Flat feet are relatively common in childhood, affecting up to 14% of children.1 Flexible flat feet can be part of an otherwise normal developmental profile, and foot arches usually develop with age; however, there is a wide range of normal variation.1–5
Paediatric flat foot (pes planus) treatment is a somewhat controversial topic, with a lack of clarity in the literature regarding which children require treatment, as well as the efficacy of intervention.2,6,7 However, there is increasing evidence that non-surgical interventions, such as orthoses and physiotherapy, may be beneficial for certain groups of children.6,8
The goal is not usually to permanently reverse the changes in the foot and ankle, but rather to help limit progression of the deformity and reduce the rate of chronic, secondary complications up the kinetic chain.
Anatomy and pathology of the foot
The foot is the complex ‘terminal organ’ of weight bearing and locomotion. There are 26 bones and 33 joints in the human foot and ankle, controlled and stabilised by multiple muscles, tendons and ligaments. The foot can be sub-divided into the hindfoot, midfoot and forefoot. The cuboid, navicular and three cuneiform bones help form the two longitudinal arches and single transverse arch of each foot (Figure 1). The elasticity of these arches makes walking and running more efficient in terms of energy consumption, as well as dissipating much of the force incurred in locomotion before it reaches the more proximal lower limb.9
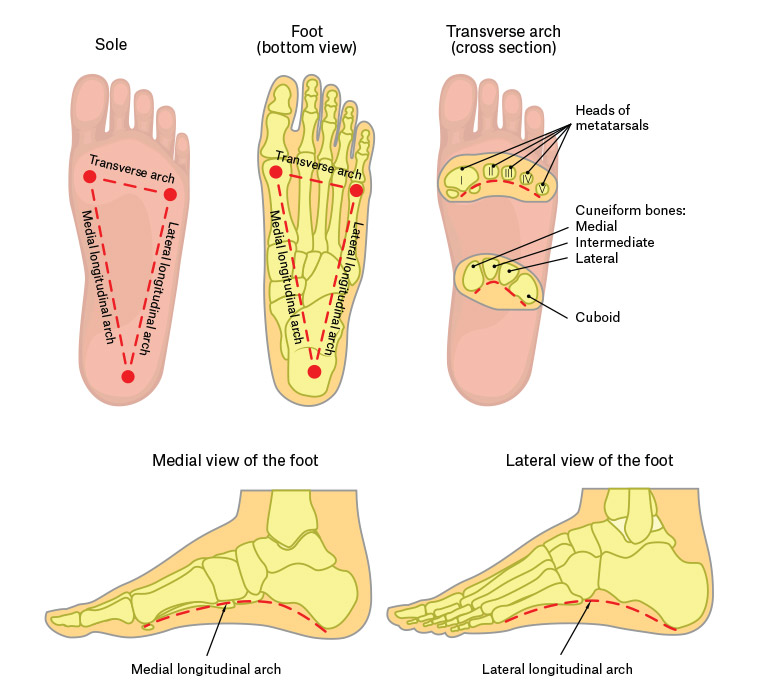
Figure 1. Arches of the foot
Pes planus results in flattening of the medial longitudinal arch (MLA), with secondary effects including medial navicular prominence, hind foot eversion, secondary hallux valgus and crowding of the lesser toes. There may be stretching of the plantar calcaneonavicular ligament (spring ligament) and the tibialis posterior tendon.2,10,11
Pes planus may occur as an isolated disorder or as part of a broader syndrome, particularly if the individual has low muscle tone or ligamentous laxity, with joint hypermobility.4,12
Other contributory factors may be tendo-Achilles shortening or tibialis posterior dysfunction. When pes planus is associated with underlying pathology – such as ligamentous laxity, genetic conditions and muscle imbalance – intervention is generally supported.1,4,5,12 Pes planus in children with underlying pathology has been shown to be associated with significant and measurable gait abnormalities.13
Clinical classification divides pes planus into either rigid or flexible depending on the mobility of the subtalar and other tarsal joints.1,4,7,14 Most mild, flexible pes planus is asymptomatic and does not require any intervention. Some flexible flat feet may cause localised fatigue and pain, with a secondary reduction in mobility, play and athletic performance. Additionally, chronic, untreated or undertreated pes planus may produce unwanted long-term sequelae up the kinetic chain, with secondary ankle, knee, hip and even lumbar pathology. However, there is currently no strong evidence that early, sustained orthotic intervention mitigates or prevents such complications.2,3,6,10,14
