Renal tract pain is a common presentation to a general practitioner (GP) or emergency department, accounting for approximately 75% of presentations due to disorders of the genitourinary system.1 Ureteric calculi causing obstruction are among the most commonly identifiable causes. One in 10 Australians will have kidney stones in their lifetime.2 Recurrence of renal stones within five years approaches 50%;2 however, 75–90% of renal calculi pass spontaneously without intervention.3
The aim of this article is to present current evidence-based recommendations for the acute management of renal colic. Its pathophysiology, investigations, diagnosis and therapeutic options are important considerations for GPs in the acute setting.
Discussion
Renal tract pain can be caused by acute ureteric obstruction, pedicle traction or stretching/compression of the peripelvic renal capsule or renal pelvis.4 Severity of renal colic is associated with acuity rather than degree of obstruction.5
Renal colic occurs in predictable phases, reaching maximum intensity in 30–120 minutes and usually lasting for 3–18 hours.
The three phases are:
- acute – insidious, constant, intermittent exacerbations that crescendo up to six hours
- constant – sustained maximal pain intensity, lasting 1–4 hours
- relief – gradual diminishment, lasting 1–3 hours.
To understand renal tract pain, two concepts must be explored – the migratory nature of renal tract pain, and referred pain.
Sensory innervation over the entire length of the ureter is fed back to the sympathetic autonomic nervous system through T10-L2.6 Renal colic pain is migratory depending on the location of the offending calculus, resulting in the classic ‘loin to groin’ pain. When a renal calculus advances into the ureter, ureteric spasms occur secondary to a massive release of prostaglandins.7 Renal stones in the upper two-thirds of the ureter tend to present with flank and renal angle tenderness. As they progress into the distal third of the ureter, patients tend to experience pain in the groin, labia/scrotum or perineum. This may be associated with storage-related lower urinary tract symptoms (LUTS), such as urinary frequency, urgency, nocturia and incontinence.8 None of the aforementioned symptoms reliably predicts the location of the offending stone in the ureter.
Referred pain is pain perceived by the body at a location other than the site of the painful stimulus.9 General visceral afferent pain fibres travel with sympathetic fibres back to the spinal cord segments that gave rise to the preganglionic sympathetic fibres.10 This is difficult to distinguish from pain travelling along dermatomes that occupy the same spinal root segment dorsal ganglia. Given their varied presentations, various extra-urinary diseases can masquerade as ureteric disorders and vice versa. Table 1 lists some important causes and mimickers of renal tract pain.
| Table 1. Causes and mimickers of renal tract pain6 |
| Renal |
- Inflammation – pyelonephritis, renal/perinephric abscess
- Tumour – renal cell carcinoma
- Vascular – thrombosis, trauma
- Obstruction – renal calculi
|
| Ureter |
- Intrinsic – calculi, blood clot, papillary necrosis, stricture, malignancy (ureteric urothelial cancer, prostate adenocarcinoma invading ureter)
- Congenital – pelviureteric junction obstruction, vesicoureteric reflux
- Iatrogenic – instrumentation, trauma
- Extrinsic – lymphadenopathy/malignancy, retroperitoneal fibrosis
|
| Testis |
- Inflammation – epididymo-orchitis, testicular torsion, epididymal cyst infection, hydrocele
- Tumour – testicular cancer
- Vascular – varicocele
|
| Extra-urinary |
- Inflammation – appendicitis, cholecystitis, diverticulitis, pelvic inflammatory disease
- Vascular – aortic and iliac aneurysms
- Inguinal hernias, ovarian pathology, ectopic pregnancy
|
Assessment of renal tract pain
History-taking
History-taking is important as many factors predispose individuals to the formation of renal calculi, and it should include:
- personal or family history of renal stones
- known structural renal tract abnormalities – horseshoe, ectopic or medullary sponge kidneys; pelviureteric junction obstruction; polycystic kidney disease; pyelo-ureteral duplication11
- medical conditions – gout, hyperparathyroidism, renal tubular acidosis, osteoporosis, recurrent urinary tract infections
- medications – loop diuretics, carbonic anhydrase inhibitors, ciprofloxacin, sulfonamide-containing medications, indinavir12
- dehydration, high salt and protein intake.
