Abortion is a common experience for women globally. In Australia, 16% of women have had an abortion by the age of 34 years.1 While both surgical and medical methods of abortion are available in Australia, they can be difficult to access, with many women travelling long distances2 or interstate3 and incurring high out-of-pocket costs3,4 to receive abortion care. Provision of medical abortion in general practice can improve access to abortion care. General practices tend to be more proximal than tertiary centres and frequently visited by women,5 particularly for assistance with pregnancy and family planning issues.6 There is evidence that women prefer to receive their abortion care from a known health provider, such as a general practitioner (GP).7 GPs are also well placed to provide other related services such as contraceptive care. Thus, GPs are ideally positioned to provide medical abortion in the community setting.
Currently, medical abortifacients in the form of MS-2 Step (mifepristone and misoprostol) are available for GPs to prescribe under the Pharmaceutical Benefits Scheme in all Australian states and territories excluding South Australia (SA).8 In SA, abortions must occur on hospital grounds, not in a general practice.8 MS-2 Step can be prescribed at up to nine weeks’ gestation. For a GP to legally prescribe medical abortion, they are required to undertake mandatory certification through online training (available at www.ms2step.com.au/register).
Although no nationwide data exist, it appears that some Australian GPs are willing to provide medical abortion but do not.9 Evidence suggests that lack of training, lack of support, fear of or actual stigmatisation and fear of demand are key barriers to GPs establishing and providing medical abortion services, both internationally and in Australia.10–14 Uncertainty regarding how to establish provision of medical abortion in a clinical setting is another cited concern.13,15 Describing an exemplary GP medical abortion delivery model may therefore facilitate commencement of practice and empower GPs to start delivering medical abortion.
Previously, Australian medical abortion models have described nurse-led models in which nurses provide most of the counselling, administration and follow-up tasks that comprise provision.16,17 These nurse–GP models,16,17 known as ‘task-sharing models’, have been successfully implemented in community healthcare settings where specific funding is available for those nurses. However, there has not been the same focus on how to implement and sustain medical abortion service delivery in the general practice setting. The aim of this study was to describe models of medical abortion care and to gain insights from current GP medical abortion providers as to how to establish and sustain medical abortion service delivery.
Methods
A qualitative descriptive approach was taken to describe medical abortion models of care used by current GP providers within the general practice setting. To guide the study design, the researchers used a quality framework for Australian general practice proposed by Booth et al18 comprising six dimensions (acceptability, accessibility, appropriateness, efficiency, effectiveness and safety) to better understand the various facets of medical abortion delivery in Australian general practice.
Ethics
Ethics approval was granted by Monash University (MUHREC project ID 18852).
Recruitment and consent
Recruitment followed purposive sampling and snowballing
because of the low numbers of current GP medical abortion providers. Current GP medical abortion providers were recruited between June and August 2019 via three strategies:
- online advertisement on a private Australian medical abortion providers special interest Facebook group
- mail out of invitations to any practice with a GP medical abortion provider listed on the Victorian reproductive health service directory (1800myoptions)19
- referral of medical abortion providers by interviewees, who were asked to pass on the investigator’s details to any known GP medical abortion providers.
Those interested in participating emailed one of the authors (SD, a female medical honours student). Written or verbal consent was obtained, and interview times were subsequently arranged.
Data collection
Demographic details collected included the state and remoteness of medical abortion provision, length of time the GP has provided medical abortion in general practice, age, sex and practice(s) billing type. The six dimensions of the quality framework18 underpinned the semi-structured interview guide, and two pilot interviews were completed. The final interview guide (Appendix 1, available online only) examined how providers established provision, medical abortion model structure, engagement of other clinicians, acceptability, improvements and advice to a colleague. Audio-recorded telephone interviews were conducted by SD. Sampling continued to 25 participants to confirm data saturation.
Data analysis
Interviews were transcribed verbatim and corrected by SD. Data were stored and managed in NVivo 12. Coding of data was completed by two researchers (AKS and SD) using thematic analysis.20 AKS and SD coded five transcripts and then discussed coding discrepancies to create a final coding scheme. SD used the final coding scheme to code remaining transcripts. Following coding, consensus of findings occurred between all three researchers (SD, AKS and DM). The Booth et al18 framework was then used to interpret themes.
