to instead talk about movement or activity or specific tasks such as sitting less, moving more or taking part in activities such as gardening, for example. Ongoing exercise adherence is enhanced if it is goal-directed and caters to the individual preferences of the patient; therefore, part of the prescription process should be to identify patient goals and activities they enjoy (such as playing with their grandchildren) and to make these the focus of exercise prescription. The treating clinician can assist by using motivational interviewing skills with their patients to encourage change in their behaviour by focusing on the patient’s own motivating factors to experience the benefits of exercise.18
Role of the general practitioner
If referring a patient or recommending exercise, GPs have a role in screening those who are not currently suitable for an exercise program or need close supervision while undertaking exercise. Unsuitable patients include those with unstable angina, unstable respiratory disease, untreated heart failure or cardiomyopathy, severe aortic stenosis and uncontrolled diabetes. Once stabilised, these patients may be suitable for an exercise program. Patients who may need close supervision while exercising include those who have had a complicated myocardial infarct within the previous three months, those with a resting heart rate ≥100 beats/minute and those with poorly controlled hypertension.19 It is important to recognise that every clinically stable patient (including the very frail) can benefit from exercise tailored to their individual circumstances. As every patient is different, a single solution tailored purely to the primary morbidity is unlikely to work, and instead a holistic approach to prescription should be followed. For example, a patient who is frail may be prescribed similar exercise to one with the same conditions who is not frail but at a reduced intensity and with increased use of fall-prevention strategies. An individual who is morbidly obese might have a reduced focus on weight-bearing activity to reduce the risk of developing impact-related musculoskeletal problems. It is also important to recognise that any increase in level of physical activity, however small, is likely to be beneficial. Figure 1 provides a flowchart to assist with decision making to support patients to become physically active.
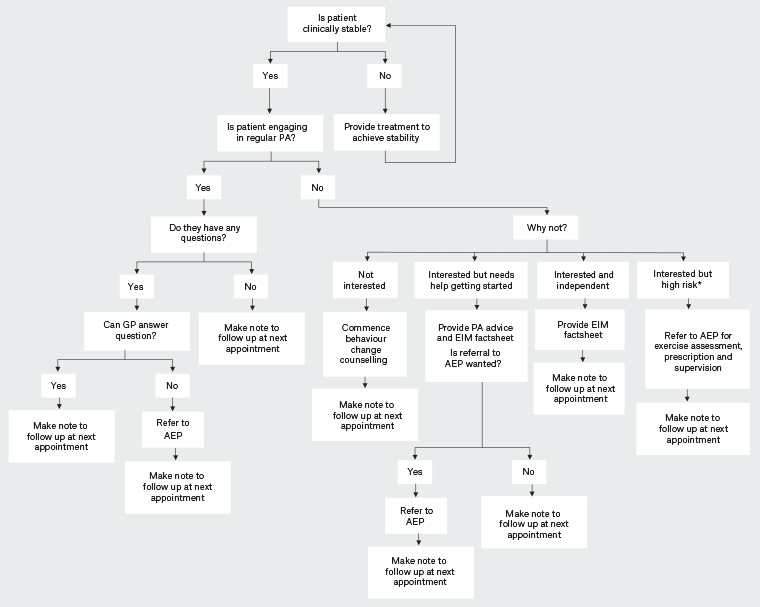
Figure 1. Decision-making aid to support patients to become optimally active
*High risk: risk of hypoglycaemia, morbidly obese, musculoskeletal limitations, severe mental illness or any other factor the GP thinks will complicate physical activity
AEP, accredited exercise physiologist; EIM, Exercise is Medicine; GP, general practitioner; PA, physical activity
Click here to enlarge
Several systematic reviews indicate that general practitioner (GP) advice and counselling related to physical activity leads to increases in physical activity participation by patients.20,21 Despite this evidence there may be numerous barriers to GPs delivering safe and effective exercise counselling. Barriers that have been identified to GPs initiating discussions about physical activity with their patients include feeling ill-prepared to offer specific advice about appropriate exercise types, frequencies and intensities, and perceptions of low patient motivation to change.22,23 Potential solutions to the barriers GPs experience in providing specific advice about appropriate exercise parameters include providing patients with existing resources related to exercise for people with diabetes such as an Exercise is Medicine factsheet (http://exerciseismedicine.com.au/factsheets) and the referral of patients to appropriately qualified health professionals24 for a specific exercise prescription and coaching in how to enact it.
Role of accredited exercise physiologists
AEPs are university-qualified allied health professionals trained in exercise prescription and behaviour change interventions for a wide range of clinical and sub-clinical populations. Through GP referrals, via a GP Management Plan or residential aged care facility plan, patients with diabetes can obtain up to five individual consultations and eight group sessions funded by the Medicare Benefits Schedule (MBS) with an AEP in a calendar year.25 On the basis of individual patient needs, the AEP can use these sessions to assess exercise tolerance, discuss goals, address barriers to support behaviour change, and prescribe and instruct safe and effective exercise. Importantly, AEPs are independent health practitioners with the clinical knowledge and skills to identify potentially significant signs or symptoms that may indicate a client is not clinically stable and requires further treatment before it is safe for them to exercise. AEPs can also identify situations in which safe thresholds for exercise to avoid signs or symptoms need to be considered (eg stable angina), eliminating the need for a GP to provide a potentially problematic clearance to exercise.26 For many patients without significant clinical symptoms requiring close supervision during exercise, transitioning to groups or the gym can be confronting. For these individuals, an initial referral to an AEP or physiotherapist may assist to facilitate a supported transition to independent group or gym exercising.
Referrals to group programs allow for an initial individual assessment by the allied health professional that is not considered part of the five individual sessions that can be provided as part of a Team Care Arrangement. Patients are then able to attend up to eight group sessions for between two and 12 patients each per calendar year. These sessions can assist allied health professionals to address lifestyle changes in a manner more likely to result in sustained behaviour change than may be achievable through the maximum of five individual visits. Primary care physicians can check whether there are group sessions operating in their area as this might provide extra care for the patient above the five one-on-one sessions per year. The Royal Australian College of General Practitioners’ Smoking, nutrition, alcohol, physical activity (SNAP) guideline has links to state-based programs;19 local Primary Health Networks may also be able to assist.
Despite these options, the long-term adherence to exercise programs is poor,19 so ongoing review of progress by treating allied health professionals and the general practice team is needed. Regular non-judgemental review with the patient can assist with identifying and addressing any barriers to exercise, and provides an opportunity for the GP to deliver follow-up coaching, while regular review of goals can assist the patient to maintain the motivation critical to sustained lifestyle change.27
Conclusion
Exercise is a safe and effective treatment modality to assist in the control of glucose levels and reduce complications for individuals with T2D. However, there are multiple challenges that must be overcome both for GPs and their patients to initiate and maintain regular exercise as part of a treatment plan. A referral to an AEP or physiotherapist for exercise counselling and prescription should be strongly considered as it can support and build on the behaviour change process initiated in general practice settings to enhance patient outcomes.
Key points
- Exercise should be discussed/prescribed for every patient with or at risk of T2D.
- Every patients who is clinically stable can benefit from exercise.
- Any increases in physical activity can be beneficial.
- All health professionals in the general practice team are ideally placed to discuss and provide an initial exercise prescription and to refer to an AEP or physiotherapist for a more detailed exercise prescription.
- MBS funding is available for the referral, and treatment with exercise, of patients with T2D.