Case
A man aged 53 years presented to a general practitioner (GP) with a 1–2-month history of a rapidly increasing skin growth on his right medial ankle. It had become tender and bled readily on contact. He had a history of right leg venous insufficiency, with three previous venous ulcers in the same location as the new skin lesion. The venous insufficiency was being managed with a class 2 compression stocking. He had no history of skin cancer. On examination there was a 3.5 cm × 3.5 cm exophytic, friable skin growth with a crusted rim over his right medial malleolus (Figure 1). His leg showed chronic changes of venous insufficiency. There was no palpable lymphadenopathy of the affected leg and groin, and no palpable hepatosplenomegaly.

Figure 1. The skin growth
Question 1
What is the likely diagnosis?
Answer 1
The likely diagnosis is squamous cell carcinoma arising from a scar (Marjolin ulcer). Other possibilities to consider could include alternate cutaneous cancer subtypes such as basal cell carcinoma; and pseudoepitheliomatous hyperplasia. The differential diagnosis for chronic ulcers includes venous ulcers, arterial ulcers, diabetic ulcers, pyoderma gangrenosum and systemic factors inhibiting wound healing such as malnutrition, smoking, corticosteroids and immunosuppressants.
Question 2
What is a Marjolin ulcer?
Question 3
What are the risk factors for developing a Marjolin ulcer?
Question 4
What features on history and examination raise suspicion for Marjolin ulcer?
Question 5
What are the options for biopsy?
Answer 2
A Marjolin ulcer refers to a cutaneous malignancy, usually a well-differentiated squamous cell carcinoma, developed within a pre-existing scar or ulcer. Marjolin ulcers are a recognised complication of chronic venous ulcers.1
Answer 3
A Marjolin ulcer is three times more likely to be diagnosed in men than women, and the average age at diagnosis is within the fifth decade.2 It is more common on the lower limbs. A Marjolin ulcer most commonly develops within an old burn scar, but can also develop from within any prior skin trauma such as traumatic scars, venous ulcers, pressure sores and osteomyelitic fistulae. The average period from scar acquisition to malignant degeneration is 36 years.3
Answer 4
The first scenario is a wound or ulcer developing features such as increasing pain, contact bleeding, increasing size, failure to heal, foul smell, rolled edges and indurated edges. The second scenario is the development of a growth, ulcer or induration within a scar.
Answer 5
A punch, shave or excisional biopsy is recommended for cutaneous squamous cell carcinoma.4 The choice of biopsy technique will depend on the lesion characteristics and the clinician’s preference. A punch or piece-of-pie biopsy of an affected border may be a starting point. Performing an appropriate and adequate biopsy will prevent delay of diagnosis and treatment. Discrepancy between the clinical diagnosis and the pathology result should prompt discussion with the pathologist, further biopsy or referral.5
Case continued
The GP took a partial shave biopsy for histopathology, which reported a well-differentiated squamoproliferative lesion with suspicion for well-differentiated squamous cell carcinoma
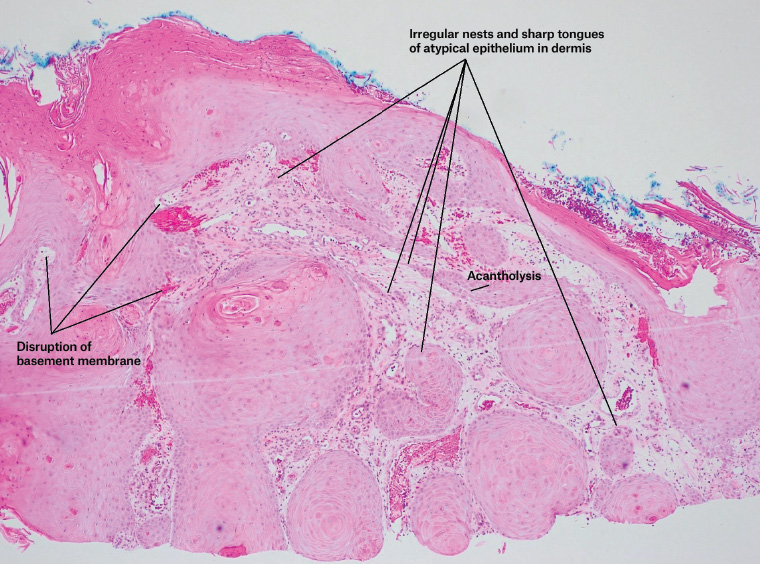
Figure 2. Superficial tissue fragments show a well-differentiated squamoproliferative lesion, suspicious for well-differentiated squamous cell carcinoma, arising within a background of severely solar-damaged skin with vascular changes associated with venous eczema. The lesion, as seen on this micrograph, shows mild cytological atypia, focal acantholysis and disruption of the basement membrane. Irregular, sharp-edged tongues of epithelium extend through the superficial dermis, together with small irregular nests of squamous epithelium. The latter occasionally display paradoxical maturation and keratinisation.
Question 6
How should a Marjolin ulcer be managed?
Answer 6
A Marjolin ulcer is frequently managed with wide local excision and skin grafting. Mohs surgery, flaps, and amputation may also be appropriate. Aggressive excision is advocated, as Marjolin ulcer skin cancers are more aggressive and have higher rates of recurrence and metastasis.6 Evidence of lymph node involvement should prompt lymph node biopsy. In the absence of this, the benefit of routine sentinel lymph node biopsy for high-risk cutaneous squamous cell carcinoma is to be determined.7 Close monitoring is recommended, but a consensus has not been reached regarding specific follow-up after treatment of Marjolin ulcers. Similarly, there is no guideline for monitoring after treatment of non-melanoma skin cancer.8
Case continued
The patient was referred to a general surgeon, who performed a wide local excision and a split skin graft (Figure 3). The complete excision specimen confirmed a well-differentiated squamous cell carcinoma invading to the deep reticular dermis. Margins were clear, and there was no perineural or lymphovascular infiltration.

Figure 3. Four months after the wide local excision and split skin graft
The patient had an uncomplicated recovery and underwent monitoring for local and regional recurrence. The patient was advised to have a three-monthly clinical examination for the first year, a six-monthly examination for the second and third years, and annually thereafter.
Key points
- A Marjolin ulcer should be considered when a patient presents with ulcers with suspicious features, or a growth or ulcer within a scar.
- Discrepancy between the clinical diagnosis and the pathology result should prompt discussion with the pathologist, further biopsy or referral.
- Marjolin ulcers require monitoring for recurrence and metastasis.
-