Results
Twenty-five participants from 24 practices were interviewed (Table 1). Interviews ranged in duration from 18 to 70 minutes.
| Table 1. Participant demographics |
| Characteristic |
Number of participants |
| Sex |
|
| Female |
18 |
| Male |
7 |
| Age (years) |
|
| 30–39 |
13 |
| 40–49 |
9 |
| 50–59 |
2 |
| ≥60 |
1 |
| State/Territory |
|
| Victoria |
13 |
| New South Wales |
4 |
| Queensland |
4 |
| Tasmania |
2 |
| Northern Territory |
1 |
| South Australia* |
1 |
| Remoteness of practice† |
|
| Metropolitan |
12 |
| Regional |
11 |
| Rural |
0 |
| Remote |
2 |
| Years providing medical abortion |
| <1 year |
6 |
| ≥1 but <2 years |
6 |
| ≥2 but <3 years |
3 |
| ≥3 but <4 years |
5 |
| ≥4 but <5 years |
3 |
| ≥5 years |
2 |
| General practice clinic billing type |
| Private |
12 |
| Bulk billing |
6 |
| Mixed |
7 |
*Participant from South Australia provides medical abortion in both general practice and hospital settings, as participant works in a general practitioner–run hospital
†Remoteness of practice was collected from the health workforce locator tool using the Australian Standard Geographical Remoteness Areas (ARIA) 2016 classification32 |
General practitioner models of medical abortion care
Most participants used one of three models of medical abortion provision: common, streamlined or ultrasonography-inclusive (Figure 1). A fourth model – task-sharing, in which GPs and nurses collaborated to provide medical abortion – was used by five participants primarily in the community practice setting, not in private practice. Two of the five participants were also using additional, non–task sharing models in their private practices. However, only the common, streamlined and ultrasonography-inclusive models are covered in this article.
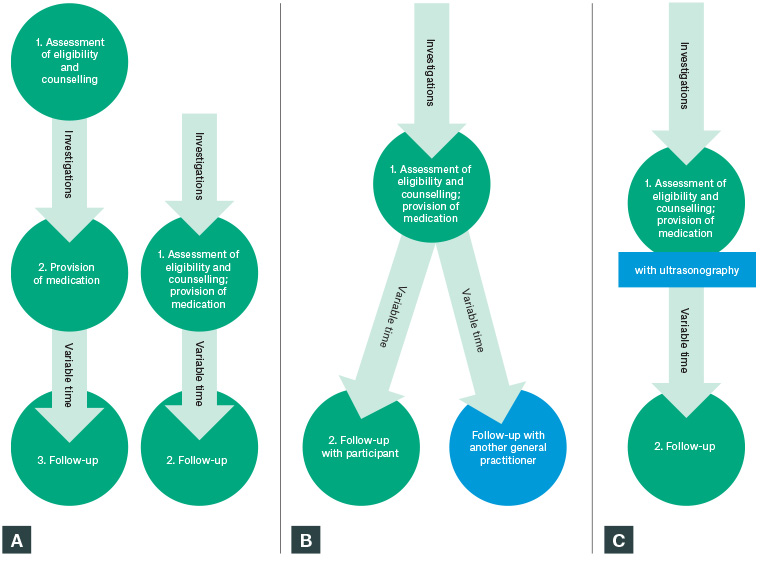
Figure 1. Diagram of three models of medical abortion delivery in general practice
A. Common; B. Streamlined; C. Ultrasonography-inclusive
Green circles represent patients’ appointments with participants and tasks conducted within appointments; arrows represent medical abortion provision processes completed outside of provider appointments. Investigations can include blood tests such as haemoglobin, quantitative human chorionic gonadotropin and blood group; ultrasonography; and chlamydia and/or gonorrhoea urine testing. ‘Variable time’ represents the time between provision of medication and follow-up, which varied between three days and three weeks.
Model 1: Common
The common model (Figure 1A), used by 17 participants, involved either two or three appointments, dependent on whether appropriate investigations had been obtained prior to or at the first appointment. Ultrasonography was completed by community radiology, with only one participant not routinely requesting ultrasonography for medical abortion eligibility. Although the length of time between medication provision and follow-up appointments varied (three days to three weeks), most participants sought to implement in-clinic follow-up at two weeks post–medical abortion prescription.