Associated symptoms during examination can often help to distinguish one diagnosis from another. Haematuria is a common feature of ureteric calculi and is associated with approximately 82% of renal colic presentations.13 Nausea and vomiting as well as LUTS often accompany renal colic. Concomitant fevers might be indicative of other inflammatory or infective processes or signal the presence of an infected obstructed kidney, which is a urological emergency. A comprehensive examination of all abdominopelvic organ systems is essential to rule out other important life-threatening conditions. A diagnosis of renal colic does not exclude other concomitant medical conditions that may require more urgent attention.
Investigations
Bedside and laboratory tests for suspected renal colic patients should include the following:14
- urine dipstick analysis/urine culture
- beta human chorionic gonadotropin
- full blood examination
- C-reactive protein
- urea, electrolyte, creatinine.
In conjunction with individual patient (eg age, comorbidities, renal function) and disease (stone, duration) factors, these investigations are important in helping to identify a subset of patients who are not suitable for conservative management, especially if there are markedly raised inflammatory markers or severe renal failure in the absence of other infections/inflammatory conditions.
Diagnostic imaging is also important in the workup of renal tract pain (Figure 1). Immediate imaging is indicated in vulnerable patient populations (eg those with infective symptoms, a single kidney or severe renal failure).15 Low-dose, non-contrast computed tomography (CT) of the kidneys, ureters and bladder (KUB) is the current gold-standard imaging of choice and can readily identify stone location, size and density.16 It is also useful in diagnosing most mimickers within captured surrounding anatomy. A meta-analysis of non-contrast CT diagnoses of renal tract calculi has demonstrated a pooled sensitivity of 93.1% and specificity of 96.6%.17 In patients with a body mass index <30 kg/m2, sensitivity for detection of stones >3 mm in size is 100%.18
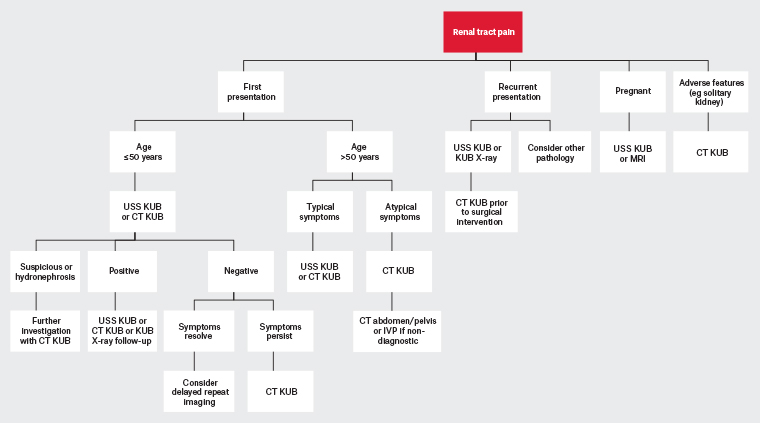
Figure 1. Diagnostic imaging pathway of renal tract pain.37 Click here to enlarge
CT, computed tomography; IVP, intravenous pyelogram; KUB, kidneys, ureters and bladder; MRI, magnetic resonance imaging; USS, ultrasonography
In younger individuals (ie those aged <50 years) and those more susceptible to radiation risk, such as pregnant women, KUB ultrasonography is a useful alternative first-line imaging tool to identify calculi present in the renal calyx, pelvis, proximal and distal ureter. KUB ultrasonography can also readily pick up hydroureter and hydronephrosis suggestive of a ureteral obstructive process.19 However, it is markedly less useful in identifying calculi in the mid ureter because of overlying bowel gas. KUB ultrasonography is also highly dependent on operator skill and patient factors such as body habitus. Overall, KUB ultrasonography is safe, reproducible and inexpensive, with acceptable calculi detection rates for both renal (sensitivity 45%, specificity 88%) and ureteric (sensitivity 45%, specificity 94%) calculi.19 When results are inconclusive, or in the event of persistent symptoms or ongoing suspicion of renal colic, a CT scan should be performed, especially if surgical intervention may be required.
