Case
A man aged 85 years presented to his treating doctor for his annual skin examination. He had extensive sun damage and multiple previous basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs). Examination revealed a lesion on the posterior aspect of his right deltoid (Figure 1). The patient stated that the lesion had been present for decades and that he had not noticed any recent change in size or appearance.
The lesion was irregularly shaped, erythematous and slightly sunken, measuring 8 mm in diameter. It had a smooth surface with no scale and was firm to palpation. When squeezed between the thumb and forefinger, the lesion demonstrated a positive ‘delling’ or ‘dimple’ sign, characteristic of a dermatofibroma.1 Close examination revealed milia and erythema between 12 and 3 o’clock.
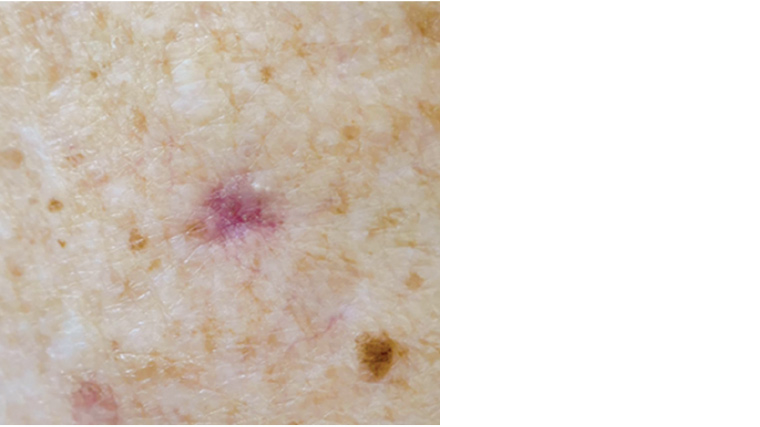
Figure 1. Clinical image of posterior right deltoid lesion
Question 1
Prior to dermoscopy, what is the differential diagnosis for this lesion?
Question 2
What are the features found on dermoscopy (Figure 2)?
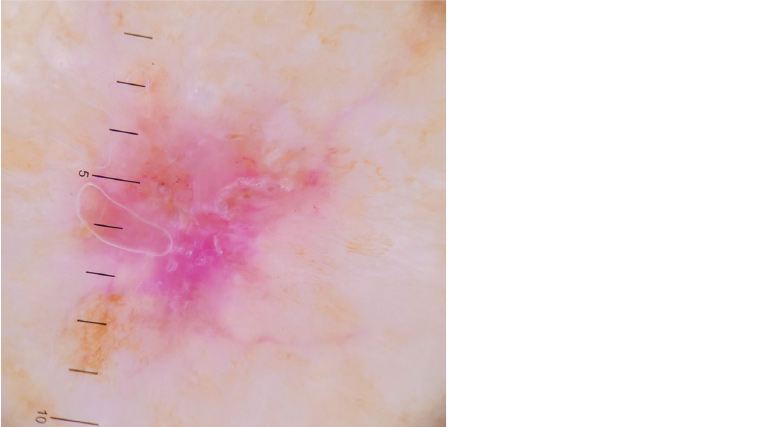
Figure 2. Dermoscopy image of posterior right deltoid lesion
Question 3
Combining the clinical and dermoscopic findings, what would be the most likely diagnosis?
Question 4
What is a dermatofibroma?
Question 5
How does a BCC arise from a dermatofibroma?
Question 6
What are the management options?
Answer 1
The differential diagnosis, ranging from benign to more sinister, includes:
- scar
- dermatofibroma
- BCC
- desmoplastic lesions including desmoplastic malignant melanoma and early dermatofibrosarcoma protuberans.
Answer 2
Dermoscopic features seen in Figure 2 include:
- linear and arborising telangiectasia
- scale and central ulceration
- possible deep milia versus cystic change
- translucent erythema
- brown pigment dots
- peripheral fine lentigo-like pigment network
- white, fibrotic centre
Answer 3
At first glance, the lesion may appear to be an inflamed dermatofibroma; however, when combining the historical, clinical and dermoscopic features, it is clear this is an atypical lesion. In this case, the diagnosis of a BCC arising in conjunction with a dermatofibroma can be made.