Model 2: Streamlined
Streamlined models (Figure 1B) had two appointments maximum. Although Model 2 appears similar to Model 1, which can also have two appointments, the streamlined model required the involvement of other GPs in order to minimise appointments with the medical abortion provider. Streamlined model patients were referred to the GP with investigations already completed and/or were referred back to the patient’s original GP for follow-up. Referrals occurred from within the participant’s clinic, other local GPs or external organisations (eg family planning services). Participants chose external GP follow-up to decrease costs, avoid obstructing pre-existing GP–patient relationships and minimise patient travel.
Model 3: Ultrasonography-inclusive
Four participants from four different clinics used this model, performing ultrasonography themselves in-clinic (Figure 1C). Participants chose to perform ultrasonography as a result of limited sonographer access or a desire to deliver comprehensive medical abortion services.
General practitioner insights into establishing a medical abortion service
Communicating initiation of delivering medical abortion
Many participants were deliberate in communicating medical abortion initiation to their workplace to seek support from employers or to notify clinic staff of this new service. Contrastingly, two GPs intentionally did not communicate their decision because of fears that the practice would restrict their ability to provide medical abortion:
I essentially operate by stealth; women will find me … I would absolutely not recommend that approach [communicating decision to colleagues] in the setting that I’m in now, because there would be a reason to obstruct my practice. (Participant [P] 18)
Many participants who had communicated their decision to commence medical abortion delivery in their practice simultaneously restricted advertising of the service. They did this out of fear and stigma:
[Y]ou don’t want to put yourself at risk of maybe being targeted by any anti-abortion campaigners if you’re too visible. (P11)
Providers’ networks
Establishing a network of external clinicians to support medical abortion delivery in general practice was seen as a critical step to commence medical abortion service delivery. A basic provider’s network included a pharmacist, sonographer and the MS-2 Step 24-hour nurse hotline.
Efficient medical abortion delivery could not occur without a pharmacist. Most participants contacted a local pharmacy and requested that they become dispensers of MS-2 Step. Only one participant had a local pharmacy that would not dispense. Efficiency was also increased by participants establishing a relationship with local radiology:
[B]y having a relationship with the radiographer ... to make sure they know … they’ll always squeeze [women in] soon … (P18)
Participants used the MS-2 Step 24-hour nurse hotline and hospitals (emergency departments [EDs] and/or obstetrician-gynaecologists) to improve safety. The nurse hotline number was perceived as enhancing support for patients and reducing the burden of after-hours follow-up. Contrastingly, hospitals were less commonly used, and some participants perceived communication with hospitals as a courtesy, rather than vital to medical abortion provision:
I did not [communicate with local hospital] primarily … I was aware that if the patient required to go to ED, their duty of care meant they would have to provide that care anyway … (P7)
Participants used various communication methods to create their clinician networks, including telephone, letters, specific terminology on radiology forms (eg ‘confirm location and gestation patient considering termination of pregnancy [TOP]’) and use of online directories (eg MS-2 Step pharmacist directory).
Medical abortion provider community
All participants spoke of the support they received from networks comprising other medical abortion providers. Many participants had other providers in their practice, which commonly motivated colleagues or participants themselves to initiate medical abortion provision. However, knowledge of local provision by another practitioner did discourage medical abortion provision for one participant as they perceived medical abortion was already accessible in their area of practice.
Medical abortion providers networked through local GP events, conferences or, most commonly, online using a private medical abortion provider Facebook group.
The medical abortion provider community enhanced medical abortion delivery through colleagues covering another’s medical abortion provision when on leave, as well as providing support, advice and education:
[I]t’s [the Facebook group] a very supportive environment and a good way for people to access the, I suppose, the breadth of information that you might not get if you were practising in your own silo. (P17)
However, one participant queried the actual benefit of a group that is not easily accessible.
Additional considerations for medical abortion delivery
Use of anti-D
Sourcing anti-D was perceived as difficult, especially when initiating medical abortion provision. Options for sourcing anti-D included pathology services, blood banks, specialised women’s health clinics and, for one participant, delivery from the local hospital. However, once established, some found anti-D provision ‘streamlined’ and simple.
Those unable to source anti-D for their clinics sent patients to local hospitals, with one participant explaining that patients chose not to receive anti-D as a result of long waiting times. Others found local hospital referrals quick. Some discussed ceasing anti-D provision because of its sourcing difficulties:
[O]ther [international] guidelines don’t require anti-D. And I think if [we] move to not requiring anti-D, I think it will make things a bit easier. (P14)
Follow-up considerations
Methods of follow-up included in-person consultations, consultations with another GP or follow-up via telephone. Participants’ choices depended on the perceived risks of performing medical abortion, patient compliance and travel time. Most participants requested a quantitative human chorionic gonadotropin serum blood test showing a >80% drop from baseline and an in-clinic consultation for follow-up.