It is important to note that the foot is a dynamic ‘organ’ that develops and changes throughout infancy and childhood. ‘Pseudo’ flat feet are often observed in children aged under five years, secondary to the presence of a physiological fat pad occupying the MLA. This does not require treatment.2,4,5,15 Most children develop arches as they grow, while others show relentless progression of their foot and ankle deformities, despite timely and appropriate treatment.1,2
A wide range of disciplines may be involved in the assessment and management of flat feet including GPs, rehabilitation physicians, paediatricians, rheumatologists, orthopaedic surgeons, sports medicine physicians, podiatrists, orthotists, physiotherapists and exercise physiologists.1,15
Assessment
History-taking for paediatric pes planus includes:
- major motor milestones, such as the age at which the child first stood and walked
- the child’s falls history in comparison to age-matched siblings or peers
- pain in the feet or legs, particularly when walking longer distances, or playing sport
- easy fatigability in the foot and ankle region
- higher level mobility task ability, such as running, jumping and hopping
- previous use of orthoses, including the child’s compliance and the effectiveness of the orthoses
- the presence of significant comorbidities, or syndromes, which may be related to the presenting problem
- family history of flat feet.
The physical examination should begin with an inspection of the outersole wear pattern of the shoes (provided they are not new shoes or worn infrequently; school shoes are usually a good option). The physiological wear pattern should be around the posterolateral heel, as this represents the area of initial ground contact at heel strike during the normal gait cycle. However, a child with pes planus may display a posteromedial heel wear pattern.
The feet should also be examined, looking for hallux valgus secondary to foot pronation, which may in turn produce crowding of the lesser toes, with underriding and overriding toes. It is important to assess the volar surface of the feet and look for abnormal, chronic pressure areas, evidenced by callosities.
The stance and gait pattern should then be analysed, first with footwear and then barefoot. It is important that the examination includes inspection anteriorly, posteriorly and laterally; both while standing and during walking. Particular attention should be paid to evaluation of heel valgus, the foot progression angle and any rotational deformity.2,10,12,14
When observing the child from behind while they are standing, note the angle of the Achilles tendon near the insertion, as well as calcaneal alignment. The Achilles tendon may have a valgus angulation as it approaches the calcaneal insertion, rather than being vertical. Hyperpronation of the foot can be demonstrated with the ‘too many toes’ sign. Usually the fifth digit and some of the fourth digit can be seen laterally when viewing the foot from behind; visibility of more toes indicates abduction and external rotation of the foot, which occurs with pes planus.10 There may be navicular prominence antero-inferior to the medial malleolus.
Pes planus is clinically classified as either flexible or rigid, with flexible flat foot accounting for approximately 95% of cases in children.1,2,4–7,10 Radiological confirmation is rarely required in uncomplicated cases.