Management of renal tract pain
Pain relief
Paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) have been shown to be effective in the treatment of renal colic and are superior to opioid medications in terms of analgesic efficacy.20 Less rescue analgesia is required for breakthrough pain or recurrent renal colic with the use of NSAIDs than with opioid medications.21 The current understanding of the mechanism behind this is that the increased release of prostaglandins secondary to ureteric obstruction promotes glomerular afferent arteriolar dilatation and increased vascular permeability.22 This leads to increased urine output from the affected kidney and higher renal pelvic pressure. NSAIDs exert their effect primarily by reducing prostaglandin production, thereby reducing the glomerular filtration rate by as much as 35%, thus reducing renal pelvic pressures and stimulation of stretch receptors.23,24 Ureteric oedema improves as well, enabling better drainage and reducing ureteric spasms. There is also some evidence that NSAIDs exert a direct effect on local ureteric smooth muscle, mediating relaxation.24
NSAIDs are also versatile, available in many formulations for rapid effect, such as oral, intravenous and per rectal formulations. Per rectal administration of NSAIDs may provide better symptomatic control as there is an increased local anti-inflammatory effect.25
NSAIDs can worsen acute renal failure in patients with underlying chronic renal failure when taken for renal colic and should be used with caution and for short periods of time only. In general, NSAIDs should be used at the lowest dose for the shortest period required to minimise NSAID-induced nephropathy.26
Opioid medications should be used as second-line analgesia if NSAIDs are contraindicated or insufficient in pain control. They tend to provide only short-term relief and require multiple dosing to achieve the desired effect. Opioid medications are also associated with a less favourable side-effect profile including nausea, vomiting, sedation, respiratory depression and constipation with increasing duration of use.27 Combination therapy of opioids with paracetamol and NSAIDs achieves synergistic effects, better pain control and fewer side effects through opioid sparing.27
Medical expulsive therapy
Medical expulsive therapy (MET) has been studied extensively to determine whether it reduces interval time for passage of stones if surgical intervention is not immediately indicated. This follows the discovery that ⍺-adrenergic receptors are present in high density along the distal ureter.28 Several medications have been trialled, including ⍺-blockers, calcium channel blockers, steroids and phosphodiesterase type 5 (PDE5) inhibitors.29 The theory was that medications that could relax ureteral smooth muscle without losing peristalsis or reduce ureteral oedema would hasten passage of stones into the bladder.
Tamsulosin has been shown to be superior to calcium channel blockers and PDE5 inhibitors in several small studies.30 Indeed, ⍺-blockers as a class have been evaluated in a meta-analysis and were found to increase rate of stone expulsion (risk ratio: 1.54, 95% confidence interval: 1.29, 1.85; P <0.01),30 reduce time to expulsion (P <0.01), reduce analgesia use and relieve renal colic (P <0.01).31 Tamsulosin, the most widely studied in the class, proved to be more efficacious for larger stones (>5 mm) and stones within the distal segment of the ureter that were amenable to conservative management.32 The most common reported side effect associated with the use of tamsulosin was transient postural hypotension (4.2%).33 A newer, more selective medication of the same class includes silodosin (⍺1A), while naftopidil (⍺1D) also shows great promise.34 Studies have been conducted using ⍺-blockers post–surgical intervention (eg laser lithotripsy and extracorporeal shock wave lithotripsy) to aid in passage of residual stone fragments with some success.35
Surgical intervention
Renal colic failing medical treatment, stones associated with anuria (eg single kidney or bilateral obstruction), acute renal failure or concomitant infection would require surgical decompression of the affected kidney(s). Options include cystoscopic retrograde stent insertion or nephrostomy tube insertion with or without antegrade stenting. There is no current good evidence to support one intervention over the other.36 If there is no evidence of infection, it is feasible to attempt a primary laser lithotripsy of the offending calculus, although success rates are lower with larger, more proximally situated calculi.3
Conclusion
Renal tract pain is a common presentation in the primary care setting. Accurate diagnosis and early initiation of adequate analgesia and medical expulsive therapy in appropriate patient groups can help improve quality of patient care and reduce emergency department presentations and healthcare costs.
Key points
- Renal tract pain is a common presentation in the primary care setting that can masquerade as other abdominopelvic conditions, and vice versa.
- Understanding the underlying pathophysiology will help in its diagnosis.
- Clinical assessment, blood tests and imaging should be included in the diagnostic process.
- Optimum management includes a combination of adequate analgesia and medical expulsive therapeutic options.
- A large percentage of renal calculi can be managed conservatively; surgical intervention is only required in the first instance when red flag symptoms are present.