But I think from my perspective, I’m not as comfortable to say, ‘Don’t come back or just get a blood test done and you’re okay’ … I’d just rather see them. (P19)
When patients did not return for follow-up, several participants attempted contact through text messages, telephone calls and registered post.
Cost and time of provision
Few participants provided medical abortion via bulk billing, with most charging fees. Participants charged either gap fees per appointment (between $32 and $135 out of pocket) or one fee for all associated care involved in the medical abortion (between $120 and $295). Many offered bulk billing for follow-up appointments to incentivise patients to return.
Importantly, medical abortion was perceived as decreasing most participants’ earning power:
[I]t’s costly because it prevents me from seeing a higher number of patients in the same time frame that I am counselling patients about medical abortion. (P5)
However, one participant had an increased income, while others perceived no change to income, as medical abortion provision fitted into their pre-existing appointment schedule.
All participants used time-based item numbers to bill medical abortion, with most requiring 30-minute appointments for medical abortion counselling and medication provision, and 15-minute appointments for in-clinic follow-up. Some ‘maximised’ medical abortion billings by using time-based item numbers in conjunction with others, such as 4001 (non-directive unplanned pregnancy counselling).
Relationship building with patients
Most participants perceived their medical abortion service was acceptable to patients, although some had not received formal feedback. Participants reported that women were ‘relieved’ and ‘supported’, and that they appreciated the anonymity general practice provided. Some participants continued to see patients after medical abortion for contraception or unrelated appointments. If a patient had returned for ongoing care, participants felt they had provided an acceptable, high-quality service, particularly for rural patients:
[T]hey [patients] really appreciate being able to do it locally … I’ve got people that I’m still seeing a couple years later that have become my regular patient[s]. (P22, regional provider)
Three participants had dissatisfied patients. Dissatisfaction was related to the intensity of medical abortion side effects and appointment scheduling:
[I]’m not saying every patient [is] happy … they want the script then and then in the first appointment. I tell them ‘I’m not gonna give it’ … a lot of people stormed at me … (P2, Model 1 provider)
Discussion
This is the first Australian study to describe GP medical abortion delivery models aside from task-sharing. Although three main models (common, streamlined and ultrasonography-inclusive) are used, most participants used three appointments to provide medical abortion in general practice. Few GPs interviewed provided medical abortion care in 1–2 appointments, and fewer provided ultrasonography services to patients seeking medical abortion in-clinic, despite these models being more efficient than the common model. However, the use of ultrasonography-inclusive models may be difficult for medical abortion providers to establish as a result of initial costs, such as ultrasonography training and purchasing and certification of ultrasonography machine(s). Therefore, GPs wanting to provide medical abortion could consider adopting streamlined or common medical abortion delivery models to increase medical abortion accessibility to Australia women.
Although international7,21 and Australian22 data confirm that women find GP medical abortion generally acceptable, data from the present study suggest that streamlined and ultrasonography-inclusive GP medical abortion models may be more acceptable than the common model. Multiple appointments were perceived to cause dissatisfaction for some women. Additionally, women living in rural areas – who are likely to have poorer access to abortion services – may prefer optional, telephone or proximal GP follow-up. With the minority of participants providing streamlined, ultrasonography-inclusive models or optional follow-up, increasing the availability of these models may better align with acceptable medical abortion delivery in general practice as well.
Despite the World Health Organization determining ultrasonography non-essential for medical abortion eligibility (following clinical assessment and other investigations), the present findings are consistent with other developed countries’ practices, where standard medical abortion protocol requires ultrasonography.16,23 Current Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) guidelines recommend ultrasonographical examination as mandatory prior to abortion, rather than non-mandatory,24 despite the fact that some women who live in rural areas find ultrasonography difficult to access.2 Additional support for GPs to provide ultrasonography-inclusive models, particularly in rural areas, could alleviate ultrasonography-related delays for medical abortion provision.
