Measles cases are increasing globally, with more than 429,000 confirmed cases and approximately 679,000 additional suspected cases reported to disease surveillance systems worldwide during 2019.1 According to the World Health Organization (WHO), more measles cases were reported worldwide during the first half of 2019 than in any year since 2006.2 The WHO regions with the highest increases in reported cases included Africa (900% increase), the Western Pacific (230% increase) and Europe (150%).2 With the number of measles cases globally, Australia’s popularity as a tourist destination and a large population of frequent travellers, there is a constant threat of imported cases of measles entering Australia.
The re-establishment of measles transmission in several countries where it was previously eliminated, including four in Europe (Albania, Czechia, Greece and the UK), comes as a wake-up call to countries such as Australia.3 The UK lost their measles elimination status in August 2019 following a marked increase in cases across England and Wales during 2018 and sustained local transmission.4 In 2016, the WHO region of the Americas was the first region (as a whole) declared to have eliminated measles. Re-establishment of the disease in Venezuela and Brazil, following ongoing transmission for more than 12 months, has resulted in the region’s loss of this status.5 In 2019, the USA narrowly missed losing its elimination status, following its largest measles outbreak since it achieved elimination in 2000. This underscores that while measles elimination is hard won, it can be easily lost.
In 2019, one of Australia’s closest neighbours, New Zealand, recorded its largest measles outbreak in over two decades. The Auckland region had 1735 confirmed measles cases from the start of January 2019 to 15 January 2020.6 There has been a higher proportion of hospitalised cases during the Auckland outbreak (35–40%, in comparison to the 10% expected) and a higher than expected rate of complications among those hospitalised (three cases of encephalitis, 65 cases of pneumonia and five pregnant women hospitalised with measles infection, including two fetal losses associated with these cases).7 Hospitalisations and complications have mainly been reported among children aged <4 years.7
The severity of cases and outcomes seen in the Auckland outbreak supports the rationale for the high priority placed on public health response actions in the control of measles. It emphasises the need for timely diagnosis and reporting of suspected cases to disease surveillance systems by clinicians.
Since October 2019, measles outbreaks have also been reported by the respective Ministries of Health in Samoa, Tonga and Fiji.8–10 A state of emergency was in place in Samoa between 15 November and 28 December 2019, where over 5700 cases have been reported and 83 deaths have occurred (as of 20 January 2020), mainly of small children and infants.11 The Auckland and Pacific Island outbreaks are of particular importance to Australia, given the large population of New Zealanders and Pacific Islanders who regularly travel between these countries and Australia, potentially bringing the infection into Australia with them.12 Considering the widespread distribution and the high incidence of measles cases reported globally in 2019, only a handful of cases are needed to spark a large outbreak that could threaten Australia’s measles elimination status.
Measles in the Australian context
In Australia, there were 286 cases of measles notified in 2019, almost three times as many as in 2018. New South Wales (NSW) recorded 62 of these cases occurring in their residents, with a further nine people from other states, territories or countries having spent time in NSW while infectious during this period.
Forty-seven per cent of measles cases in NSW, and 50% of national cases, occurred in people born between 1966 and 1994. A further 27–29% occurred in people aged 15–24 years. Eleven percent of cases nationally and 13% of cases in NSW occurred in children aged 0–4 years. In NSW, all but one of these cases occurred in babies under 12 months of age.13,14
In NSW, two-thirds of patients with measles were unvaccinated (n = 21) or had an unknown or undocumented vaccination history (n = 17). A further 11% of cases occurred in people who were inadequately vaccinated. Of the unvaccinated patients, one-third were unable to be vaccinated prior to exposure because of their age on the basis of recommendations at the time.
Fifty-eight percent of the 2019 NSW cases acquired their infection overseas (imported cases), with five importations resulting from outbreaks in New Zealand, and two from Samoa. Of the 20 patients who acquired their infection in NSW (local cases) up to the end of November 2019, 70% have been linked epidemiologically and by nucleotide sequencing to cases imported from overseas (import related). Despite a larger proportion of locally acquired cases when compared with recent years, rapid public health action undertaken by NSW public health units and high vaccine coverage has limited ongoing transmission to tertiary spread.