On gross clinical examination, features of a BCC include the lesion’s irregular shape, localised translucent erythema and milia-like cysts.2 Further, dermoscopic findings 1–5 (as listed in Answer 3) are consistent with a BCC, while findings 6 and 7 are in keeping with a dermatofibroma.1–4
Answer 4
Dermatofibromas are common benign fibrosing cutaneous lesions occurring within the dermis and occasionally subcutis.1,5 They are hypothesised to be either a neoplasm or reactive process arising from arthropod bites or trauma. The lesions are seen primarily in adults and can develop anywhere on the body, most commonly on the lower extremities.1,6,7 Clinically, dermatofibromas appear as firm papules, nodules or plaques, ranging from a few millimetres to 2 cm; they can be atrophic, as seen in this case, and are coloured from pink or purple-red to shades of brown.3,5 The lesions consist of nodular dermal proliferating spindle-shaped fibroblasts and myofibroblasts.1
Typical dermoscopic features of a dermatofibroma include peripheral light-brown pigment networks, central irregular white scar-like patches, white networks, homogenous pigmentation, vascular-like structure, dots and globule-like structure, related to hyperpigmented rete ridges.3,5
Answer 5
Both BCC and reactive basaloid cell hyperplasia (BCH) in the context of dermatofibromas represent proliferation of germinative basaloid cells.8 While some authors speculate that these processes belong on the same pathological continuum, others argue that BCC-like changes in dermatofibromas lack malignant potential.8,9 There are case studies of true BCCs overlying dermatofibromas, a rare co-presentation of two common conditions, and this can potentially be mistaken for BCH.8,10,11 Case reports also document the association of other malignant lesions, such as SCCs and melanomas, with dermatofibromas.12,13
Answer 6
Management of this lesion is determined by the fact that it is atypical and contains features highly suspicious for malignancy.
If the clinician were confident in the diagnosis of a BCC arising in a dermatofibroma, surgical excision with direct closure would confirm the diagnosis and cure the lesion in a single visit, given clear post-operative margins.2 For a lesion of this size and location, definitive excision carries little risk of poor cosmetic or functional outcomes.
Alternatively, if the clinician is unsure of the diagnosis but recognises that this is an atypical dermatofibroma, an initial biopsy before definitive treatment would be a reasonable approach. To avoid sampling error, which may miss the diagnosis of the BCC, the biopsy should be guided by clinical and dermoscopic examination and be of sufficient size to give the pathologist a definitive sample. A punch biopsy ≥3 mm, or a deep and wide shave biopsy is recommended.3
In this case, histopathology revealed a solid BCC and dermatofibroma with clear margins, as seen in Figure 3. Complete excision in the first instance meant that no further treatment was required.
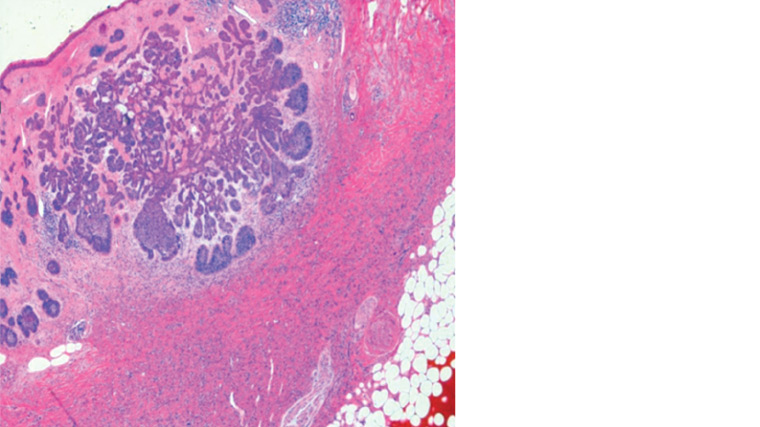
Figure 3. Basal cell carcinoma and dermatofibroma histological slide stained with haematoxylin and eosin
Key points
- Dermatofibromas and BCCs are common lesions with distinctive clinical and dermoscopic features. However, their co-existence within one lesion is uncommon.8
- Dermatofibromas can be associated with a variety of malignancies, including BCC, SCC and melanoma. Therefore, any suspect historical, clinical or dermoscopic findings or changes in a previously benign dermatofibroma should prompt further investigation.8,12,13
- Careful clinical examination and dermoscopic assessment of an atypical dermatofibroma are key to guide the diagnosis of a BCC occurring in conjunction with a dermatofibroma.
- Recommended management of a BCC arising in a dermatofibroma is complete excision; however, if this is not possible, an initial punch or wide and deep shave biopsy guided by dermoscopy is reasonable.2