With one in 10 Australian women unsure of where to access abortion services,3 advertising the location of available services can significantly affect medical abortion accessibility. Surprisingly, only two participants disclosed providing clandestine abortions as a result of stigmatisation fears. Although fear of stigma is a commonly reported barrier to abortion provision,12,14,25 very few participants voiced concern about being stigmatised. Provision of specific advertising platforms (eg 1800myoptions) for medical abortion provision may attenuate stigmatisation fears. Expansion of the 1800myoptions telephone and online services – which provide information as to where providers of medical abortion are practising, from Victoria only to nationwide – may also improve accessibility.
The present findings show that the cost of medical abortion is not standardised. However, the highest cost for medical abortion ($295, excluding medication cost) was significantly lower than the median fee within a group of specialised Australian clinics ($560).3 While bulk-billed medical abortion models exist,16 the rarity of bulk billing among participants may be due to the majority working in private services rather than funded facilities such as the one described by Tomnay et al.16 As is the case internationally, cost can be a significant barrier for women.26 Additional costs such as ultrasonography, medication and travel to multiple appointments can increase the financial burden of medical abortion.3 Cost-reduction strategies such as using bulk-billing ultrasonography providers or minimising ultrasonography use (where safe)27 were used inconsistently by participants. These strategies should be considered to improve the appropriateness of medical abortion services. However, with no specific remuneration for GPs providing medical abortion, the cost of medical abortion may continue to be variable between providers. It may be unaffordable and thus inaccessible to some Australian women.
The present findings show that GPs prefer in-clinic medical abortion follow-up, despite follow-up via telephone or self-reported outcome being safe.28,29 Preference for in-clinic follow-up reflects concerns that patients might not be able to rely on the unconditional support of the public system in the albeit rare event of complications. Whether participants had knowledge of the safety of alternative methods of follow-up is unclear. The recent introduction of telehealth as a result of COVID-19 may change this.Additionally, with no nationwide medical abortion guidelines currently available, variation was found between participants’ medical abortion delivery, particularly with follow-up method. Indeed, all phases of medical abortion may be transitioned to telehealth delivery. Translation of Queensland’s guidelines30 for all of Australia, or adoption of the new National Institute for Health and Care Excellence (NICE) guidelines27 into a succinct, GP-focused guideline, may assist GPs to deliver medical abortion more efficiently, acceptably and accessibly in Australia.
The present study is consistent with Dawson et al,15 who suggest that strong networks, especially with other medical abortion providers, create effective service. Participants networked with other medical abortion providers using a private Facebook group, which is essentially an informal community of practice (CoP)31 because of the shared interest, shared resources and collaborative nature. However, given the private nature of this group, a formal CoP endorsed by government and peak bodies may be more advantageous to support current and future provision of safe medical abortion.
The large sample size (n = 25) and recruitment from six states and territories is a strength of the present study. Additionally, two coders were used to analyse results, adding further rigour to the validity of the results. Although participants were largely recruited though a single private Facebook group, which could overemphasise this group’s importance in the results, the researchers were still able to recruit a geographically diverse sample. As a result of legislative differences and availability of anti-D depending on location, subgroup analyses of participants from different states, territories and remoteness areas may have been preferable; however, this was not possible because of small numbers within some subgroups. Furthermore, although the authors have described acceptability of GP medical abortion models, acceptability should be ascertained by interviewing women who have had GP medical abortion rather than the GPs providing medical abortion.
Conclusion
This study focused on three models for delivering medical abortion currently used by GP medical abortion providers: common, streamlined and ultrasonography-inclusive. Although most participants used the common model, it may be beneficial for providers to focus on GP medical abortion models that are more efficient and acceptable such as streamlined or ultrasonography-inclusive, although ultrasonography-inclusive models may be more difficult because of costs and training requirements. Additionally, follow-up methods that do not require in-person attendance may be more acceptable and help make medical abortion more accessible to Australian women. The development of a CoP platform endorsed by discipline peak bodies and government, and creation of national guidelines, can further support medical abortion providers and could encourage GP medical abortion provision. These strategies are needed to promote higher quality abortion care in Australian general practice.
Implications for general practice
- Medical abortion models of care that limit the number of consultations required in general practice are feasible and guideline concordant.
- GPs wishing to commence medical abortion delivery are advised to consider establishing a network of supportive health professionals to facilitate medical abortion delivery, communicating to colleagues in their workplace their intent to provide the service, advertising the service to their patients and forming or joining a network of current providers for support, education and advice.
- The creation of a more accessible CoP supported by government and endorsed by discipline peak bodies may improve the safety and effectiveness of medical abortion, and provide support for future and current GP medical abortion providers.
Appendix 1