The role of general practitioners in combating measles
General practitioners (GPs) have an important part to play in both the prevention and early detection of measles cases (Box 1). The Australian Government Department of Health15 as well as State and Territory health departments16–18 have guidelines for the diagnosis and management of measles. A current campaign by NSW Health urges travellers to ‘bring back memories, not measles’ (Figure 1). Largely delivered through social media, the campaign encourages travellers to ensure they are fully protected against measles prior to overseas travel, and more recently has included New Zealand– and Pacific Island–specific references. The campaign links to the updated NSW Health measles website, which provides audience-targeted information for travellers, medical providers and the general public, as well as current measles alerts for NSW and links to information on measles internationally.18
| Box 1. The role of general practitioners in combating measles |
Prevention
Patients travelling overseas need to be assessed to ensure they are up to date with their immunisations. Those born during 1966 or later require two doses of a measles-containing vaccine to confer lifelong immunity. Note that Australian-born patients born between 1966 and 1994 may have missed one or both doses because of changes to the immunisation schedule in this period.
It is important to determine the measles immunisation status of overseas-born patients who may not have received two doses of a measles-containing vaccine.
It is safe to give another dose of measles-containing vaccine to patients unsure of their immunisation status, provided there are no contraindications. Alternatively, patients who are uncertain about their vaccination status can have their measles serology (immunoglobulin G) checked.
Children aged 6–12 months can receive a measles, mumps and rubella (MMR) vaccine early if travelling overseas to a country with known measles cases.
Early detection
A high index of suspicion needs to be maintained for measles in recently returned travellers with a febrile illness, particularly when they have travelled to a country with known measles cases, and in anyone with a fever and a maculopapular rash.
If measles is suspected, it is important to isolate the patient and notify the local public health unit immediately, as they can provide advice regarding testing. |
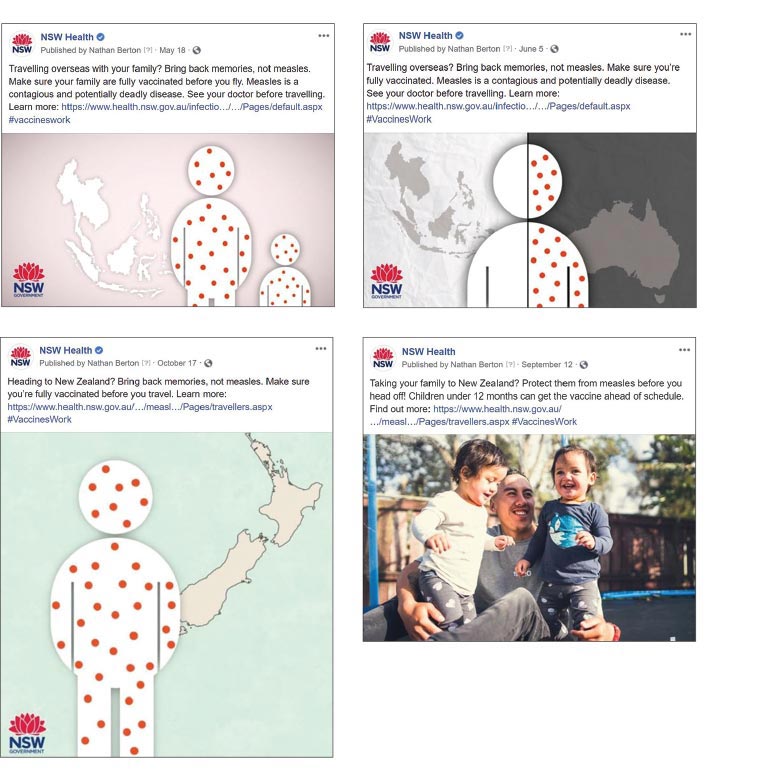
Figure 1. Social media posts for NSW Health’s ‘bring back memories, not measles’ Facebook campaign
The Australian Academy of Science, in partnership with the Australian Government Department of Health, has developed ‘measles: everything you need to know’, which contains information and videos targeting specific audiences including travellers and health professionals at a national level.19
Measles elimination status is hard won. In this age of regular international travel, a single imported case could be enough to spark a large outbreak among those not immunised or under-immunised, which could threaten this achievement. Localised outbreaks currently occur in Australia as a result of imported cases, but because of effective public health and primary care actions, these outbreaks have not resulted in ongoing sustained local transmission that has threatened Australia’s elimination status. However, given the current global context, heightened vigilance is essential for early detection and management of any imported measles cases.