Case
A woman aged 30 years presented with a six-month history of an expanding plaque on the right superior shin. The plaque was associated with mild itch and tenderness. It had an indurated periphery.
Her only medications were mirtazapine and venlafaxine. Her systems review was unremarkable. A recent ultrasound reported non-specific subcutaneous changes with no clarification on aetiology.
Question 1
How would you describe the lesion in Figure 1?

Figure 1. Photograph of the patient’s right anterior shin
Question 2
What is your differential diagnosis?
Question 3
What investigation(s) would you perform?
Answer 1
There is a single annular plaque on the right anterior superior shin with an erythematous periphery and central clearing. There are no secondary changes such as scale or crusting.
Answer 2
As the lesion is strikingly annular, granuloma annulare and tinea should be considered. However, the clinical features of ill-defined erythema and palpable induration taken together with the ultrasound result indicate a process affecting the subcutis.
Granuloma annulare, although annular, is a dermal process that produces a typical beaded edge on palpation. Similarly, tinea typically produces superficial inflammation with a scaling erythematous margin and central clearing. Induration and evidence of subcutis inflammation would be inconsistent with either diagnosis.
Pretibial myxedema, sarcoidosis and infective cellulitis should also be considered; however, the patient had no other comorbidities and was otherwise well.
The provisional diagnosis is thus a subcutaneous inflammatory condition. A common panniculitis of the pretibial area is erythema nodosum, which usually presents as a nodule.
Answer 3
As the working diagnosis is thought to be confined to the subcutaneous layer, biopsies should be performed to include a substantial amount of fat.1,2
Case continued
The patient’s elliptical biopsy showed dermis-sparing, septal panniculitis with lymphohistiocytic cells and scanty neutrophils, without necrotising vasculitis – consistent with a rare presentation of erythema nodosum (Figure 2).
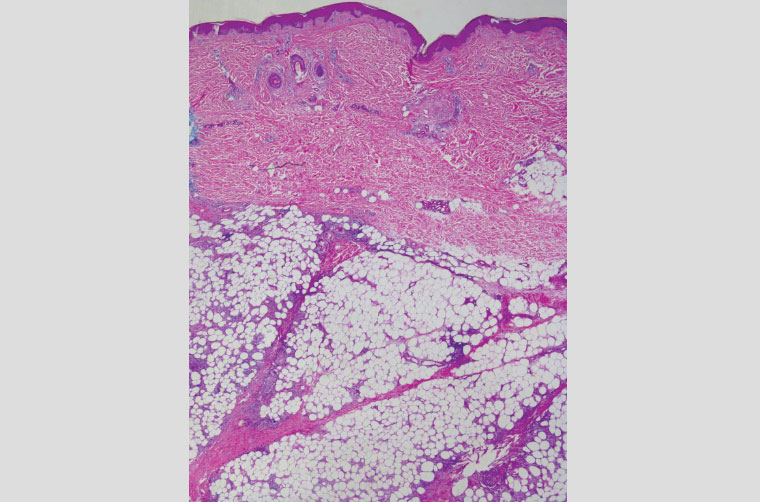
Figure 2. Microphotograph of the biopsy, showing a panniculitis that predominantly involves thickened septae with spilling of inflammatory cells into the fat lobules. The dermis is predominantly spared.
Question 4
What would be your further management?
Answer 4
Erythema nodosum is a cutaneous reaction pattern with a range of documented triggers.3 These include infectious, medication-related and inflammatory conditions (Table 1).
| Table 1. Common triggers of erythema nodosum |
| Infectious |
Medication-related |
Inflammatory |
Other |
- Streptococcus spp.
- Primary tuberculosis
- Yersinia spp.
- Chlamydia spp.
- Viral (eg human immunodeficiency virus, herpes simplex virus)
- Parasitic (eg histoplasmosis)
- Fungal (eg coccidioidomycosis)
|
- Sulphonamides
- Amoxicillin
- Contraceptive pills
- Nonsteroidal anti-inflammatory drugs
- Bromides
- Salicylates
|
- Inflammatory bowel disease
- Sarcoidosis
- Malignancies
- Leukaemia
- Lymphoma
- Behçet’s disease
|
|
A thorough history and clinical examination should be conducted to exclude these associations. The range of investigations to be performed will be guided by findings from the history and examination (Table 2). In just over half of all cases, no cause is identified.4
| Table 2. Investigations for erythema nodosum |
| Blood tests |
Other investigations to consider |
Baseline
- Full blood examination
- Elevated liver function tests
- Erythrocyte sedimentation rate/C‑reactive protein
|
Based on clinical suspicion
- Antinuclear antibody
- Serologies/antibodies:
- Hepatitis B/hepatitis C
- Antistreptolysin O titre
- Anti-DNase
- Campylobacter spp.
- Yersinia spp.
- Acid-fast bacilli
- Others
- Beta-human chorionic gonadotropin
|
- Chest X-ray
- Computed tomography scans
- Colonoscopy
- Endoscopy
|
Case continued
The results of the patient’s full blood examination, metabolic panel and inflammatory markers were normal, and her serology results were negative.
Question 5
How is this presentation different to typical erythema nodosum?
Question 6
What is the usual clinical course of erythema nodosum, and how would you manage this patient?
Answer 5
Classically, erythema nodosum presents with bilateral tender erythematous subcutaneous nodules, usually on anterior lower legs, knees and arms, although rarely they can present on the face and neck. The nodules are initially bright to deep red. They fade to leave bruise-like areas and hyperpigmentation. Arthralgia with swollen ankles and fevers can also be associated.5
In contrast, the patient had no palpable erythematous nodules but instead had a single plaque and no associated systemic symptoms. This annular plaque presentation is unusual and has only been previously reported in one other case, whereby the patient had a single lesion spreading centrifugally on her left thigh.6
Another atypical feature of erythema nodosum demonstrated in this case is the unilateral disease process, although this has been described previously in the literature.6,7
Answer 6
Erythema nodosum usually follows a benign and self-limiting course, but any identified underlying trigger should be addressed (eg stopping a precipitating medication or treating an underlying infection).8 Most cases resolve spontaneously within days to weeks, although relapses can occur in one-third of cases. For these patients, erythema nodosum may become a chronic or persistent issue. It should also be noted that a rare complication of erythema nodosum is encapsulated fat necrosis (mobile encapsulated lipoma).9
In terms of treatment, non-pharmacologic management options for pain include rest and venous compression therapies. Analgesia including nonsteroidal anti-inflammatory drugs and colchicine can be used.8
Once any underlying infection has been treated and malignancies have been ruled out, systemic corticosteroids may also be considered.10
Key points
- Erythema nodosum is usually a benign condition; however, underlying triggers must be ruled out.
- Erythema nodosum usually presents with multiple tender erythematous nodules on the anterior shins but can occur on the upper limbs, neck and face.
- The annular presentation is unusual and should be included in differential diagnosis for annular plaques on legs.
- The type of biopsy performed should target the underlying pathology. A superficial biopsy in this case would have been unrepresentative.
- Management is predominantly symptomatic, and most patients have complete resolution.