If the MLA is flattened during loading at stance phase, but the patient forms a dynamic arch when standing up on their metatarsal heads, this indicates flexible flat foot and may benefit from orthotic use. If no dynamic arch forms, this indicates rigid flat foot, defined by restriction at the subtalar joint. It may be associated with an underlying neuromuscular or orthopaedic condition.2,3,14,15
The range of motion of the joints of the lower limb should be assessed, in particular active and passive dorsiflexion of the ankle.2,10,15
Of those with flexible pes planus, only a subset will benefit from intervention. Important considerations on assessment include symptoms such as pain and impaired gait and balance.2,4,6,8 Pain is a common symptom. Improvement in pain associated with flat feet may be seen with the use of foot orthoses.5,6,8,13 Balance has also been shown to improve with the use of foot orthoses.6,8 It is also important to consider the presence of underlying neurodevelopmental disorders and associated muscular hypotonia and ligamentous laxity, as children with these conditions more commonly require physiotherapy, orthotic intervention and closer follow-up.2,12
General management
The merit of treatment for all flexible flat feet remains equivocal; however, there is increasing evidence that foot orthoses produce improvements in children with pes planus over multiple outcome measures.1,6,8,15 This ambiguity is partly due to the absence of a universally accepted classification system to allow specific measurement of improvement, together with a lack of high-level evidence for different treatment options.2–7,10 There is added confusion due to difficulty separating spontaneous physiological arch improvement from the effect of intervention.1,13 There is minimal evidence for treatment of asymptomatic, flexible, paediatric flat feet in a child with no underlying medical issues.2–4,6,10 Treatment of symptomatic, flexible flat feet is generally accepted for children with contributory background factors or secondary complications, or if pes planus persists past childhood.6–8,11 There is evidence that symptoms related to pes planus, particularly pain, improve with non-surgical interventions.1,5,6,8,13
Quality footwear may be sufficient for mild cases; however, shoes generally offer more protection than correction. Ideally, the child should be fitted with a flat, lace-up shoe with a firm heel counter and MLA support, a broad and deep toe box and the ‘toe break’ at the junction between the anterior third and posterior two-thirds of the shoe (when the shoe is compressed, toe to heel, between the palms).
Physiotherapy
In addition to optimisation of footwear, with or without orthoses, management includes physiotherapy to improve the strength of the extrinsic and intrinsic foot musculature. As part of the assessment process, the physiotherapist can assist in evaluating the gait, gross motor skills and the impact the foot deformity has on functional activities.2,10 Physiotherapists also assess endurance, speed, fatigability, pain and ability to walk on different terrains, with a focus on assessing function, not just structural abnormalities.6,8 The physiotherapist can suggest an exercise program to increase strength in the muscles that stabilise the arches. Specific exercises include: walking up on the metatarsal heads (‘tip-toes’), walking on the heels, activities to improve the dynamic arch such as walking barefoot on soft sand, flexing the toes (eg picking up a tissue with the toes), rolling a ball under the arch of the foot while sitting, pretend piano playing with the toes, great toe dorsiflexion, and encouraging climbing and other gross motor activities.1,4 The recommended exercises are modified depending on the child’s and family’s needs. Exercise programs are more effective if they are family-centred and involve games and activities that can be incorporated into the child’s day.
Orthoses
There are a large range of orthoses that are used for flexible flat feet. The prescribing team tends to move up the hierarchy from the least to most supportive as the severity of pes planus increases. Options are summarised in Table 1.

Prescribed foot orthoses should be ‘worn-in’ slowly, starting with 1–2 hours of use per day, as tolerated, for the first week and gradually increasing the number of hours over an approximately 2–3-week period. Review by the orthotist and prescribing doctor is then required to assess the adequacy of correction provided by the orthoses, exclude pressure areas and adjust the orthoses as needed. Reviews should be performed every 6–12 months to reassess fit and evaluate whether the child still requires the orthoses. The child will require larger foot orthoses each time their shoe size increases.
Applications for funding of orthoses through government programs, such as the National Disability Insurance Scheme (NDIS; the current Australian Federal Government program providing funding for equipment and services for people with disability aged <65 years), require measurable functional goals to be included.
Conclusion
While debate remains in the literature as to the utility of orthotic management of paediatric pes planus, intervention should be considered, particularly for a child with symptoms or moderate-to-severe changes in the feet. The goal is not to reverse the changes but rather to help limit progression of the deformity and reduce the rate of chronic, secondary complications.
Use of the diagnostic and treatment guidelines outlined in this article may assist the GP to manage paediatric pes planus, and help guide referral to a multidisciplinary clinic as required.